Evaluation of an integrated health-nutrition-WASH project to reduce malnutrition prevalence in children under two in Bangladesh
By Monsurul Hoq and John Brogan
Monsurul Hoq was working as a Statistician Epidemiologist during the study. He has experience in monitoring and evaluation of community-based health and nutrition projects in South Sudan and Bangladesh. He is currently working as a Biostatistican at Murdoch Children’s Research Institute in Australia.
John Brogan supports communities in low- and middle-income countries, specialising in WASH and DRR. Currently based in Lausanne, he was Country Representative for Terre des Hommes (TDH) in Bangladesh and Myanmar from 2011 to 2014.
Terre des Hommes appreciates the approval and cooperation of the national and local structures of the Government of Bangladesh and the financial support of the Swiss Agency for Development and Cooperation, Swiss Solidarity, UNICEF, the World Food Programme and the European Commission. We extend thanks to Shahid Kamal, Pranab Kumar Roy, Laxman Kharal Chettry and the TDH team in Kurigram for project cycle management support and to Dr. Charulatha Banerjee, Ibrahima Diallo, Marie-Jeanne Hautbois and Mark Myatt for their technical support. Finally, we are grateful to the caregivers and community members of Kurigram Municipality, without whose courage and cooperation this project would have not been possible.
Location: Bangladesh
What we know: Poor water, sanitation and hygiene (WASH) is recognised as an underlying contributor to acute malnutrition. Evidence of impact of WASH interventions on undernutrition is limited.
What this article adds: An opportunistic comparison of an integrated WASH intervention site (infrastructure and intensified hygiene) with a comparison site was carried out by TDH in a peri-urban area of Kurigram Municipality, Bangladesh, based on service data available from a community health project over three years. While acute malnutrition prevalence (MUAC <125mm) fell in both sites, the rate of change was significantly higher in the intervention site. A proportional reduction in underweight was similar in both sites. Further research is required to explore context and mechanisms of impact of WASH interventions on nutrition.
Introduction
 According to UN estimates, in 2011 more than 100 million children under five worldwide (15.7%) were underweight and more than 70% of the world’s wasted children live in Asia; most in south-central Asia, where an estimated 10.1% (36.1 million) are affected (Black et al, 2013). Rates of malnutrition are also of concern in Bangladesh; the prevalence of acute malnutrition, defined by weight-for-height z-score (WHZ) < -2, is 11% in northern Bangladesh (FSNSP, 2013).
According to UN estimates, in 2011 more than 100 million children under five worldwide (15.7%) were underweight and more than 70% of the world’s wasted children live in Asia; most in south-central Asia, where an estimated 10.1% (36.1 million) are affected (Black et al, 2013). Rates of malnutrition are also of concern in Bangladesh; the prevalence of acute malnutrition, defined by weight-for-height z-score (WHZ) < -2, is 11% in northern Bangladesh (FSNSP, 2013).
The causal path of malnutrition is complex where biological, cultural and socio-economic factors are interrelated. As described by UNICEF, the causal path of malnutrition is multi-factorial; inadequate dietary intake and disease are considered as immediate causes and poor sanitation and hygiene practice as one of the underlying causes of malnutrition in developing countries (SOWC, 1998). According to WHO (2008), half of malnutrition is associated with repeated diarrhoea or intestinal worm infection due to unsafe drinking water, inadequate sanitation and lack of hygiene practices. In order to improve this situation, the recent Lancet series recommends WASH interventions as one of several interventions (Bhutta et al, 2013). The Lancet in 2009 hypothesised that prevention of tropical enteropathy will be crucial to normalise child growth and will not be possible without access to toilets (Humphrey, 2009). A systematic review by the London School of Hygiene and Tropical Medicine of available evidence on the effect of WASH on nutrition status of children also found a small benefit of WASH intervention on length growth in children under five (Dangour et al, 2013). Though there is need for better evidence to explore the impact of WASH interventions on undernutrition, there are few rigorous trials due to low priority given to WASH in medical research (Velleman et al, 2013).
The study described in this article reports the changes in prevalence of malnutrition, comparing an integrated WASH intervention site and a comparison site, based on service data available from a community health project in a peri-urban area of Kurigram Municipality. Acute malnutrition was defined by mid-upper arm circumference (MUAC) < 125mm and underweight as weight-for-age z score (WAZ) < -2, which were compared separately over time.
Methodology
Sites and target population
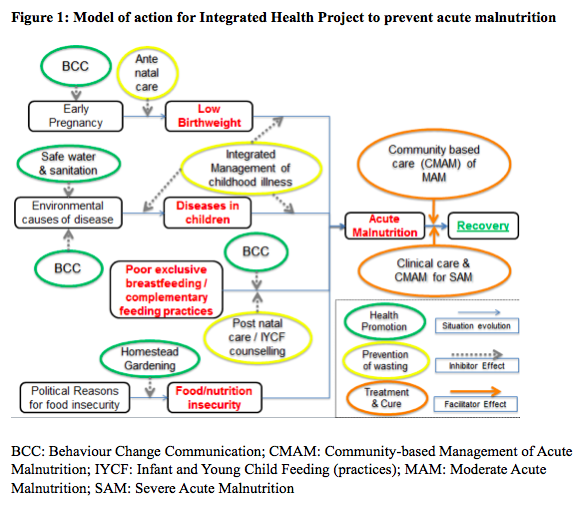
From November 2011 to December 2014, TDH implemented a comprehensive health and nutrition services project in line with Bangladesh’s National Nutrition Service Operational Plan for women, infants and young children living in the nine wards of Kurigram Municipality of Kurigram District, northern Bangladesh (see model of action in Figure 1). The households were typically of low socio-economic status; poor environmental sanitation and food hygiene, as well seasonal flooding, were also common issues in the area. Due to resource limitations, WASH activities were integrated in only two of the nine Wards - an intervention justified by the high prevalence of acute malnutrition among children under five years of age (29.0% prevalence of MUAC <125mm and 30.1% with WAZ < - 2). The two wards were also among the areas of highest flood risk in the municipality. This project was later identified as an opportunity to evaluate the integration of WASH activities within a community-based health project aimed at reducing child malnutrition.
Interventions
Of Kurigram Municipality’s nine wards, the two with the highest prevalence of acute malnutrition were selected for installation of WASH infrastructures and intensified hygiene awareness within the community-based health project and considered as the intervention site. The remaining seven wards became the comparison site, having similar ecological and demographic characteristics, childcare practices, and hygiene behaviour and sanitation coverage. Over the project period, no other development projects were implemented in either of the sites. A summary of activities implemented in the intervention and comparison sites is given in Table 1.
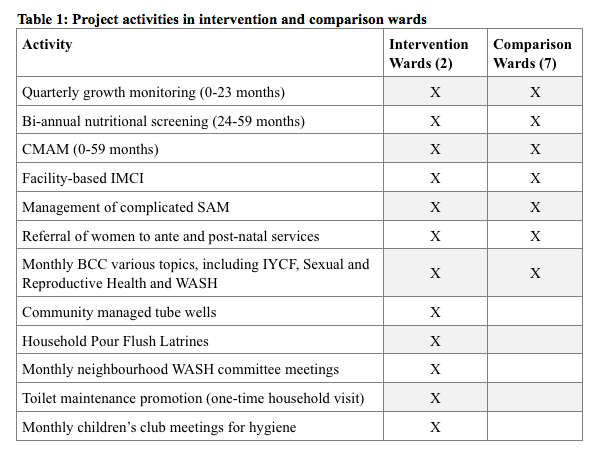
The community-based health project activities included growth monitoring of children under two years; community management of acute malnutrition (CMAM) of children under five; facility-based Integrated Management of Childhood Illness (IMCI) and management of complicated cases of severe acute malnutrition (SAM); identification of pregnant and lactating women and referral for antenatal and postnatal care; and behaviour change communication (BCC) on infant and young child feeding (IYCF) practices and reproductive health-related issues, including early marriage and family planning. CMAM activities were implemented in TDH-run maternal and child health centres and TDH-run community-based outpatient therapeutic programme (OTP) centres at household level.
 WASH-focused activities included construction of 119 community-managed, deep-tube wells and 1,280 household pour-flush twin pit latrines (offset and direct-drop pits according to space constraints). Well and latrine structures were raised to reduce the risk of inaccessibility during flooding. During the project, monthly campaigns for BCC to improve environmental hygiene were common to all nine wards. Beginning with Participatory Hygiene and Sanitation Transformation (WHO, 1998), follow-up activities included mothers’ group discussions, public theatre, music, songs, and visual education materials as media. Topics and messages focused on the importance of hand-washing, safe drinking water and excreta disposal, household environmental hygiene, and diarrhoea prevention. In addition, project staff organised monthly children’s club meetings and individual household visits to promote proper use and maintenance of the newly-installed infrastructure.
WASH-focused activities included construction of 119 community-managed, deep-tube wells and 1,280 household pour-flush twin pit latrines (offset and direct-drop pits according to space constraints). Well and latrine structures were raised to reduce the risk of inaccessibility during flooding. During the project, monthly campaigns for BCC to improve environmental hygiene were common to all nine wards. Beginning with Participatory Hygiene and Sanitation Transformation (WHO, 1998), follow-up activities included mothers’ group discussions, public theatre, music, songs, and visual education materials as media. Topics and messages focused on the importance of hand-washing, safe drinking water and excreta disposal, household environmental hygiene, and diarrhoea prevention. In addition, project staff organised monthly children’s club meetings and individual household visits to promote proper use and maintenance of the newly-installed infrastructure.
Data collection
As part of the community-based health project, a survey was conducted including all nine wards of Kurigram Municipality at the end of first year of the project (December 2012). The survey findings were used as a secondary source to compare socio-economic status, disease prevalence, healthcare-seeking behaviour and coverage of water and sanitation facilities between the sites.
In order to assess the nutritional status of children under two, weight and MUAC were measured by project staff every three months through growth-monitoring sessions in designated places of the community in each of the nine wards. There were 15 centres in the intervention site and 18 centres in the control site. Children living in the neighbourhood came to the area for screening on the scheduled day of the session. The campaign team also visited households in the neighbourhood to ensure all listed children were measured. If any children missed the session, the project staff visited the households to ensure these children were included. The children born during the project period were included for screening and children over two were excluded. The number of children measured quarterly between March 2012 and December 2014 in nine wards ranged from 132 (6.47%) to 875 (42.01%) of 2,037 children registered during the project period. The ratio of children measured between the intervention and comparison sites was 1:1, similar to the ratio of total children under two in both sites. There was no significant difference in average age (in months) of children between the sites and ratio of girls and boys was 1:1 in all quarters.
Children’s weight was measured using digital machines (Digital Lithium Scale, HD-318, Highest 150kg, China) with a precision of 100g and MUAC was measured by MUAC tape (S0146520 MUAC Child 11.5Red/PAC-50, UNICEF). All measurements were made in line with WHO standard protocols (SMART, 2006). WAZ was calculated according to WHO’s growth standard of WAZ by sex using Emergency Nutrition Assessment for SMART software (WHO, 2006; ENA, 2009) and WAZ < - 5 or WAZ > 5 was considered as flagging criteria. Children with WAZ < -2 were identified as underweight, while children with MUAC < 125mm were identified as acutely malnourished. All project staff received training on anthropometric measurement as part of the project and were refreshed as appropriate. The project-monitoring staff measured children at random and cross-checked with project staff ensuring quality of the data, as well as checking age and sex distribution, digit preference and clustering effect. This service data was used to address the study objective.
Analysis
 The socio-economic, health and hygiene characteristics of the intervention and comparison sites were compared using an appropriate statistical test (i.e. z-test) to confirm they were similar at baseline. In order to address the study objective, prevalence of underweight defined by WAZ < -2 and prevalence of acute malnutrition defined by MUAC < 125mm were estimated for each quarter compiling growth monitoring data of children under two. Linear regression analysis was conducted, estimating rate of change in prevalence of malnutrition during 2012 – 2014 (i.e. regression coefficient of time) in intervention and comparison sites separately and compared using the Wald test between the two sites. All data were entered and analysed using IBM SPSS Statistics for Windows (IBM, 2010).
The socio-economic, health and hygiene characteristics of the intervention and comparison sites were compared using an appropriate statistical test (i.e. z-test) to confirm they were similar at baseline. In order to address the study objective, prevalence of underweight defined by WAZ < -2 and prevalence of acute malnutrition defined by MUAC < 125mm were estimated for each quarter compiling growth monitoring data of children under two. Linear regression analysis was conducted, estimating rate of change in prevalence of malnutrition during 2012 – 2014 (i.e. regression coefficient of time) in intervention and comparison sites separately and compared using the Wald test between the two sites. All data were entered and analysed using IBM SPSS Statistics for Windows (IBM, 2010).
The intervention was approved by the NGO Affairs Bureau of Bangladesh. The identity of the children was anonymised and all malnourished children were enrolled in TDH-supported facilities. The OTP centres were independent of the state system but implemented with the necessary permissions. With the government subsequently moving to scale up CMAM rollout within the state health system, TDH has a Memorandum of Understanding with Institute of Public Health Nutrition of the Ministry of Health & Family Welfare to coordinate the rollout in Kurigram District.
Results
Socio-economic, health and hygiene characteristics
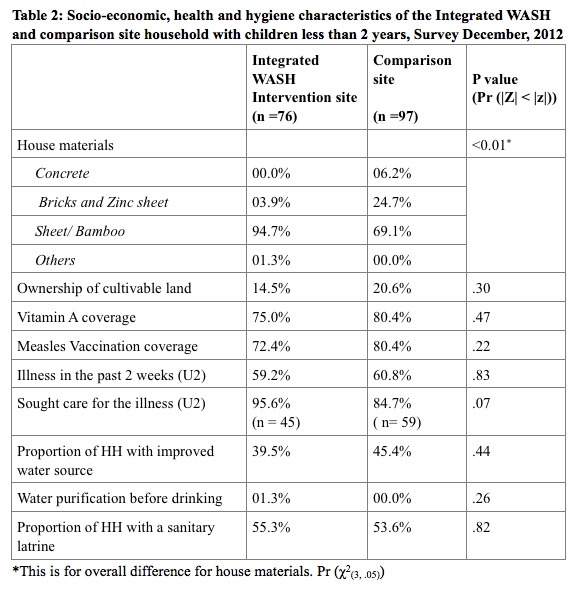
The socio-economic, health and hygiene characteristics of the integrated WASH intervention site and comparison site of children under two are summarised in Table 2. The survey confirmed that characteristics of the intervention site were broadly similar to the comparison site at the end of the first year of the project. The intervention site was similar to the comparison site in terms of ownership of cultivable land and coverage of improved water source, water purification and sanitary latrines. However, in the intervention site, more households were living in shelters built by zinc sheeting or bamboo (94.7%) compared to the comparison site (69.1%). Among children under two, Vitamin A and measles vaccination coverage and prevalence of illness in the past two weeks of survey were similar in the two sites. However in the intervention area, caregivers sought care more frequently than in comparison area (diff .11, 95% CI .01 - .22, p <.07).
Between site comparison of prevalence of malnutrition
At the outset of the project (March 2012), the prevalence of underweight was higher in the intervention site (30.1% compared to 22.7%). Figure 2 reflects how the percentage of underweight children reduced over time in both sites, but the proportional difference remained consistent over time and between sites. Similarly in March 2012, the prevalence of acute malnutrition was higher in the intervention site (29.0% compared to 12.7). However, the difference in proportion reduced over time between sites, due to a greater fall in prevalence in the intervention site (see Figure 3).
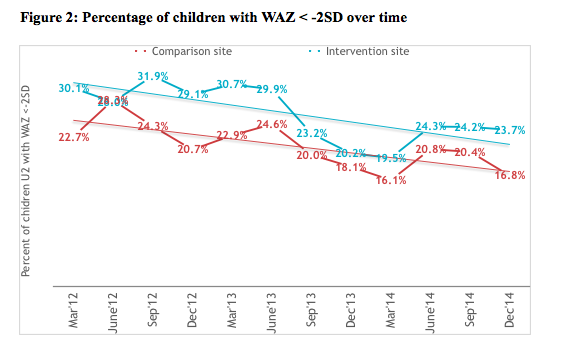
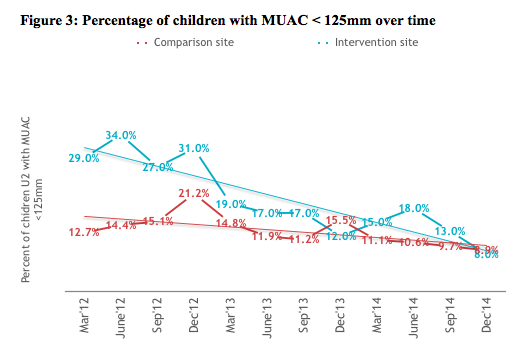
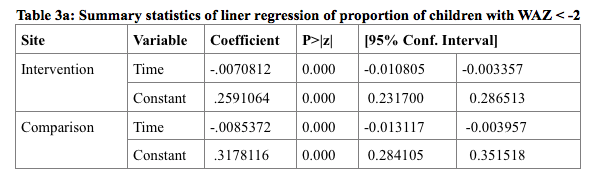
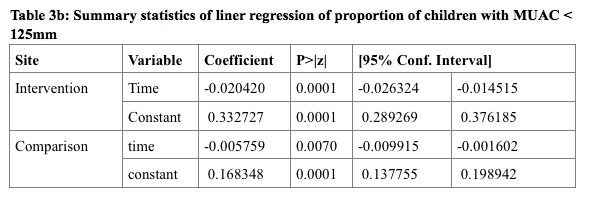
The prevalence of underweight among children under two in the intervention site reduced by 0.007% (95% CI .003% - .011%) and in the comparison site by 0.008% (95% CI .004% - .013%) over time. There was no significant difference in the rate of change over time between the two sites (chi2 (1) =.46, p-value =.4969) (Table 3a). However similar analysis of prevalence of acute malnutrition reveals that the rate of change was significantly higher (chi2 (1) =20, p-value =.0001) in the integrated WASH intervention site (.020%, 95% CI .014% - .026%) compared to comparison site (.006%, 95% CI .002% - .010%) (Table 3b).
The increase in household coverage for improved toilets is estimated at 29.4%, while household access to improved water source increased by 27.6%.
Discussion
The study findings suggest that the percentage of children with WAZ < -2SD reduced in both intervention and comparison sites but there was no significant difference in improvement between both sites. One possible reason for the result could be the effectiveness of growth-monitoring activities (that included BCC and cooking demonstrations) as part of the community-based health project, which was implemented in all nine wards. Similarly, a longitudinal study in rural Bangladesh has found behavioural change intervention effective in reducing percentage of children with WAZ < - 3SD (Nasar et al, 1993). However, Dangour et al (2013) in a review of 14 studies reported no evidence of effect of WASH intervention on WAZ.
 In Bangladesh diarrhoea is a major contributor to malnutrition. Poor hygiene practice and environmental sanitation are major contributors of diarrhoea. However, it was not possible to examine the effect of the intervention on diarrhoeal or water-related diseases rates due to lack of project data (morbidity data is collected in hard copy only; electronic data are only available on the number of children under five who came to the TDH-run satellite clinics).
In Bangladesh diarrhoea is a major contributor to malnutrition. Poor hygiene practice and environmental sanitation are major contributors of diarrhoea. However, it was not possible to examine the effect of the intervention on diarrhoeal or water-related diseases rates due to lack of project data (morbidity data is collected in hard copy only; electronic data are only available on the number of children under five who came to the TDH-run satellite clinics).
A randomised intervention trial was beyond the scope of this project, since this study was planned after project completion in 2014 and used available project data to evaluate the impact. The selection of the wards as intervention sites was justified by high percentages of children with WAZ < - 2SD and/or MUAC < 125mm which increases the probability that measureable difference after the project would be attributed to the intervention rather than to site differences.
The methodology of inclusion and exclusion of children minimised maturation effect as children grow older and ensured similar distribution of children by age over the three-year duration. The designated places of conducting growth monitoring session were distributed throughout the community which reduced bias in selection of children based on location. As part of the community-based health project, project staff working in rotation measured the children which minimised enumerator bias.
 The study shows evidence of the positive effect of integration of WASH activities within the community-based health project in reducing acute malnutrition defined by MUAC. The intervention comprised infrastructure and intensified hygiene awareness over the comparison sites. There are no studies showing the impact of WASH interventions on acute malnutrition. However further research is required to examine the impact of WASH on children’s nutritional status, taking into consideration the context and explanation for the most effective components and the mechanisms.
The study shows evidence of the positive effect of integration of WASH activities within the community-based health project in reducing acute malnutrition defined by MUAC. The intervention comprised infrastructure and intensified hygiene awareness over the comparison sites. There are no studies showing the impact of WASH interventions on acute malnutrition. However further research is required to examine the impact of WASH on children’s nutritional status, taking into consideration the context and explanation for the most effective components and the mechanisms.
For more information, contact: John Brogan.
References
Bhutta, Zulfiqar A., et al (2013). Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? The Lancet Vol 382, Issue 9890: 452-477.
Black, Robert E. et al (2013). Maternal and child undernutrition and overweight in low-income and middle-income countries, The Lancet Vol 382, Issue 9890 427 - 451
Dangour A.D., Watson L., Cumming O., Boisson S., Che Y., Vellemen Y., et al (2013). Interventions to improve water quality and supply, sanitation and hygiene practices, and their effects on the nutritional status of children (Review). The Cochrane Library. 2013; Issue 8. Retrieved 29 March 2015 from www.thecochranelibrary.com.
ENA software for SMART (2009). Retrieved March 2015 from www.smartmethodology.org/survey-planning-tools/smart-emergency-nutrition-assessment/.
FSNSP (2013). The Food Security and Nutrition Survillance Project: Results from Round 10: February to April, 2013. BRAC University, HKI & Bangladesh Bureau of Statistics.
Humphrey J.H. (2009). Child under-nutrition, tropical enteropathy, toilets, and handwashing. The Lancet, 374: 1032–35
IBM Corp (2010). IBM SPSS Statistics for Windows, Version 19.0. Armonk, NY: IBM Corp.
Nasar U., Marian F., Alexa S., Charles M., Stanley N. (1993). A longitudinal study of the impact of behavior change intervention on cleanliness, diarrhoeal morbidity and growth of children in rural Bangladesh. Soc Sci Med. Vol 37. No. 2, pp. 159-171.
SMART (2006). Measuring Mortality, Nutritional Status, and Food Security in Crisis Situations: SMART Methodology. Version 1. Retrieved March 2015 from www.smartmethodology.org
SOWC – State of the World’s Children (1998). UNICEF conceptual framework.
WHO Multicentre Growth Reference Study Group (2006). WHO Child Growth Standards based on length/height, weight and age. Acta paediatrica (Oslo, Norway: 1992). Supplement, 450, 76.
Wood S, Sawyer R, Simpson-Hebert M. (1998). PHAST step-by-step guide: a participatory approach for the control of diarrhoea disease. Geneva, World Health Organisation (unpublished document WHO/EOS/98.3)
WHO (2008). Safer water, better health: Costs, benefits and sustainability of interventions to protect and promote health. Retrieved from www.whqlibdoc.who.int/
Yael Velleman, Isabelle Pugh (2013). Under-nutrition and water, sanitation and hygiene, WaterAid, The London School of Hygiene and Tropical Medicine and Share.


