Experiences of emergency nutrition programming in Jordan
 By Ruba Ahmad Abu-Taleb
By Ruba Ahmad Abu-Taleb
Ruba Ahmad Abu-Taleb is Nutrition coordinator at Jordan Health Aid Society (JHAS). She liaises between national and international NGOs and JHAS relating to all nutrition activities and oversees the implementation of all nutrition and health education related activities within JHAS clinics and outreach structures.
The author gratefully acknowledges the work and support of Dr Ann Burton, Health Unit/UNHCR, and Gabriele Fänder, Regional Health and Nutrition Advisor for MEDAIR. The author would sincerely like to acknowledge continual technical support and advice offered by UNHCR and MEDAIR to integrate nutrition services into primary health services of JHAS clinics and for integrating nutrition professionals into JHAS clinic teams. The author would also like to express profound gratitude and deep regards to the continual guidance and support of JHAS founder (Dr. Yaroup Al-Ajlouni) and JHAS projects manager (Nicola Dababneh). Sincere thanks also go to the various departments of JHAS for their kind cooperation and valuable insights.
The founding team of the Jordan Health Aid Society (JHAS) in 2005 comprised Jordanians keen to enforce local leadership in order to respond effectively to humanitarian needs of vulnerable population groups (see a profile on JHAS in this edition of Field Exchange). One of the earliest humanitarian calls to which JHAS responded was the Iraqi crisis. Since then, JHAS has increased its experience, expertise and collaborative working relationships to respond to different humanitarian emergencies in the Middle East and North Africa (MENA) region. JHAS missions have included emergency response teams comprising experienced medical and non-medical supporting staff deployed to the Gaza strip, South Sudan, Yemen and Libya.
 Over the years, JHAS had established a solid network of primary static and mobile health care clinics in Jordan where different primary medical and health services have been incorporated. With the onset of the Syrian crisis in March 2011, humanitarian and health aid responses in Jordan began a new chapter. In the earliest stages of the Syrian crisis, humanitarian aid was provided to assemble refugee camps and to supportemergency/life-saving aid. However, access to quality nutrition among refugees with specific nutritional requirements, such as pregnant and lactating women (PLW) and infants and young children, was limited since only general food rations were provided. At the same time, food insecurity due to social, health and protection issues was an identified problem but remained unresolved. The situation became even more complicated with refugees’ urbanisation, as resources like food coupons had to be exchanged for shelter and other basic survival needs. According to UNHCR registration records, the total number of Syrian refugees in Jordan had reached 597, 328 by June 2014 of which only 16.26% are hosted in refugee camps. The remainder of Syrian refugees have settled within host communities1.
Over the years, JHAS had established a solid network of primary static and mobile health care clinics in Jordan where different primary medical and health services have been incorporated. With the onset of the Syrian crisis in March 2011, humanitarian and health aid responses in Jordan began a new chapter. In the earliest stages of the Syrian crisis, humanitarian aid was provided to assemble refugee camps and to supportemergency/life-saving aid. However, access to quality nutrition among refugees with specific nutritional requirements, such as pregnant and lactating women (PLW) and infants and young children, was limited since only general food rations were provided. At the same time, food insecurity due to social, health and protection issues was an identified problem but remained unresolved. The situation became even more complicated with refugees’ urbanisation, as resources like food coupons had to be exchanged for shelter and other basic survival needs. According to UNHCR registration records, the total number of Syrian refugees in Jordan had reached 597, 328 by June 2014 of which only 16.26% are hosted in refugee camps. The remainder of Syrian refugees have settled within host communities1.
With the escalation of the Syrian crisis, agencies with experience of humanitarian nutrition programme implementation, such as MEDAIR and Médecins Sans Frontières (MSF), pointed out critical issues that could aggravate the already complex and challenging nutritional situation of the refugee population, such as poor shelter conditions, limited general food rations, cold winters and very poor hygiene conditions, which commonly predispose to impaired health status. Appropriate nutrition programming during the early stages of the Syrian crisis was constrained by a lack of updated data on malnutrition prevalence amongst the Syrian refugees. National pre-crisis data from Syria (2009) recorded a prevalence of 12% wasting, 10% underweight and 28% stunting, which while not ideal, were not at emergency levels. However, given the unfolding situation, it was clear that there was a need for an up-to-date nutrition survey for this refugee population.
In November 2012, a nutrition survey of Syrian refugees in Jordan found a 5.1% prevalence of wasting2 among children under five years in host communities and 5.8% in Za’atari camp (the main camp for Syrian refugees in Jordan), 8.2% stunting in host communities and 15.9% in Za’atari camp3, and 2% underweight in host communities and 6.3% in Za’atari camp. Although these results were not a trigger for ‘emergency’ nutrition interventions, they did raise concerns amongst the nutrition group of humanitarian agencies working in Jordan, about the need to maintain systematic screening and surveillance, especially for vulnerable population groups such as children and PLW. This was especially a concern as refugees continued to arrive in Jordan in ever increasing numbers. In line with this thinking, integration of medical nutrition services into primary health care seemed a sound approach to facilitate early diagnosis of malnutrition, thereby helping prevent an increased prevalence of acute malnutrition.
Programming through partnership
JHAS and MEDAIR partnered in 2013 to implement a comprehensive programme on Community-based Management of Acute Malnutrition (CMAM) and Infant and Young Child Feeding (IYCF) practices. Initially, the JHAS-MEDAIR partnership introduced screening for acute malnutrition indicators to the primary medical practice within JHAS clinics in January 2013. This was preceded by a comprehensive IYCF/CMAM training in December 2012 of selected staff (medical doctors, nurses, midwives, health educators and community outreach workers). From January to October 2013, MUAC only was used in screening. Weight for height (WFH) was added to screening in October 2013 in preparation for implementing the outpatient therapeutic programme (OTP) and the supplementary feeding programme (SFP), since both use WFH as an admission criterion and for follow-up. JHAS, with technical support from MEDAIR , has become a lead agency in Jordan with capacity to implement this type of programme.
A number of agencies, including UNHCR, UNICEF, WFP and Centres for Disease Control and Prevention (CDC), collaborated to plan and implement another nutrition survey in April 2014. JHAS, in partnership with MEDAIR, participated in supervising survey teams and in the data collection component. The survey targeted Syrian refugee children (0-5 years old) and women of child bearing age ((CBA); 15-49 years old). The survey measured MUAC, WFH and blood haemoglobin (Hb) status. In addition, respondents were asked questions about food security status, water, sanitation and hygiene (WASH) conditions of refugee families, as well as polio and measles vaccination coverage. Preliminary results4 indicate alarming levels of iron deficiency anaemia among women and children within both camps and urban settings (see Table 1). Global acute malnutrition (GAM) rates were relatively low: GAM (MUAC based) prevalence was 1.5% inside Za’atari camp and 0.4% outside the camp (urban setting). However, findings for many other indicators that directly or indirectly impact on nutrition - anaemia prevalence, compromised food security, IYCF practices, shelter and WASH conditions - all confirmed concerns of a risk of a worsening nutritional status of the Syrian refugee population. Thus, the nutrition sub-working group is currently looking for opportunities to scale up nutrition programmes and introduce other potentially needed interventions.
| Table 1: Preliminary results* of blood Hb status survey in targeted groups within camp and urban settings | ||
|
|
Za’atari Camp |
Non-camp (urban) settings |
Women 15-49 years |
45.0 % |
31.0 % |
Children under 5 years |
49.0 % |
25.9% |
*Reported figures in the table are preliminary and final results are yet to be officially reported.
After almost 18 months since JHAS started applying malnutrition screening in clinics, JHAS has become the sole agency in Jordan to implement SFPs within urban settings and a comprehensive OTP within camps and urban settings, with ongoing technical support from UNHCR and MEDAIR. The SFP began as a targeted programme (malnourished children under 5 years and PLW) and in June 2014, was expanded to both blanket and targeted programming (through the addition of all children less than 5 years in JHAS clinic and outreach settings).
Capacity development
Over 100 national and international non-governmental organisations (NGO) and partners of UN agencies have been working in Jordan in response to the Syria crisis. The partnership between UNHCR and JHAS has further strengthened the capacity of JHAS to become the first line healthcare provider for the Syrian refugees in Jordan. JHAS staff have regularly attended national health sector meetings and sub-working groups, which has allowed JHAS to participate in identifying key strategic areas for humanitarian interventions in health and nutrition.
The credibility of JHAS has been enhanced by participation in a number of trainings. MEDAIR has conducted trainings on CMAM and IYCF for health workers in JHAS on a regular basis. At Nutrition Working Group level, JHAS attended training on SFP implementation organised by WFP for partner agencies. At the regional level, selected JHAS staff attended a Middle East and North Africa (MENA) Region Nutrition in Emergencies training. While these trainings have been technical in nature, they have also equipped trainees with an understanding of the protection rights of refugees, as well as the need to be considerate of specific social, cultural and psychological characteristics of those accessing services.
Implementation of the nutrition programmes
Guidance development
Although prevalence of acute malnutrition has been low, the Nutrition Working Group5 advocated for preparedness measures, such as drafting context-specific guidelines and standard operating protocols for the treatment of acute malnutrition and anaemia. The Nutrition Working Group assembled a task force consisting of JHAS, MEDAIR and Save the Children Jordan (SCJ) to draft operational guidelines for the integrated management of acute malnutrition and management of iron deficiency anaemia in pregnancy.
The CMAM programme
Syrian refugee children and PLW have been regarded as the most vulnerable population group and therefore, are the primary target group in the CMAM programme. The programme has focused on community mobilisation to maximise coverage, access and compliance. JHAS clinics and outreach settings have been able to integrate management of acute malnutrition into their daily working schemes.
The four main elements of the CMAM programme are management of moderate acute malnutrition (MAM/SFP), management of severe acute malnutrition (SAM/OTP), inpatient management for severe acute malnutrition with medical complications (SAM/SC) and community outreach. Admission and discharge criteria are reported in Tables 2, 3 and 4.
| Table 2: Admission and discharge criteria to inpatient care (SAM with medical complications) | ||
|
|
Admission criteria |
Transfer to OTP/SFP |
Children 6-59 months |
WFH < -3 z score or MUAC< 11.5 cm PLUS any of the following medical complications: + Anorexia + Intractable vomiting + Convulsions + Lethargy, not alert + Unconscious + Lower respiratory tract infection + High fever + Severe dehydration + Severe anaemia + Hypoglycaemia + Hypothermia |
Medical complications stabilised
Successful appetite test
Children transfer to either OTP or SFP depending on their anthropometric status
|
|
Bilateral pitting oedema ++ or any grade of bilateral pitting oedema with severe wasting. |
||
| Table 3: Admission and discharge criteria for OTP (SAM without medical complications) | ||
|
|
Admission criteria |
Discharge criteria |
Children 6-59 months |
WFH less than -3 z scores and/or MUAC of less than 11.5cms |
Children are discharged according to their admission criteria: + WFH greater than -3 z scores at two consecutive visits and/or + MUAC greater than or equal to 11.5 cm at two consecutive visits |
|
Bilateral pitting oedema + and ++ |
+ 15% weight gain (from admission weight when free of oedema) + No oedema for two consecutive weeks + Clinically well and alert |
|
|
Discharged from inpatient care |
Anthropometric discharge criteria as above. |
|
| Table 4: Admission and discharge criteria for SFP (MAM cases) | ||
|
|
Admission criteria |
Discharge criteria |
Children 6-59 months |
WFH less than -2 z scores and greater than -3 z scores |
WFH greater than -2 z scores at two consecutive visits |
|
MUAC less than 12.5cm and greater than or equal to 11.5cm |
MUAC greater than or equal to 12.5 cm at two consecutive visits |
|
|
Discharged from OTP |
Children discharged from OTP should stay in the SFP for a minimum of 2 months |
|
|
Discharged from inpatient care |
Children discharged from inpatient care* should stay in the SFP for a minimum of 2 months |
|
PLWs |
MUAC less than 23cm for pregnant woman in second or third trimester |
MUAC greater than or equal to 23 cm at two consecutive visits or when the infant becomes 6 months** Infants aged 6 months and older should be assessed by MUAC and referred appropriately |
|
MUAC less than 23cm for lactating women with infants younger than 6 months |
||
* Children stay in inpatient care until their medical condition has stabilised. Afterwards are discharged into OTP or SFP according to their anthropometric (MUAC/WFH) indicators.
**If a mother is compliant with the programme but has remained malnourished for more than 4 months, complicating medical conditions or social aspects are investigated and necessary support provided.
SFPs and OTPs operate in both Za’atari camp and urban settings. In Za’atari camp, JHAS/UNHCR supports the OTP while SCJ/WFP supports the SFP. Outside the camp setting, mobile JHAS clinics are employed for remote areas or where transport for patients is unavailable, through which CMAM services are made available or accessed (see Box 1). Within urban settings, JHAS in collaboration with UNHCR and MEDAIR, support nine OTP/SFP sites. This comprises six JHAS static clinics, one MMU, and two OTP/SFP sites in Jerash and Ajloun implemented by local community based organisations (CBOs) (therapeutic and supplementary food provision happens once weekly at each CBO site). Other mobile services screen for malnutrition using MUAC tapes and refer to the nearest JHAS clinics.
Box 1: Mobile JHAS clinic services
- One fixed mobile medical unit (MMU) with scheduled trips within southern governorates of Jordan (Tafilah, Kerak, Ma’an, Aqaba, Qatranah and Madaba). This unit provides primary medical care and facilitates secondary referrals through defined local stations in southern governorates. CMAM services are completely supported through the MMU.
- One community outreach team consisting of 10 community health workers, responsible for liaising between refugee population and JHAS in terms of health care services’ provision and UNHCR registration issues.
- One medical team deployed once weekly to remote areas of Jordan (those not covered by the MMU schedule). This team responds to requests from local communities to implement a ‘Free Medical Day’6.
Both WFH and MUAC criteria are used to assess children and a thorough medical evaluation is conducted on admission. Medication and OTP/SFP foods (Ready to Use Therapeutic Food (RUTF) for SAM children and Super Cereal Plus for MAM children and PLW’s) are prescribed according to standard protocols. Therapeutic and supplementary food commodities have been approved for use in both camp and non-camp settings, which has made it possible to facilitate integrated CMAM programmes in both contexts.
For SAM children in particular, physical examination also aims to identify acute medical conditions requiring hospitalisation. Where such cases are identified, JHAS facilitates the referral process through an established network with affiliated MoH hospitals. JHAS focal points in each hospital follow up with admitted cases and provide timely feedback. Malnourished SAM or MAM children with chronic illnesses are treated as outpatients, in close cooperation with JHAS nutritionists for potential nutritional support needed. Anthropometric evaluation and monitoring of PLWs is conducted solely through MUAC measurements.
In all urban JHAS clinics and in Za’atari camp, a specific day of the week has been assigned for OTP/SFP RUTF prescription/RUSF provision. However if a SAM child is identified within the week, s/he receives medical and nutritional assessment and a RUTF ration until the nominated attendance day. On attendance, patients are followed up and monitored and there are Super Cereal cooking demonstration sessions. It appears that the exchange of experiences between SFP and OTP clients has improved SFP compliance, i.e. reduced defaulting.
 Management of iron deficiency anaemia in pregnancy
Management of iron deficiency anaemia in pregnancy
As part of standard antenatal care visits, pregnant women in JHAS clinics are screened for their blood Hb status. A blood Hb level less than 11 g/dl is classified as moderate anaemia, whereas, a blood Hb status less than 7.9 g/dl is classified as severe anaemia. In the latter case, a pregnant woman will be directly referred for urgent medical care through JHAS affiliated hospitals. According to operational guidelines developed by the Nutrition Working Group, pregnant women receiving antenatal care within JHAS clinics receive supplementary doses of iron and folic acid starting from the second trimester of pregnancy until 6 months postpartum (see Table 5). Pregnant women remain under close medical supervision, in case dosage alterations are needed. To date, there has been no specific programme regarding anaemia in children less than 5 years, however this has been integrated into the Nutrition Working Group strategy for 2014.
| Table 5: Guidelines for iron supplementation to pregnant women | ||||
Age Groups |
Indications for supplementation |
Dosage schedule |
Duration |
|
Pregnant women |
Universal supplementation |
Iron: 60 mg/day Folic acid: 400 μg/day |
6 months in pregnancy |
|
Lactating women |
Where anaemia prevalence is above 40% |
Iron: 60 mg/day Folic acid: 400 g/day |
6 months in pregnancy, and continuing to 3 months postpartum |
|
Programme figures
A relatively low number of children have been diagnosed with SAM or MAM in 2014 in both urban JHAS clinics and Za’atari camp (see Tables 6 and 7). This accords with the 2014 nutrition survey data. Given the relatively low caseload in Za’atari camp, JHAS in coordination with SCJ have had capacity to conduct regular counselling visits for SAM patients, especially those missing their distributions. This has allowed caregivers to discuss any constraints they have in programme participation with JHAS staff.
Interestingly, PLWs have so far represented the majority of SFP beneficiaries. This has raised several questions around food security and protection issues. This relatively high caseload of malnutrition amongst PLW is mirrored in their blood Hb status. The prevalence of iron deficiency anaemia (IDA) among pregnant women screened for their blood Hb status within JHAS clinics in 2014 is reported to be 43.16%. The cultural propensity to early marriage may be partially contributing to compromised maternal health, as a pregnant teenager faces increased demand for nutrients to support both foetal growth and adult maturation.
| Table 6: Malnourished children and PLWs enrolled in urban programmes | ||
|
|
Indications for supplementationAccumulative 2014 (week 25, June 2014) |
|
Children with MAM |
56 children still in SFP |
|
Children with SAM |
6 boys in OTP |
|
|
2 girls in OTP |
||
Malnourished PLW |
88 pregnant women and 78 lactating women in SFPTP6 boys in OTP |
|
| Table 7: SAM children enrolled in OTP* within Za’atari camp | ||
|
|
Accumulative 2014 (week 25, June 2014) |
|
Number of SAM children in Za’atari camp |
23 boys in OTP |
|
|
23 girls in OTP |
||
*JHAS only implements OTP in Za’atari camp. The SFP is implemented by SCJ, hence figures are not presented here.
 Challenges and observations
Challenges and observations
A number of challenges were encountered as MUAC screening was rolled out amongst JHAS health workers in JHAS clinics and outreach settings. Both health practitioners and beneficiaries were unfamiliar with MUAC measurement, resulting in poor MUAC measuring accuracy. This was often compounded by caretakers having difficulty in calming the child or getting the child to expose the whole of their arm, especially in cold weather conditions. In addition, given the very low initial caseload, some practitioners questioned the value of MUAC as an accurate indicator of malnutrition, especially when some children who looked pale, weak or detached were found to have a normal MUAC measurement.
Another challenge faced by JHAS teams was fostering sufficient understanding of CMAM/IYCF concepts, especially when there was a significant delay in getting the therapeutic and supplementary foods approved and released in Jordan. The first step in procuring the therapeutic and supplemental food commodities was to decide, at Nutrition Working Group level, which products were needed. Procurement of Super Cereal Plus (for SFP) and Ready to Use Therapeutic Food7 (RUTF) (for OTP) was agreed. WFP was responsible for securing MoH approval to procure Super Cereal Plus. Although MoH approvals were granted later than expected, the considerable delay in launching the SFP was largely due to delayed custom’s release of Super Cereal Plus and time taken to secure the necessary Jordan Food and Drug Administration (JFDA) approvals. As a learned lesson, the Nutrition Working Group contacted all authorities prior to international procurement of RUTF in order to avoid any further delay in implementing the OTP. As a result, RUTF procurement and JFDA’s approvals all went smoothly without significant delays.
The delays in SFP and OTP programming due to supply issues required stop-gapping at an operational level. The majority of children and PLWs identified as malnourished were regular patients at JHAS clinics so that retrieving their records and getting in contact with them was possible once therapeutic and supplementary foods had become available. Although JHAS teams were able to overcome the problem of refugees changing residence by referring to the nearest JHAS clinic and exchanging patient data, a few patients were untraceable and therefore dropped out because of disconnected phone numbers.
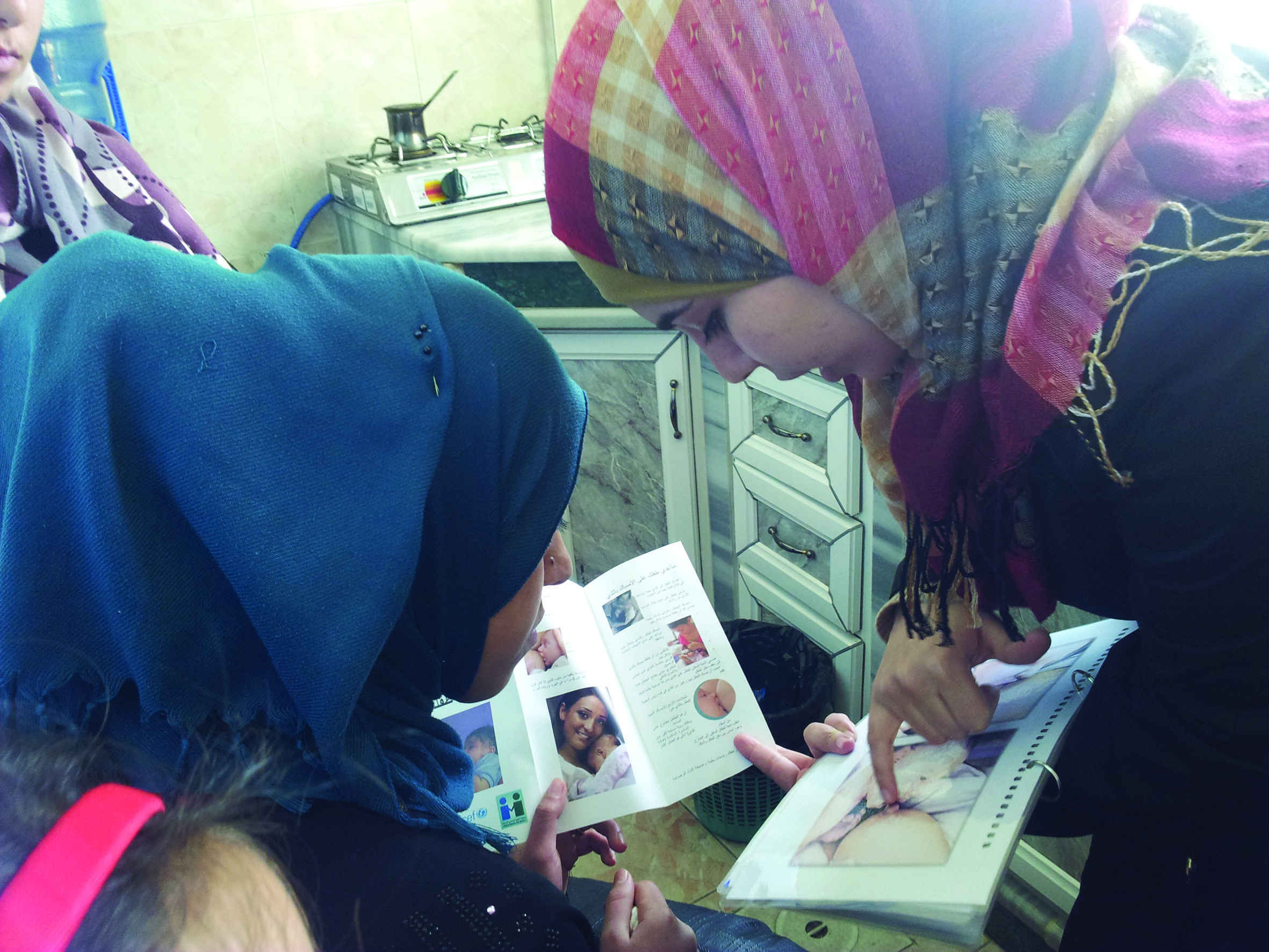
A challenging part of outreach work has been trying to support young mothers around breastfeeding. Given the cultural norms in Syria, girls become mothers at a very young age and are usually put under pressure to wean female infants to increase the chance of becoming pregnant, hoping that the next child will be a boy. Community outreach workers also report that refugees’ interest in, and acceptance of, nutrition education is compromised. This is particularly the case in refugee extended family contexts, where cash and shelter needs are prioritised over other needs including health and nutrition.
 Lessons learned
Lessons learned
The partnerships with UNHCR and MEDAIR have given JHAS a wealth of expertise to invest in future sustainable national action plans for the management of acute malnutrition. However, the skills of health and nutrition professionals at JHAS still need to be strengthened to meet the needs of different targeted populations.
As JHAS had taken the lead role in screening for malnutrition within urban settings, refresher trainings and frequent supervision visits to health workers has provided strong motivation for JHAS staff.
Although screening and health education has gradually been improving, patient compliance with the SFP/OTP programmes has been difficult to achieve. JHAS nutritionists working in clinics have therefore linked each patient with MEDAIR community outreach volunteers. This has allowed for follow up and communication beyond the clinic setting and contributed to better understanding amongst mothers and caretakers of the underlying causes of malnutrition and how to address them.
Other efforts to improve SFP and OTP performance have included caretakers’ focus group discussions and cooking sessions in JHAS clinics to demonstrate optimal Super Cereal cooking methods and recommended consistency. Mothers used to undercook the Super Cereal Plus which negatively affected its taste; satisfaction of mothers and children with Super Cereal Plus has now improved. In Za’atari camp, focus group discussions and linkages with outreach workers have hugely improved caretakers’ compliance with SAM treatment programmes. Caretakers are asked to return empty RUTF/Super Cereal Plus packets as one marker of compliance. This has, in turn, been reflected in improvement in the health status of SAM children and an increased numbers of caretakers presenting to JHAS clinics asking to have their children screened for malnutrition.
The low caseload of acute malnutrition in Jordan in camps and urban settings has provided room for gradual capacity building of JHAS health and nutrition professionals. The experience from this relatively small scale CMAM will be a solid base for JHAS to scale up programming for any nutrition emergency.
For more information, contact: Ruba Ahmad Abu-Taleb, email: r.abutaleb@jhas-international.org
Mobile: +962 77 7466 610 Web: www.jordanhealthaid.org
1 Source: data.unhcr.org, 2014
2 Based on weight-for height (WFH)
3 Inter-agency nutrition assessment Syrian refugees in Jordan host communities and Za’atari camp. Final report. January 2013. Available from UNHCR Syria response online portal at http://data.unhcr.org/syrianrefugees/country.php?id=107
4 Results pending (June 2014). Check for updated availability at http://data.unhcr.org/syrianrefugees/regional.php?
5 Nutrition is covered in a sub-working group of the Health Working Group. It is co-chaired by UNHCR and Save the Children Jordan.
6 A free medical day is a term used to describe the activity of providing primary medical care free of charge. This term is used by different community based organisations in Jordan.
7 Plumpy’nut


