Simplifying the response to childhood malnutrition: MSF’s experience with MUAC-based (and oedema) programming
By Kevin P.Q. Phelan, Candelaria Lanusse, Saskia van der Kam, Pascale Delchevalerie, Nathalie Avril and Kerstin Hanson
 Kevin P.Q. Phelan was the Nutrition Working Group Leader for MSF International Office from October 2013-April 2015).
Kevin P.Q. Phelan was the Nutrition Working Group Leader for MSF International Office from October 2013-April 2015).

Candelaria Lanusse has been the Nutrition Referent for MSF Operational Centre Barcelona since January 2015.
 Pascale Delchevalerie is a paediatric nurse with a Master’s degree in epidemiology who has been working with MSF since 1991. She has been the Nutrition Referent for MSF Operational Centre Brussels since 2004.
Pascale Delchevalerie is a paediatric nurse with a Master’s degree in epidemiology who has been working with MSF since 1991. She has been the Nutrition Referent for MSF Operational Centre Brussels since 2004.
 Nathalie Avril is Nutrition Advisor for MSF Operational Centre Geneva.
Nathalie Avril is Nutrition Advisor for MSF Operational Centre Geneva.
 Kerstin Hanson, MD is a Paediatric/Nutrition Advisor for MSF Operational Centre Paris.
Kerstin Hanson, MD is a Paediatric/Nutrition Advisor for MSF Operational Centre Paris.
 Saskia van der Kam is a nutrition specialist at MSF Operational Centre Amsterdam.
Saskia van der Kam is a nutrition specialist at MSF Operational Centre Amsterdam.
Location: Global
What we know: MUAC and WHZ are commonly used anthropometric criteria for admission to CMAM programmes. WHO recommends that the specific anthropometric indicator used to confirm SAM should also be used to assess nutritional recovery. MUAC is a simpler, faster and more immediate measure that identifies malnourished children at higher risk of death. There is limited evidence on outcomes of untreated children with low WHZ (but acceptable MUAC).
What this article adds: From 2007 to the present, MSF has operated MUAC (and oedema) only based CMAM programming in a number of challenging emergency contexts. MUAC thresholds for admission varied from <115 mm to <125mm with differing prescribed lengths of stay according to contextual factors, e.g. prevailing mortality, presence of other credible nutrition actors, access constraints, and available resources. Outcomes for recovery, mortality, and defaulters surpassed SPHERE Minimum Standards in most programmes. Consequently, MSF recommends MUAC-based (and oedema) programming for most of its emergency responses, with ongoing review. Further research is needed on appropriate MUAC thresholds and how to ensure low WHZ only children receive appropriate nutrition support.
Globally, undernutrition is one of the single greatest threats to child survival, associated with 3.1 million child deaths each year – a half million from wasting – or 45 percent of all worldwide child deaths.1 Among those fleeing war and violence, both internally displaced persons (IDPs) and conflict-affected populations have highest rates of mortality and malnutrition, higher than among refugees.2
Since the successful introduction of outpatient nutritional rehabilitation in 2005, MSF has treated more than two million children for severe acute malnutrition in both acute emergency and chronic settings. More recently teams have increasingly explored strategies that are effective and yet simple to deploy, especially in situations with access constraints and limited health personnel. It was with this objective that teams in Upper Nile adopted MUAC (Mid upper arm circumference)-based programming in response to a dramatic situation unfolding in April 2014 in South Sudan’s Upper Nile State. Conflict sparked thousands of families to flee their homes. Illness and dramatic food insecurity combined to cause an expected spike in childhood malnutrition. Ongoing insecurity and severe logistic constraints drastically limited access – for aid workers and displaced alike.
To address acute malnutrition, emergency teams from Médecins Sans Frontières (MSF) adopted a simplified protocol in which Mid-Upper Arm Circumference (MUAC) was the only anthropometric measure used by therapeutic feeding programmes for admission, monitoring and discharge of malnourished children. (Bilateral pitting oedema is an independent criterion for malnutrition treatment regardless of anthropometry.) The usual admission criteria of MUAC <115 mm was expanded to admit all children with MUAC <125 mm, and children were discharged as cured when achieving MUAC >125 on two consecutive measurements (in addition to a minimum three-week stay in the programme.) Over the course of 22 weeks, more than 4,600 children were admitted for treatment, of which 1,395 were admitted in the initial five weeks of the intervention. All children with severe complications were hospitalised.
To date, MSF has also run such MUAC-based programmes in Titao and Yako (2007-2011), Burkina Faso; Bihar (2009-present) and Chattisgarrh (2013-present), India; Gedaref, Sudan (2010), Yida (2012), Agok (2012-2013), and Upper Nile (2014-present), South Sudan ; northern Mali (2012); Bokoro (2014) and Masakory (2011-2012), Chad; Bangui and Bossangoa (2014-present), Central African Republic (CAR); and Bolomba-Equateur (2014-2015) and Bili-Bas Huele (2015-present), Democratic Republic of Congo (DRC). This article shares experiences and lessons learned from this programming.
Use of MUAC as the sole anthropometric measure for admission, management and discharge
While further research is needed, there is a growing body of evidence that MUAC is safe and effective as the sole anthropometric criterion (along with oedema) used to identify, manage and discharge children requiring severe acute malnutrition (SAM) treatment.3 MUAC has been shown to be an as good as or a better predictor of mortality than weight-for-height z-scores (WHZ) <-3 or WHZ <-3 combined with MUAC, with an inherent age bias that targets younger children who are at highest risk of death.45678
Data analysis from MSF programmes in Burkina Faso and India showed that MUAC gains closely paralleled weight gain, suggesting that MUAC would work well for monitoring and discharge.910 A recent study from Malawi also showed that children with MUAC≥125 mm on two consecutive visits were safe for discharge, with acceptable negative outcomes at three months post-discharge.11 The World Health Organisation (WHO) recommends that “[T]he anthropometric indicator that is used to confirm severe acute malnutrition should also be used to assess whether a child has reached nutritional recovery.”12
In an MSF programme in Gedaref, Sudan, using MUAC for discharge resulted in children with lower MUAC at admission having a longer duration of treatment and a higher percent of weight gain than children with higher MUAC.13 In the Burkina Faso programme, switching to >124 mm MUAC instead of 10% weight gain for discharge resulted in a 36% increase in length of stay for the most malnourished and a 38% reduction in length-of-stay for the least malnourished.14 In other words, the most malnourished received the most treatment in both programmes. (Even though the WHO no longer recommends using 10% weight gain for discharge, this sharp reduction in the length of stay for the largest group of less malnourished children carried substantial operational and financial benefits).
One of the major concerns related to MUAC-only programming is the potential exclusion of children with MUAC >115 mm, but WHZ <-3.15 MSF has addressed this concern in some instances by increasing the MUAC threshold for admission. The threshold was, for example, increased to 120 mm in northern Burkina Faso and Bokoro, Chad and to 125 mm in Upper Nile, South Sudan (described above). This increases the number of children who benefit from therapeutic feeding while reducing the potential exclusion of children who are MUAC and WHZ discordant. In Dhaka, Bangladesh, MSF monitored children with MUAC > 115 mm but WHZ <-3 and found almost all of the children (93%) either improved in nutritional evolution or maintained a status-quo after three months’ follow up, without receiving any nutritional treatment.16 Few needed admission to a nutritional programme, although several had medical conditions that required hospitalisation irrespective of nutritional status, and only one death (from TB) occurred. More evidence on MUAC and WHZ discordant children is needed, especially for contexts in Africa.
Outcomes and practical lessons from MSF’s MUAC-based programming
Outcomes for recovery, mortality, and defaulters exceeded the Minimum Standards set by SPHERE in most of the MSF MUAC-based programmes reported here (see Table 1). High recovery rates (88- 90%) were achieved in the programmes in northern Burkina Faso, northern Mali, and Yida, South Sudan with lengths of stay in the order of 30-45 days. Of the children who died in the Burkina Faso programme from 2009-2011, nearly half had MUAC ≤110 on admission, stressing the importance of early identification. Many programmes were confronted with high default rates. In Bihar, India, however, most of the children who defaulted did so after obtaining six weeks’ worth of benefits from the programme.17 Teams there also identified risk factors for default (including more severe wasting on admission, commuting from outside of the programme location, and not having been referred by an Accredited Social Health Activist, among others) to help improve delivery of services. High default rates in Upper Nile, South Sudan and Bangui, CAR were attributed to continued population movements due to ongoing insecurity, and would have likely been high no matter the anthropometric measure used. Defaulting occurred more often among children in the moderate acute malnutrition (MAM) category, suggesting that adherence is perceived as less important once caretakers see their children noticeably improve.
Using MUAC as the sole anthropometric measure carried with it several practical advantages. Because MUAC is simpler and faster than WHZ (which requires two measurements and a calculation) it can facilitate better coverage, better management and earlier case detection at community level, as has been shown in Bangladesh when using active MUAC-based case detection.1819 Agencies like Alima and Befen are even showing that mothers can successfully use MUAC for screening at the household level.2021 With WHZ there are also questions over having different tables for girls and boys, whereas MUAC is gender neutral.22
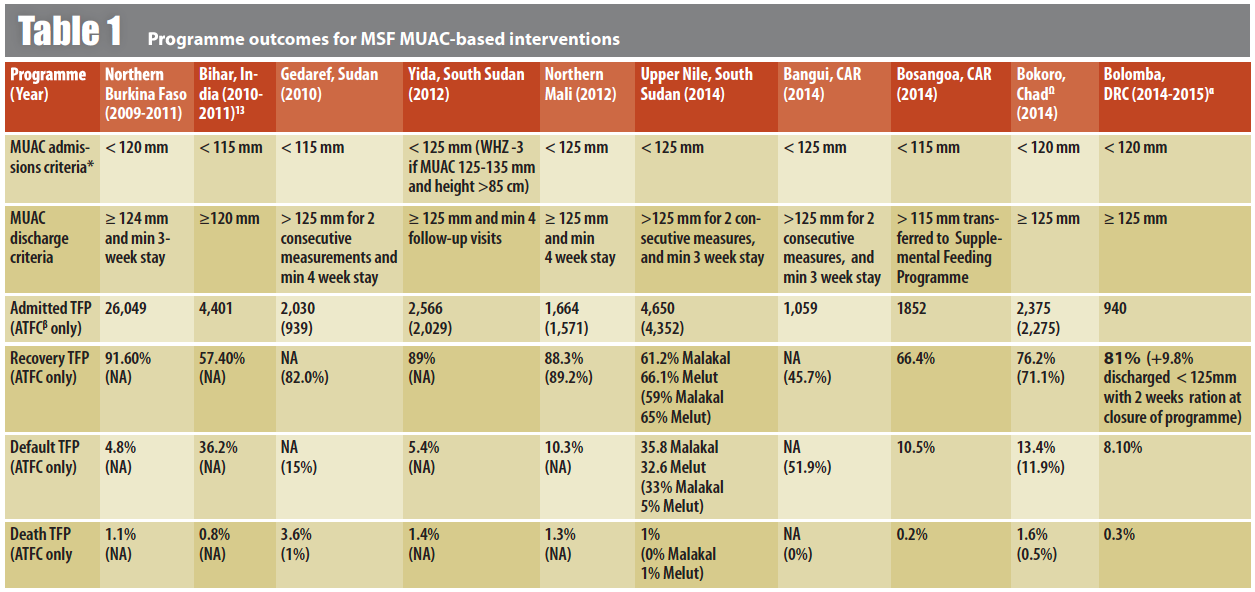
* Bilateral pitting oedema is an independent criterion for malnutrition treatment regardless of anthropometry
β ATFC = Ambulatory Therapeutic Feeding Centre
? Only includes data for August-October 2014 when MUAC-based programming was used
α Emergency intervention: ATFC only, Week 49 to week 06.
It was easier to implement and to train community health workers in the use of MUAC, relieving limited health structures and personnel of additional pressures. However, the reluctance of more experienced staff to only use MUAC proved to be a particular challenge because they were unsure of what would happen to children with low WHZ who may not be admitted. In a long-term programme in Masakory, Chad, training community health workers to manage treatment by MUAC (and oedema) helped improve coverage among families who live prohibitively far from health centres. And using the same criteria for screening as well as admission can help reduce “rejected” cases (i.e. children screened and referred based on MUAC but not admitted for treatment based on WHZ). This characteristic of MUAC-based programming may have even greater importance in settings of chronic malnutrition because of the negative perceptions such inconsistencies can create in a community.23
MUAC is also more adapted to community-based care, particularly in situations with severe access constraints for aid workers and caretakers alike, high food insecurity, or limited qualified staff dealing with multiple health priorities. Reaching children earlier on the spectrum of acute malnutrition prevents a slide into the most life-threatening form of SAM, potentially reducing the need for hospitalized care. Such a focus on preventive efforts has been reported to relieve pressure on overwhelmed doctors and nurses working in areas with limited medical capacity and many causes of illness.24
In the context of emergencies or population displacement, using MUAC as the sole anthropometric criterion facilitated a better flow of patients at the health structure level, reducing the time needed per child to identify the malnourished. The additional materials for measuring WHZ, like height boards and weight-for-height tables, insert extra, onerous steps in the screening and management that can introduce error. Of course accuracy questions arise with both types of anthropometric measurements. For MUAC, the strips can be pulled too tightly, left too loose, or misplaced on the child’s arm, whereas with WHZ, dehydration can affect the accuracy of weight or height measures2526(as can wriggling children), scales may not be properly calibrated, and errors can occur in calculation. Thus continued training and supervision is required for both. Supervision is simpler with MUAC, though, which is especially important during early stages of an intervention when staff are limited and less trained.
Notably, it is relatively easy to shift MUAC thresholds for admission or discharge according to context. Where there were high levels of under-5 mortality or severe food insecurity with few other actors present, using expanded criteria to treat SAM and MAM enabled teams to cover the most vulnerable children in both groups without needing to set up two different projects with separate products, criteria, and statistics, reducing the burden on the teams and staffing needs.
Moving forward
Based on the growing body of evidence and these experiences, MSF currently recommends that its teams use MUAC-based (and oedema) programming for most of its emergency responses. Although it requires continued discussion about benefits, risks, and costs, MUAC can be safe and effective as the only anthropometric measure for admission, management, and discharge. Further research is called for, especially on the question of appropriate MUAC thresholds and how to ensure those with low WHZ but not eligible by MUAC receive appropriate nutrition support.27For the moment, MSF will continue to adjust MUAC thresholds for admission according to contextual factors like prevailing mortality, presence of other credible nutrition actors, access constraints and available resources.
Building on these experiences and gathering more evidence about how to safely simplify the management of acute malnutrition will be important in the coming years, especially with situations like the one encountered in Upper Nile – conflict, displacement, difficult access, and limited personnel dealing with various health needs – becoming more common in contexts like CAR, DRC, South Sudan, northern Nigeria, Somalia, and elsewhere. While the benefits of a simpler, more decentralized approach is particularly relevant for improving coverage to prevent malnutrition-associated mortality or further deterioration into SAM in conflict settings, it also has clear implications for an improved response in areas of Africa (like the Sahel) and South Asia where recurrent emergencies result in high burdens of acute malnutrition.
For more information, contact: Saskia van der Kam, email: saskia.vd.kam@amsterdam.msf.org
1 Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, Webb P, Lartey A, Black RE. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost?The Lancet. 6 June 2013. DOI: 10.1016/S0140-6736(13)60996-4
2 Centre for Research on the Epidemiology of Disasters (CRED). People affected by conflict: Humanitarian needs in numbers. 2013. http://cred.be/sites/default/files/PAC2013.pdf
3 Roberfroid D, Hammami N, Lachat C, Prinzo ZW, Sibson V, Guesdon B, Goosens S, Kolsteren P. Utilisation of mid-upper arm circumference versus weight-for-height in nutritional rehabilitation programmes: a systematic review of evidence. WHO. 2013.
4 Myatt M, Khara T, Collins S. A review of methods to detect cases of severely malnourished children in the community for their admission into community-based therapeutic care programmes. Food and Nutrition Bulletin. 2006 Sep; 27 (3 Suppl): S7-23).
5 Briend A, Maire B, Fontaine O, Garenne M. Mid-upper arm circumference and weight-for-height to identify high-risk malnourished under-?ve children. Matern Child Nutr. 2012 Jan;8(1):130-3. doi: 10.1111/j.1740-8709.2011.00340.x.
6Briend A. Use of MUAC for Severe Acute Malnutrition. CMAM Forum. 2012. http://www.cmamforum.org/Pool/Resources/FAQ-1-Use-of-MUAC-Briend-Eng-June-2012%281%29.pdf
7Mwangome MK, G Fegan, T Fulford, AM Prentice, JA Berkley. Mid-upper arm circumference at age of routine infant vaccination to identify infants at elevated risk of death: a retrospective cohort study in the Gambia. Bull World Health Organ 2012;90:887–894 | doi:10.2471/BLT.12.109009
8Briend A, Khara T, and Dolan C. Wasting and stunting—similarities and differences: Policy and programmematic implications. Food and Nutrition Bulletin, vol. 36, no. 1. 2015 (supplement).
9Goossens S, Bekele Y, Yun O, Harczi G, Ouannes M, Shepherd S. et al. Mid-Upper Arm Circumference Based Nutrition Programming: Evidence for a New Approach in Regions with High Burden of Acute Malnutrition. PLoS ONE 2012; 7(11): e49320. doi:10.1371/journal.pone.0049320.
10 Burza S, Mahajan R, Marino E, Sunyoto T, Shandilya C, Tabrez M, Kumari K, Mathew P, Jha A, Salse N, and Mishra KN. Community-based management of severe acute malnutrition in India: new evidence from Bihar. Am J Clin Nutr First published February 25, 2015, doi: 10.3945/?ajcn.114.093294
11 Binns, Paul et al.. Safety of Using Mid-Upper Arm Circumference as a Discharge Criterion in Community-Based Management of Severe Acute Malnutrition in Children Aged 6–59 Months. Oxford, England: Valid International 2014.
12 World Health Organization. Guideline: Updates on the management of severe acute malnutrition in infants and children. Geneva: WHO; 2013. www.who.int/nutrition/publications/guidelines/updates_management_SAM_infantandchildren/en/index.html
13 Dale NM, Myatt M, Prudhon C, Briend A. Using mid-upper arm circumference to end treatment of severe acute malnutrition leads to higher weight gains in the most malnourished children. PLoS One. 2013;8(2):e55404.
14 Cohuet S, Goosens S, Koudika MH, Shepherd S, Martinez D, Munger A, Porten K. Comparison of MUAC and percent weight gain as discharge criterion in a large TFP programme in Burkina Faso 2007-2011. Poster session presented at: International Congress of Pediatrics – ICP 2013. 27th International Pediatric Association Congress of Pediatrics - IPA 2013; 2013 Aug 24-29; Melbourne, Australia.
15 Grellety E, Krause LK, Shams Eldin M, Porten K, Isanaka S. Comparison of weight-for-height and mid-upper arm circumference (MUAC) in a therapeutic feeding programmes in South Sudan: is MUAC alone a su?cient criterion for admission of children at high risk of mortality? Public Health Nutr. 2015 Mar 25:1-7. [Epub ahead of print] doi: 10.1017/S1368980015000737 PMID:2580527
16Ali E, Zacharia R, Shams Z et al. Is Mid Upper Arm Circumference sufficient for case-finding and admission of children with severe acute malnutrition into nutritional support programmes in an urban slum in Dhaka, Bangladesh? Trans R Soc Trop Med Hyg, 6 February 2013.
17 Burza S, Mahajan R, Marino E, Sunyoto T, Shandilya C, Tabrez M, Kumari K, Mathew P, Jha A, Salse N, and Mishra KN. Community-based management of severe acute malnutrition in India: new evidence from Bihar. Am J Clin Nutr First published February 25, 2015, doi: 10.3945/?ajcn.114.093294.
18 Sadler K, Puett C, Mothabbir G, and Myatt M. Community Case Management of Severe Acute Malnutrition in Southern Bangladesh. Save the Children and Feinstein International Center. June 2011. Available online at: http://fic.tufts.edu/publication-item/community-case-management-of-severe-acute-malnutrition-in-southern-bangladesh/. Accessed 8 April 2015.
19 Puett C, Coates J, Alderman H, Sadler K. Quality of care for severe acute malnutrition delivered by community health workers in southern Bangladesh. Matern Child Nutr. 2013; 9:130-42
20 Blackwell N, Myatt M , Allafort-Duverger T , Balogoun A , Ibrahim A , Briend A. Mothers understand and can do it: a comparison of mothers and community health workers determining mid-upper arm circumference in 102 children aged from 6 5 months to 5 years. Archives of Public Health, 2015 May 18;73(1):26. doi: 10.1186/s13690-015-0074-z. eCollection 2015
21 Equipe BEFEN ALIMA. Final Report: Evaluation du recrutement en programmeme nutritionnel therapeutique a travers deux strategies de depistage communautaire en milieu rural au sud du Niger. September 2014. Personal correspondence
22 Moestue H, de Pee S, Hall A, Hye A, Sultana N, Ishtiaque MZ, Huq N, Bloem MW. Conclusions about differences in linear growth between Bangladeshi boys and girls depend on the growth reference used. Eur J Clin Nutr 2004;58:725–31.
23 Guerrero S, Myatt M, Collins S. Determinants of coverage in Community-based Therapeutic Care programmemes: Towards a joint quantitative and qualitative analysis. Disasters 2009; 34(2):571-585
24 War, Drought, Malnutrition, Measles — A Report from Somalia. Jean-Clement Cabrol, M.D.N Engl J Med 2011; 365: 1856-1858November 17, 2011DOI: 10.1056/NEJMp1111238
25 Mwangome MK, Fegan G, Prentice AM, Berkley JA. Are diagnostic criteria for acute malnutrition affected by hydration status in hospitalized children? A repeated measures study. Nutr J. 2011 Sep 13;10:92. doi: 10.1186/1475-2891-10-92.
26 Modi P, Nasrin S, Hawes M, Glavis-Bloom J, Alam NH, Hossain MI, Levine AC.Midupper Arm Circumference Outperforms Weight-Based Measures of Nutritional Status in Children with Diarrhea. J Nutr. 2015 May 13. pii: jn209718. [Epub ahead of print]
27 Grellety E, Krause LK, Shams Eldin M, Porten K, Isanaka S. Comparison of weight-for-height and mid-upper arm circumference (MUAC) in a therapeutic feeding programme in South Sudan: is MUAC alone a su?cient criterion for admission of children at high risk of mortality? Public Health Nutr. 2015 Mar 25:1-7. [Epub ahead of print] doi: 10.1017/S1368980015000737 PMID:2580527


