Challenges of IYCF and psychosocial support in Lebanon
 By Juliette Seguin
By Juliette Seguin
Juliette Seguin is currently Health and Nutrition Coordinator for ACF Lebanon. She has been working with ACF since 2011 in Haiti, Guinea, Bangladesh, Turkey and Lebanon, managing nutrition projects on IYCF including mental health and care practices activities, CMAM, and Ministry of Health capacity building.
The author gratefully acknowledges the support of the Kayany Foundation, which enabled ACF to start nutrition activities in Lebanon, specifically in Aarsal. Thanks also to the ACF nutrition team in Lebanon for their work on the field and for sharing their experiences reflected in this article and to Anusara Singhkumarwong (ACF regional nutritionist) and Marisa Sanchez Peinado (ACF-Spain nutrition advisor) for their helpful review and comments.
Nutrition interventions targeting undernutrition are not common in many countries in the Middle East. Lebanon does not suffer from a high burden of undernutrition and is still categorised as a country in early nutrition transition, according to the WHO 2010-2019 strategy1. This categorisation is based on the fact that in Lebanon, there are moderate levels of undernutrition, overweight and obesity in certain demographic and other population sub-groups, as well as widespread micronutrient deficiencies. However, the Syrian crisis and the continuous influx of refugees into Lebanon have, after more than three years, brought attention to undernutrition in Lebanon.
 The preliminary results of a Joint Nutrition Assessment on Syrian Refugees undertaken at the end of 20132 (still under analysis) does not indicate an increase in the prevalence of acute malnutrition compared to the 2012 assessment results3. In the 2013 assessment, it is expected that the prevalence of acute malnutrition in the Bekaa Valley will be above the national average, as this is a region of the country particularly affected by the conflict in Syria due to its proximity to the border. Although the nutritional situation in Bekaa and other refugee impacted areas of Lebanon is not alarming, it is still a concern and remains one of the main priorities of the health sector. A number of stakeholders have therefore been working on programming to prevent deterioration of nutrition amongst Syrian refugees in Lebanon, as well as programmes to treat cases of acute malnutrition where these arise.
The preliminary results of a Joint Nutrition Assessment on Syrian Refugees undertaken at the end of 20132 (still under analysis) does not indicate an increase in the prevalence of acute malnutrition compared to the 2012 assessment results3. In the 2013 assessment, it is expected that the prevalence of acute malnutrition in the Bekaa Valley will be above the national average, as this is a region of the country particularly affected by the conflict in Syria due to its proximity to the border. Although the nutritional situation in Bekaa and other refugee impacted areas of Lebanon is not alarming, it is still a concern and remains one of the main priorities of the health sector. A number of stakeholders have therefore been working on programming to prevent deterioration of nutrition amongst Syrian refugees in Lebanon, as well as programmes to treat cases of acute malnutrition where these arise.
Prior to the crisis, a large proportion of Syrian caregivers was not practicing appropriate infant and young child feeding (IYCF). In 2009, according to the Syrian Family Health Survey, the national prevalence of exclusive breastfeeding amongst infants under 6 months was 42.6% while the proportion of newborns introduced to breastfeeding within the first hour of birth was 42.2%. The 2013 Joint Nutrition Assessment of the Syrian refugee population in Lebanon confirmed these practices and has raised more concerns about the nutritional situation of children under two years old in particular. This assessment found that only 25% of infants under 6 months of age were exclusively breastfed and only 64.7% of children were still breastfeeding at 1 year of age in Lebanon. By the age of 2 years, 70% of children were not breastfed (see Table 1).
Table 1: Infant and young child feeding practices in Lebanon (2013)*
Assessment area |
All Lebanon |
Bekaa |
|||
| N/Total | % (95%Cl) | N/Total | % (95%Cl) | ||
| Timely Initiation of Breastfeeding (First time to put child to the breast) | < 24 hours | 157/502 | 31.3% (27.37-35.45) | 31/102 | 30.4% (22.31-39.89) |
| 1-24 hours | 201/502 | 40.0% (35.85-44.39) | 34/102 | 33.3% (24.93-42.94) | |
| ≥ 24 hours | 144/502 | 28.7% (24.91-32.8) | 37/102 | 36.3% (27.6-45.95) | |
| Exclusive breastfeeding <6 months | 22/88 | 25.0% (17.13-34.96) | 4/16 | 25.0% (10.18-49.5) | |
| Continued breastfeeding at 1 year | 44/68 | 64.7% (52.85-75.0) | 9/12 | 75% (46.77-99.11) | |
| Continued breastfeeding at 2 year | 19/63 | 30.2% (20.24-42.36) | 4/12 | 33.3% (13.81-60.93) | |
*Preliminary results.
The health situation is also a concern with the potential for outbreaks of polio, measles, hepatitis and widespread waterborne diseases. At the end of May 2014, according to the Epi-Monitor Update of the Lebanon Ministry of Public Health (MoPH), several cases of acute flaccid paralysis, measles, viral hepatitis A and viral hepatitis B were reported among the Syrian population living in Lebanon4. These health threats could also have a significant adverse impact on the nutritional situation of the affected population. Living conditions in the Informal Tented Settlements (ITS) and the chronic nature of the crisis are also perceived by Action Contre la Faim (ACF) as potential factors that could lead to both acute and chronic undernutrition.
ACF programme context
ACF has been present in Lebanon since 2006, working mainly in the southern region of the country, to provide humanitarian assistance to populations affected by the conflict between Lebanon and Israel. Until the latest crisis, the focus of assistance was mainly on food security and improvement of access to water, sanitation and hygiene (WASH). ACF scaled up activities in Lebanon in 2012 by developing programmes in the Bekaa Valley focusing on WASH in ITSs and collective shelters. ACF WASH interventions in this region aim at providing a comprehensive response to the refugee needs, including access to water and sanitation, waste management and hygiene promotion. In 2014, after assessments and resulting concerns about the nutrition situation of the refugee population, ACF began developing a nutrition programme in the Bekaa Valley. Raising awareness and providing appropriate support on IYCF was considered by ACF to be the most appropriate first response to prevent further deterioration of the nutritional situation. This programme was launched in March 2014 focusing on Aarsal, the area most impacted by refugee influx in the Bekaa Valley.
Project approach
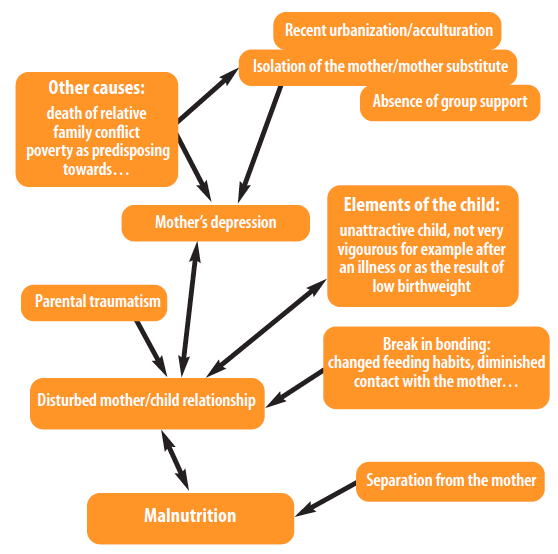
ACF’s approach to prevent undernutrition is to combine nutrition and psychosocial support5. Psychosocial support is promoted by ACF as an essential component of nutrition programmes, which focuses and emphasises the caregiver-child relationship. The psychosocial situation of caregivers and young children are identified as potential factors which can interfere with the capacity to recover from malnutrition, as well as influencing the causes of undernutrition (see Figure 1). The objective of ACF’s approach is to support caregivers to rediscover their self-confidence in order to increase their caring aptitudes and capacities. In the current context of Lebanon, this psychosocial component is essential given the stress and trauma experienced by the population targeted by the nutrition project as well as the duration of the crisis.
Figure 1: Psychological and sociological factors affecting nutritional status in chronic situations6
ACF’s nutrition project in Lebanon targets pregnant women and caregivers with children under 2 years of age. In this initial phase of the project, which started in March 2014 and ends in August 2014, ACF is providing the caregivers with a set of learning sessions on IYCF practices including hygiene sensitisation and care practices, as well as distribution of hygiene and baby kits comprising essential articles for children (soap, blanket, baby spoon, cup, etc).These services are provided in ACF tents (“Safe Havens”) set up within the ITSs to ensure access and reduce barriers of distance and potential transport costs. Each child admitted to the programme has his/her nutritional situation monitored monthly through mid-upper arm circumference (MUAC) and oedema assessments. Children suffering from acute malnutrition are referred to a nutrition centre for supplementary or therapeutic treatment but also continue to attend ACF’s programme. For children identified as suffering from malnutrition (MUAC < 125 mm) or at risk of malnutrition (125 mm ≤MUAC< 135 mm), their nutritional situation is monitored weekly. By the end of June 2014, 174 pregnant women and caregiver-child couples had benefited from this project.
Results from the field experience
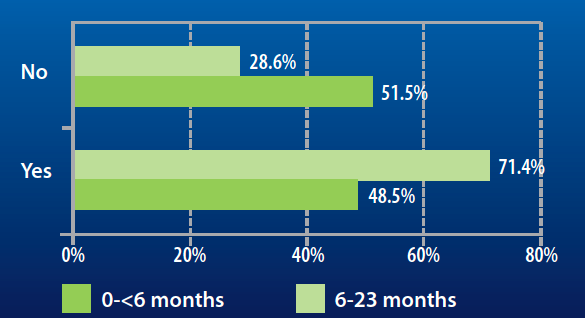
ACF has identified different practices hampering appropriate feeding and care for young children. Breastfeeding practices specifically as observed and assessed by the ACF field team are not optimal. Data collected from caregivers’ declaration at admission to the programme show that almost half of the children under 2 years old are not optimally breastfed according to WHO global recommendations (see Figure 2). According to field observations and discussion with caregivers, it also appears that caregivers spend little time breastfeeding and routinely supplement their breastmilk with water, sugar, tea and infant formula. Almost half of the infants aged 0-< 6 months admitted to the programme have received infant formula. This figure was more than 70% for children aged between 6-23 months (see Figure 3).
Figure 2: Percentage of exclusively breastfed and not exclusively breastfed children at programme admission according to caregiver declarations
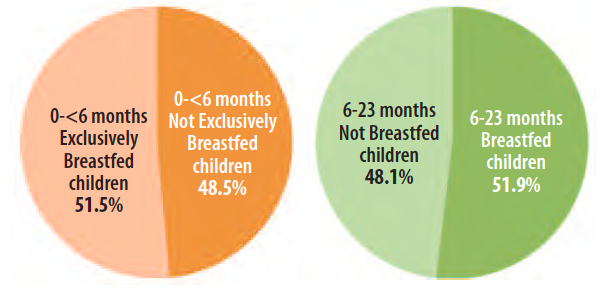
Figure 3: Percentage of children receiving or not infant formula at programme admission according to caregiver declarations
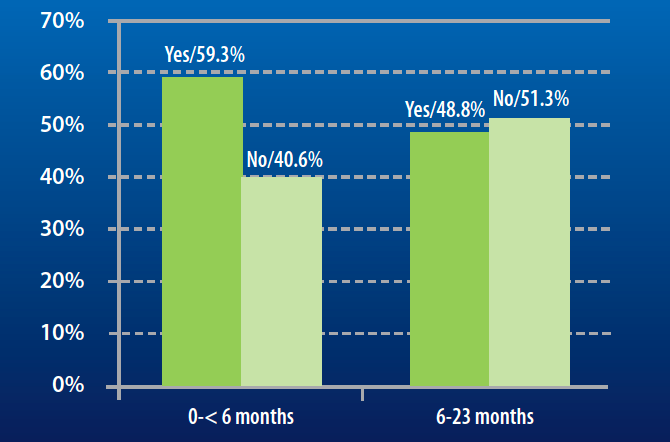
Early introduction of complementary food (at 4 months) is common and infants can be introduced to food tastes at an even earlier age (from 1 to 3 months of age). This partly relates to the widespread belief that breastmilk is not nutritious enough to meet infant needs. Caregivers also report breastfeeding difficulties, especially for infants under 6 months (see Figure 4). These difficulties are linked to a perceived lack of breastmilk by the caregiver and a child “refusing” the breast, or breast pain. The lack of perceived breastmilk could be linked to the established practice of using infant formula as an early food introduction. The common practice of mixed feeding through supplementation of breastmilk can then have a physiological impact on breastmilk production (i.e. less suckling leading to less milk production).
Figure 4: Breastfeeding difficulties reported by caregivers according to the age of their children at programme admission
Some women are also facing difficulties providing complementary food. It is, for instance, quite common that children above 6 months of age are fed mainly with breastmilk and infant formula. Child refusal of food is also a recurrent complaint received by ACF staff working within the programme. By looking in more depth at this complaint, it seems that women might not have the appropriate knowledge about complementary feeding practices and the quantity of solid food that a young child should receive per day. They complain about children “not eating” but in actuality they do, just not in sufficient quantity according to their mother’s expectation. These findings should be further explored and analysed to determine the extent of problems around complementary feeding.
 In a more general way and despite the efforts of the Ministry of Public Health to build dedicated programmes and provision of guidelines on IYCF in emergencies, the lack of information for health staff on IYCF can lead to the promotion of artificial feeding and limited support for breastfeeding at health facilities for the affected population. ACF considers also that these difficulties might be, for some cases, more psychosocial than physiological, especially perceptions of lack of breastmilk and child refusal of the breast. These difficulties could be linked to mother-child relationship difficulties, as well as less caring attitudes due to their current situation. Some women attribute their difficulties and incapacity to provide appropriate care for their children to their psychological status, i.e. they are depressed and/or anxious. It is also a common belief amongst Syrian refugee caregivers that stress and trauma affect their breastmilk quality, thus preventing them from breastfeeding.
In a more general way and despite the efforts of the Ministry of Public Health to build dedicated programmes and provision of guidelines on IYCF in emergencies, the lack of information for health staff on IYCF can lead to the promotion of artificial feeding and limited support for breastfeeding at health facilities for the affected population. ACF considers also that these difficulties might be, for some cases, more psychosocial than physiological, especially perceptions of lack of breastmilk and child refusal of the breast. These difficulties could be linked to mother-child relationship difficulties, as well as less caring attitudes due to their current situation. Some women attribute their difficulties and incapacity to provide appropriate care for their children to their psychological status, i.e. they are depressed and/or anxious. It is also a common belief amongst Syrian refugee caregivers that stress and trauma affect their breastmilk quality, thus preventing them from breastfeeding.
Discussion
Reflecting on our field experiences, we propose a number of recommendations to strengthen ACF’s IYCF programming in Lebanon.
Reflection 1: Influence of family members and impact on project quality
Grandmothers and mothers-in-law exert a powerful influence on household decision-making and may promote inappropriate feeding, such as early introduction of complementary food before 6 months of age. The ACF team has also observed some very young caregivers (under 18 years old) who are unable to act effectively on advice provided by ACF, due to conflicting advice and guidance from grandmothers and mothers-in-law. The perceptions of male members of the community also have an impact. Some men express concerns that this type of project, by gathering women together, is empowering them, hence they might not allow their wives to attend the sessions. This poses a challenge for ACF as the space provided is meant to be exclusively for women to receive support and express their concerns.
In order to make this type of project more accepted by the community, these spaces may need to be more open to men for specific sessions, as well to grandmothers and mothers-in-law. Without commitment and participation of the whole community, the impact of the programme may be reduced. ACF will address this by developing a strategy that will target these influential groups as part of the programme.
Reflection 2: Promotion of breastfeeding in a mixed feeding practices context
In efforts to promote breastfeeding, ACF is facing three main difficulties:
- Promotion of artificial feeding at health facilities, against MoPH guidance.
- Untargeted distribution of Breastmilk Substitutes (BMS) in ITSs.
- Established practices of artificial feeding of infants and young children in the population.
ACF adheres strictly to a policy of not promoting or supporting inappropriate use of BMS. However, there are practical considerations that must be taken into account, as well as the need for some form of pragmatic response, to meet the humanitarian needs of non-breastfed infants. ACF’s role, in addition to protection and support of breastfeeding, is also to ensure safe and appropriate artificial feeding. Even though there have been no studies or evidence available in this context, it is highly probable that artificial feeding is not safe in many of the poorly served ITSs. A few organisations are supporting non-breastfed children at health centres by providing kits to prepare infant formula safely. This is a start but a greater emphasis is needed to scale up and provide this type of service for non-breastfed infants, in conjunction with the development and dissemination of context-specific guidelines.
While ACF has no plans to develop a project on artificial feeding, this type of programming needs careful consideration from the wider humanitarian community as a practical response to this specific context.
Reflection 3: Psychosocial considerations
At this stage of the project, ACF has two main concerns. The first relates to caregiver capacity to care for their children appropriately due to their own or their children’s psychosocial status. Further assessments are needed in order to have a better understanding of the impact of psychosocial difficulties on child nutritional status. The second concern relates to the current living conditions of the refugees and their impact on children’s feeding ability. Even though there are no quantitative data currently available, the fact that some caregivers are complaining about their children’s refusal of solid food should be investigated7. Many caregivers also seem concerned about the impact of the living conditions on their children’s development as they see changes in their behaviours, e.g. children playing more violently and a regression to bedwetting.
Ways forward
ACF will, by August 2014, scale up its project by opening more Baby Tents in Aarsal and in other places in Bekaa Valley. While group counselling will remain a strong component of the project, ACF will also dedicate more time to individual counselling in this new phase. New activities will be added and ACF will support the national on-going effort on screening and treatment of acute malnutrition.
ACF will continue to work closely with its WASH department in order to improve hygiene practices among the caregivers participating in the programme. ACF will also investigate how best to to deal with non-breastfed infants, while also ensuring that breastfeeding is protected and enabling caregivers to make informed decisions about feeding practices.
Psychosocial support will continue to be an important element of the programme for both IYCF and CMAM. This will be strengthened by the deployment of psychologists in the programme.
For more information, contact Juliette Seguin, email:jseguin@lb.acfspain.org
1 WHO Regional Strategy on Nutrition (2010–2019) and Plan of Action
2 Joint Nutrition Assessment Syrian Refugees in Lebanon, MoPH and UNICEF, Final Report, February 2014 (pending confirmation of results)
3 Nutrition Assessment Report for Syrian Refugees in Lebanon using SMART methodology. UNICEF and WFP. Final Report, January 2013
4 http://www.moph.gov.lb/Prevention/Surveillance/documents/N10_2014May26.pdf
5Conceptual models of Child Malnutrition. The ACF approach in Mental Health and Care Practices. ACF International. Written by Cécile Bizouerne, first version 2005, revised 2012
6 Conceptual models of child malnutrition. The ACF approach in Mental Health and Care Practices, Page 35, ACF International, written by Cécile Bizouerne, first version 2005, revised 2012
7 On this matter, ACF is not planning any official investigation but is expecting to collect more information through the implementation and scaling up of its activities.


