Malnutrition peaks during malaria epidemic in Northwest Nigeria
 By Chloë Wurr, Joke Zeydner and Saskia van der Kam
By Chloë Wurr, Joke Zeydner and Saskia van der Kam
 Chloë Wurr is a medical doctor in Alaska and worked as medical coordinator with MSF-OCA Nigeria
Chloë Wurr is a medical doctor in Alaska and worked as medical coordinator with MSF-OCA Nigeria
 Joke Zeydner is a medical doctor in The Netherlands and worked as medical coordinator with MSF-OCA Nigeria
Joke Zeydner is a medical doctor in The Netherlands and worked as medical coordinator with MSF-OCA Nigeria
 Saskia van der Kam is a nutrition specialist with MSF-OCA based in Amsterdam
Saskia van der Kam is a nutrition specialist with MSF-OCA based in Amsterdam
Location: Nigeria
What we know: GAM is prevalent in Northern Nigeria. Seasonal peaks in acute malnutrition are often assumed to be linked to food insecurity.
What this article adds: MSF supported SAM treatment services in Goronyo LGA experienced alarming peaks in admissions in August 2012 which was not expected (no food security/nutrition issues in surveillance). A rapid increase in malaria admissions to the Goronyo health centre in August corresponded with this unusual SAM peak; 70% of SAM admissions were confirmed malaria cases. Support to CMAM scale up tends to focus on RUTF delivery and associated training; medical aspects of protocols are often under-resourced and managed by different ministries/agencies. Integration of funding and services to treat both childhood diseases and malnutrition is needed.
Médecins Sans Frontières-Operational Centre Amsterdam (MSF-OCA) has provided humanitarian assistance in Northwest Nigeria since 2008, delivering medical support to Sokoto State Hospital Goronyo. Activities include outpatient (OPD) and hospital based medical care for children less than five years of age, including a Therapeutic Feeding Programme (TFP) with both intensive inpatient services (ITFC) and outpatient ambulatory phases (ATFP). Goronyo Local Government Authority (LGA, administrative level comparable with a district) is located in Sokoto State and had a population in 2011 of 205,247 with an estimated population of 34,892 children aged less than 5 years. In the absence of other functioning medical services, MSF-OCA’s catchment area is much wider, including many families from surrounding LGAs.
This region of Nigeria is rural and primarily dependent on agriculture and animal husbandry for its livelihood, with some income derived from trade and small-scale manufacturing. The Goronyo LGA livelihood zone is characterised by a decades-old irrigation scheme. A variety of crops are grown in dry lands, as well as the irrigated areas, such as millet, sorghum, rice, groundnuts and cowpeas, while vegetables such as okra, onions, spinach and tomatoes are important products of the irrigated soils. The irrigated areas also favour substantial secondary cropping of maize, sweet potatoes, and cassava.
Despite the strength of its agricultural sector, northern regions of Nigeria experience higher rates of malnutrition than expected. Nutrition surveys in Goronyo LGA in March 2009 and March 2010 showed a global acute malnutrition rate (GAM) of 14.8% and 11.5% respectively and a severe acute malnutrition rate (SAM) of 4.9% and 2.6% respectively. UNICEF’s SMART nutrition cluster studies carried out in Sokoto and other northern states since 2010 have found GAM rates between 11.3-12.6% and SAM prevalence of 1.3-2.9% during the last three years. MSF-OCA’s experience in Goronyo concurs with these findings, with high participation in the TFPs among the population of children who use our health services.
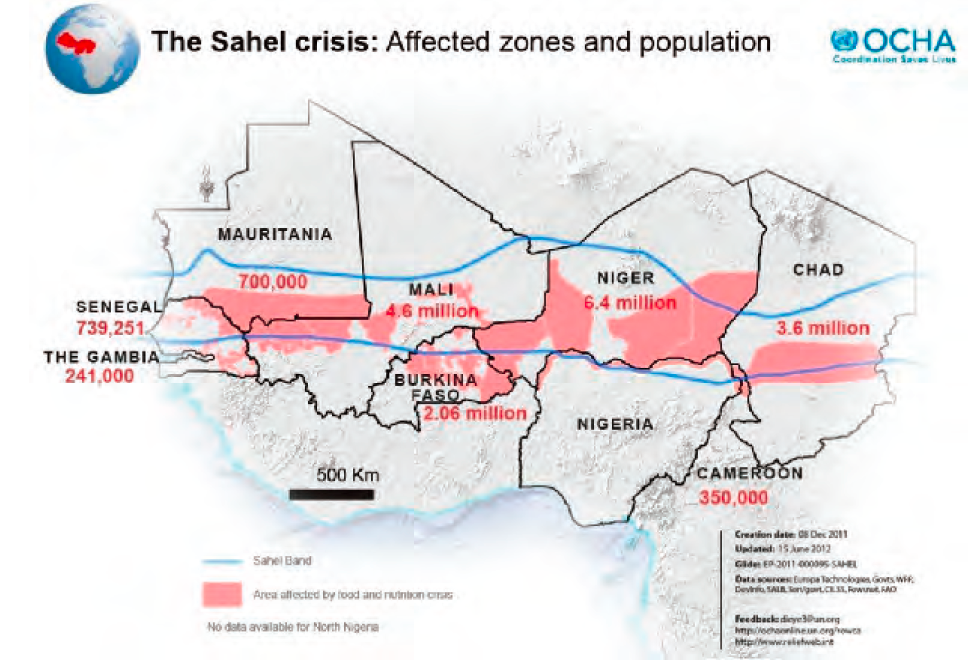
This region of Nigeria borders the Niger Republic, along the southern reaches of the Sahel belt, which is prone to food crises and epidemics. During 2012, in response to international concerns of an impending food crisis in the Sahel region, the MSF-OCA Nigeria Mission undertook nutrition and food security surveillance along the borders with the Niger Republic, to provide early warning of regional population movements and increasing malnutrition rates. Ultimately, our monitoring did not identify any particular food security concerns or population movements from the north in search of food. The TFP experienced its usual rates of participation until August 2012 when TFP admissions suddenly increased to more than double the average for the same month in the two previous years (see Figure 1). The increase in children with SAM was seen in both the ITFC and ATFP. The rapid increase in numbers overwhelmed the programme so that in September, MSF was forced to refer patients from other LGAs, who needed admission to the ATFP, to services near their home. This reduced overall activity in Goronyo and resulted in a sharp decrease in admissions (see Figure 1).
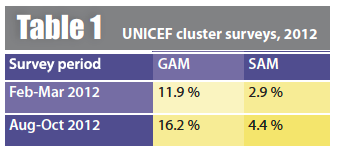
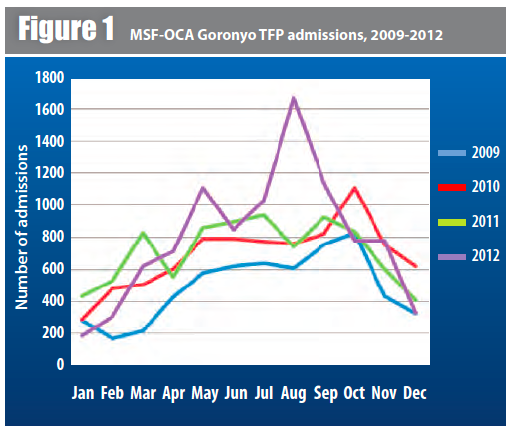 These high rates of TFP admissions in 2012 are particularly notable because MSF-OCA operated fewer ambulatory feeding programme sites in 2012 (4 sites) than in 2011 (7 sites), having closed three of seven sites at the end of 2011. A UNICEF SMART cluster survey carried out in August-October 2012 in Sokoto State also detected alarming increases in rates of GAM and SAM when compared to rates found in the same state earlier in the year (see Table 1).
These high rates of TFP admissions in 2012 are particularly notable because MSF-OCA operated fewer ambulatory feeding programme sites in 2012 (4 sites) than in 2011 (7 sites), having closed three of seven sites at the end of 2011. A UNICEF SMART cluster survey carried out in August-October 2012 in Sokoto State also detected alarming increases in rates of GAM and SAM when compared to rates found in the same state earlier in the year (see Table 1).
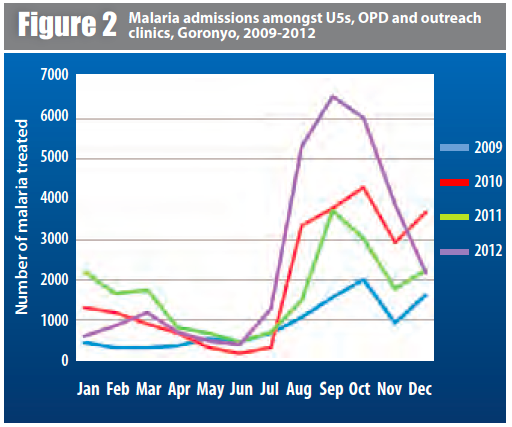
In August 2012, while our TFP was admitting record numbers of patients with SAM, the Goronyo Outpatient Clinics (OPD) experienced a huge influx of children less than five years with confirmed malaria, surging from under 100 cases in the second week of July to 833 cases in the fourth week of July. The number of cases of malaria, all confirmed by rapid diagnostic test (RDT), remained high through the end of October, with almost 18,000 children less than five years of age treated from August to October. This seasonal peak is seen in our malaria rates for 2012 as a whole, during which time MSF treated 29,183 children for malaria in four outpatient clinics. During the same year, 1,874 children under five years were admitted to the hospital for severe malaria. From September, over 70% of children with SAM admitted to the ITFC and over 50% of those admitted to the ATFC had malaria as shown by systematic screening upon admission with a rapid malaria test. This compares to rates of less than 10% during the low season.
Discussion
The rapid increase in rates of malaria in August corresponded to the unusual peak in admissions to the TFP during the same period, underscoring the relationship between disease and malnutrition. While presentation to the OPD for treatment of malaria may have increased our detection of SAM in the population, it is likely that bouts of malaria contributed to malnutrition in vulnerable children. Conversely, children with malnutrition are at greater risk of complications from malaria and other childhood diseases, requiring hospitalisation and increasing mortality.
 This vivid connection between malaria and malnutrition informs our understanding of malnutrition in a region not suffering from food insecurity and explains why delivery of food aid alone is not sufficient to reduce rates of malnutrition in such areas. In the catchment area of the Goronyo TFP, primary health care clinics are scarce and those that do operate lack consistent access to drugs and vaccines. As a result, children in this region go untreated for common childhood illnesses contributing to the unexpectedly high rates of malnutrition we see.
This vivid connection between malaria and malnutrition informs our understanding of malnutrition in a region not suffering from food insecurity and explains why delivery of food aid alone is not sufficient to reduce rates of malnutrition in such areas. In the catchment area of the Goronyo TFP, primary health care clinics are scarce and those that do operate lack consistent access to drugs and vaccines. As a result, children in this region go untreated for common childhood illnesses contributing to the unexpectedly high rates of malnutrition we see.
Similarly malnutrition can only be cured if underlying disease is addressed.
The Community Management of Acute Malnutrition programme (CMAM) established by the Nigerian government with the support of UNICEF addresses primarily the malnutrition component by providing Ready To Use Therapeutic Food (RUTF) and training. While standard antibiotics and testing for malaria (and treatment when positive) are recommended in the CMAM protocol, they are not always provided as nutrition programmes frequently lack medical capacity, diagnostic tools and drugs to treat illness.
 A complicating factor is that in Nigeria, the CMAM programme is administered by the State Primary Health Care Development Agency (SPHCDA) while primary health care, including diagnosis and treatment of malaria and childhood illnesses, is the responsibility of the State Ministry of LGA Affairs with few resources to provide this essential medical care.
A complicating factor is that in Nigeria, the CMAM programme is administered by the State Primary Health Care Development Agency (SPHCDA) while primary health care, including diagnosis and treatment of malaria and childhood illnesses, is the responsibility of the State Ministry of LGA Affairs with few resources to provide this essential medical care.
The separation between nutrition and primary health care is not unique to Nigeria. Generally CMAM programmes are successful in supporting primary health structures with training and providing therapeutic foods, focusing on early case finding and decentralisation of nutrition care. But the medical component is under resourced, partly because medical care is under resourced in general, but also because medical care is the responsibility of another agent and not included in CMAM funding. As long as funding for treatment of malnutrition is separated from primary health care funding, comprehensive treatment of malnutrition and effective prevention of malnutrition are not possible. With this neglect of primary care services, children are more likely to become malnourished from disease, and yet, once malnourished, treatment will only be successful when the underlying diseases are addressed. Effective strategy for the prevention and treatment of malnutrition requires integration of services to treat both childhood diseases and malnutrition concurrently.
For more information, contact: Saskia van der Kam, email: Saskia.van.der.Kam@amsterdam.msf.org


