Stunting and wasting in children under two years old in a semi-nomadic pastoralist population in Kenya
By Amelia Reese-Masterson, Masumi Maehara and Mark Murage Gathii
Amelia Reese-Masterson is Research Advisor in the Nutrition, Food Security and Livelihoods Unit at International Medical Corps. She has over six years’ experience in applied maternal and child health and nutrition research and programming. She holds an MPH from Yale School of Public Health, with a focus on nutritional epidemiology.

Mark Murage Gathii is Monitoring and Evaluation Officer for International Medical Corps, Kenya. He holds a Bachelor of Science in nutrition and has seven years’ experience in nutrition assessments, including SMART and SQUEAC, and social research.
Masumi Maehara is Maternal and Neonatal Nutrition Consultant for United Nations Population Fund Somalia Country Office. She holds a Bachelor’s degree in Public Health and International Relations and an MSc. in Nutrition in Global Health from the London School of Hygiene and Tropical Medicine.
The authors acknowledge funding support from UNICEF, the technical support of the NIWTG, the Ministry of Health, Samburu County, and Philip James of the London School of Hygiene and Tropical Medicine for technical support.
Location: Kenya
What we know: The relationship between stunting and wasting in children has been poorly investigated.
What this article adds: A secondary analysis of SMART survey data investigated socio-economic and health-related risk factors associated with stunting, wasting and both combined in 227 children aged 6-23 months in a poor, pastoralist Kenyan community. Stunting prevalence was 28.19%; wasting prevalence was 8.8% (WHZ) and 1.32% (MUAC <11.5 cm). In univariate logistic regression analysis, (lack of) hand-washing at four critical moments, having had fever or malaria in the past two weeks, and child age, were associated with stunting. In multivariate logistic regression analysis, no variable was significantly associated with stunting. Having access to toilet facilities was weakly associated with wasting. Children with concurrent wasting and stunting were significantly more likely to come from a household without any livestock ownership (p=0.03). The correlation between stunting and wasting was low at 5%. The analysis was limited (cross-sectional data does not capture seasonal trends; this secondary data analysis may have lacked statistical power). The authors recommend programme-specific data and measurement-related improvements to SMART to enable more meaningful analysis.
Background
While the prevalence of stunting and wasting in children under five has been decreasing globally over the past two decades, the 2013 Lancet series of Maternal and Child Nutrition estimated that stunting still affected at least 165 million children and wasting still affected at least 52 million children under five years old in 2011. United Nations Children’s Fund (UNICEF), World Health Organization (WHO) and the World Bank estimated that in 2012, 36% of all stunting cases occurred in Africa, (UNICEF, WHO & World Bank, 2016) with East Africa facing the heaviest burden of stunting. (Black, Victora, Walker et al, 2013).
Wasting prevalence in Kenya at the time of programme launch was at 7% (KDHS 2010), with children aged 6-8 months having the highest prevalence (11%) (KDHS 2010). The prevalence of stunting among children under five was 35%, with children aged 18-23 months having the highest prevalence (46%) and children less than six months having the lowest (11%) (KDHS 2010).While stunting rates declined between 2000 and 2008 by approximately 17%, since then the prevalence has not changed substantially (KDHS 2010).With an estimated 2.1 million children under five years old being stunted in Kenya and wasting prevalence as high as 20% in one province in the country, the Kenyan Government initiated the High Impact Nutrition Interventions (HiNi), based on evidence from the Lancet Series on Maternal and Child Nutrition (2008) (MPHS, 2012). Eleven of the 13 recommended interventions were chosen by the Government as relevant to the country’s nutrition challenges: breastfeeding promotion, complementary feeding promotion for infants after six months, improved WASH (water, sanitation and hygiene) practices, vitamin A supplementation for children, therapeutic zinc supplementation for diarrhoea management, deworming, iron-folic acid supplementation for pregnant women, salt iodisation, multiple micronutrient fortification, prevention of acute malnutrition, and treatment of acute malnutrition.
The analysis presented in this article focuses on Samburu County, one of the poorest counties in Kenya and home to a semi-nomadic, pastoralist population. International Medical Corps has been supporting HiNi in Samburu County since 2011. The County is located in the Rift Valley region and is characterised by arid and semi-arid lands; suffering from unreliable rainfalls, droughts and floods, it is prone to malnutrition. Even after the implementation of the HiNi, stunting and wasting persist. The prevalent malnutrition issues and limited data on the impact of HiNi in the County led us to undertake further analysis of Standardized Monitoring and Assessment of Relief and Transitions (SMART) data from Samburu County, where these interventions have been implemented. We explored the relationship between stunting and wasting in what is one of the poorest counties in Kenya to disentangle this relationship and provide concrete recommendations to address both.
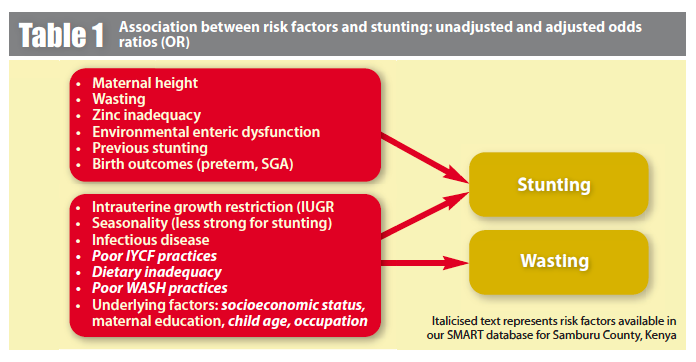
The relationship between stunting and wasting has been poorly investigated. Stunting and wasting are generally treated as two separate and distinct conditions in nutrition programming, policy, and funding streams (Khara & Dolan, 2014). While causes of wasting are clearer due to a larger body of research, a number of causes of stunting have also been identified in previous research. The two forms of malnutrition share many causes (see Figure 1) and can co-occur in the same country, region or even the same child. Wasting has, in fact, been identified as a potential risk factor for stunting.
The overall aim of this analysis was to identify socio-economic and health-related risk factors associated with stunting and wasting in children aged 6-23 months in the Samburu population. Specific objectives included:
- To investigate factors (and effect size) associated with stunting, wasting and both combined;
- To investigate the relationship between stunting and wasting; and
- To provide evidence-based recommendations to inform nutrition programmes in this population/region.
Study methods
Data from a cross-sectional SMART nutrition survey, carried out by International Medical Corps in 2013, were used for a secondary data analysis. This SMART survey was conducted between 7 and 16 January 2013 among the semi-nomadic, pastoralist population in Samburu East and North districts. It assessed the effect of the HiNi programme on maternal and child health in Samburu. The survey questionnaire was adjusted to the Kenyan context using guidelines provided by the Nutrition Information Technical Working Group (NITWG), in partnership with the Ministry of Public Health and nutrition sector partners. Specifically, the survey captured anthropometrics of children aged 6-59 months, child mortality rate, infant and young child feeding (IYCF) practices among those aged 6-23 months, exclusive breastfeeding rates among infants under six months, maternal healthcare and child care practices, WASH, and demographic and household characteristics of the nomadic pastoralist population. It was conducted during the dry season. Data were collected by trained enumerators under the guidance of a team leader, entered by trained data entry clerks.
A two-stage cluster sampling methodology was used to sample participants in the original survey. The first stage involved cluster sampling based on probability proportional to population size of clusters. Villages were used as clusters. All the clusters and their population sizes were derived from the 2009 Kenya Census Report (KNBS, 2009). The second stage involved simple random sampling of households from each cluster. Households were identified by creating a list of all the households with the help of village guides. For the original survey, sample size was calculated based on the global acute malnutrition (GAM) prevalence of 21.5% in 2011 in Samburu, precision of 4.5, a design effect of 1.5, an average household size of 5.4 people, and an estimated non-response rate of 4%, which resulted in 36 clusters and 18 households from each cluster. For the purpose of this present analysis, only participants from the original survey that met the eligibility criteria outlined below were included in the analysis.
The predictors of stunting (length-for-age z-score (LAZ) <-2) and wasting (weight-for-length z-scores (WLZ) <-2) were explored through a secondary data analysis. All analyses were adjusted for the complex survey design used during the SMART survey. For stunting, univariate logistic regression analysis was conducted to obtain unadjusted odds ratios. Variables identified to be associated with stunting (p<0.10) were taken forward to multivariate logistic regression analysis. Child age, sex and occupation of the household head were forced into the final logistic regression model. Adjusted Wald tests were performed to investigate which variables were associated with stunting (p<0.05). For wasting, the number of children with this condition was low, so using logistic regression was not appropriate. Instead, chi-squared tests were used to see the association with exposure variables and the significance level was set at 0.10. Since the Samburu are a pastoral population and pastoralists have been shown to be taller and leaner than sedentary populations, mid-upper arm circumference (MUAC) was also used as a substitute for WLZ to determine wasting prevalence. Correlation between stunting and wasting was explored using Pearson’s correlation coefficient.
Findings
Of 227 children, 120 (52.86%) were boys. Median age was 17 months (IQR=11, 21 months). There was no difference between boys and girls in height or weight (p-values=0.37 and 0.24, respectively).
Household characteristics
More than half of households had six or more people living together; 83% were male-headed while 5% were single-parent households. Most households (81%) owned livestock and 69% were engaged in livestock herding. Regarding mothers/caregivers of children under five years, 57% were in their twenties and 5% were adolescents, while 13% were above 40 years old.
Water, sanitation and hygiene practices
Despite the fact that 74% of households obtained their water for drinking from potentially unsafe sources, 40% did not treat water before drinking. Those who treated water used various methods, including boiling, chemical treatment and use of traditional herbs. Only about 40% of households had access to toilet facilities. While 75% of mothers/caretakers reported using water and soap to wash their hands, 87% of caregivers did not practice hand-washing at least one critical moment or more, such as before cooking or after cleaning the child.
Household dietary diversity and food security
Generally, dietary diversity was comparatively low at the household level in this population. The median dietary diversity score was three food items. Based on the rankings used in the original SMART survey, 55% of households had low dietary diversity (three or less food groups consumed), 40% had medium dietary diversity (four or five food groups consumed), and only 5% had high dietary diversity (six or more food groups consumed). Despite their pastoral lifestyle, 75% of the households identified purchased food items as their main source of food, while 10% identified their own livestock products as their main source of food. Ninety per cent of households normally ate two or more meals per day, while 10% ate only once a day. In the three months prior to the survey, 47% of households had received general food distribution.
Children’s health
Kenya’s Expanded Programme on Immunisation includes vaccination of children against polio, tuberculosis, measles, diphtheria, and pertussis (MPHS, 2011). In the present survey, BCG, measles vaccine and oral polio vaccine (OPV) status was assessed. Immunisation coverage was generally high, with BCG and OPV reaching more than 80%, which met the National Immunisation Programme target of at least 80% coverage (MPHS, 2011). Seventy-eight per cent of children were given vitamin A supplementation, whereas 48% received deworming medicines in the past year. In the two weeks prior to the survey, 34% of children experienced one or more diseases; however 66% of mothers/caregivers said they did not seek any medical help whenever their child was sick. Among those who did seek help, public clinics were the most common point of contact. Community health workers were not utilised at all and traditional healers were also not a main source of help.
IYCF practices
More than 90% of children were breastfed within one hour of birth. In the first three days after delivery, 74% of children were given only breastmilk, while 26% of them were given non-breastmilk fluids. Apart from one child, none of the children met minimum dietary diversity (consumption of four or more food groups). Their diet was characterised by high consumption of dairy products and low consumption of vegetables, fruits, cereals, tubers, roots and legumes. However, since 78% of household main source of food was purchased food instead of the products of their own livestock, children’s dairy consumption may have been mainly sourced from purchased milk as well.
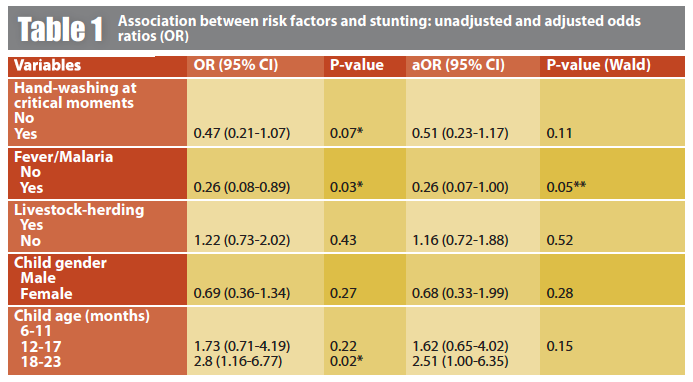
Stunting
Data for a number of factors that have been shown to be associated with stunting and wasting, such as maternal nutritional status pre-pregnancy, during pregnancy and after delivery; parental educational levels; and comprehensive socio-economic status were not available in the current dataset. Stunting prevalence in this population was 28%, with severe stunting of 5%. In the univariate logistic regression analysis, (lack of) caretaker hand-washing at four critical moments, having had fever or malaria in the past two weeks, and child age were associated with stunting. After adjusting for all the variables and a priori variables in multivariable logistic regression, none of the variables turned out to be associated with stunting. However, there was a borderline association between having experienced fever or malaria in the past two weeks and stunting (adjusted odds ratio=0.26, 95% confidence interval=0.07-1.00, p=0.05).
Wasting
Wasting prevalence was 8.8% based on WLZ, with only two severe wasting cases; MUAC produced a smaller prevalence of wasting (1.32%). Among those variables tested, lack of access to toilet facilities was significantly associated with wasting (p=0.09). Although not statistically significant, wasting was found to increase with age, with the 18-23 month age group having the highest wasting prevalence. No other risk factors were statistically significantly associated with wasting, and multivariate logistic regression was not conducted with wasting due to the low sample size for this indicator.
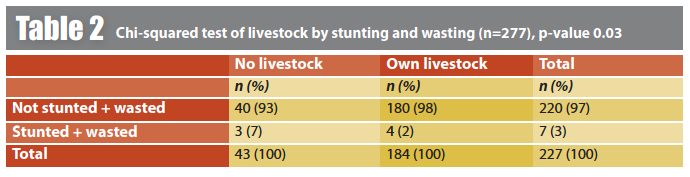
Combined stunting and wasting
While only a small sub-sample of the population was found to be both wasted and stunted, these children were significantly more likely to come from a household without any livestock ownership (p=0.03). The correlation between stunting and wasting was low at 5%.
Conclusions and recommendations
The prevalence of stunting in this pastoralist population in Samburu was 28.19%, which falls under the medium severity range according to the WHO classification of severity of malnutrition (WHO Global Database). Older children were more stunted than the younger ones. Median LAZ in all the age groups was below that of the reference population. In the univariate logistic regression analysis, three explanatory variables – hand-washing at four critical moments, having had fever or malaria in the past two weeks and child age – were associated with stunting. In the multivariate logistic regression analysis, none of these variables and a priori variables was significantly associated with stunting. However, there was a marginal association between fever or malaria and stunting.
The prevalence of wasting based on WLZ was 8.8%, which may also be considered in the range of medium severity according to the WHO classification (WHO Global Database). However, the body shape of pastoralist populations has been shown to be taller and thinner than sedentary populations, indicating that MUAC may be a better measure of wasting in such populations (Iannotti & Lesorogol, 2014). The prevalence of wasting based on MUAC was much lower.
Having access to toilet facilities and wasting were weakly associated. There was no evidence that the rest of the variables tested were associated with wasting. However, those children who were both stunted and wasted were more likely to be in households that did not own livestock.
There are several limitations to this secondary data analysis. Because the dataset is cross-sectional in nature, it only shows the nutritional status of children at one point in time and cannot account for seasonality and how this may affect prevalence of stunting and wasting. Additionally, because the SMART survey was not designed for the current analysis, the statistical power to detect an effect of the potential predictors on the outcomes of interest may be low. The lack of association, therefore, may be attributed to the study design and to errors in data entry, which resulted in a small sample size after data merging.
These results highlight the need for both programme-specific data and measurement-related improvements to be made at the field level and beyond. The following recommendations may be considered:
Programme-specific recommendations:
- Address poor WASH practices among the Samburu;
- Address access to healthcare for pastoralist communities;
- Improve dietary diversity among children under two years old;
- Increase integration across nutrition, WASH, reproductive health and health sectors to address multi-factor risk factors in settings of stunting and wasting.
Data and measurement-related recommendations:
- Consider powering SMART surveys to look at stunting as well as acute malnutrition in settings where both are known to be prevalent;
- Adjust reporting functions in Emergency Nutrition Assessment (ENA) to have the option to include stunting where relevant;
- Ensure data quality (unique IDs to ensure datasets can be linked between sector-specific surveys on the same population, or linked over time);
- Improve monitoring and evaluation integration between nutrition, WASH, reproductive health and health sectors;
- Rigorous research trials are needed to determine best measurement of wasting (MUAC vs. WLZ) in pastoralist contexts before meaningful work on stunting and wasting among these communities is possible;
- A rigorous impact evaluation of HiNi interventions on stunting and wasting among the Samburu is needed to determine pathways and explain lack of significant improvement in nutritional status despite ongoing, evidence-based interventions.
For more information, contact: Amelia Reese-Masterson or Mark Murage Gathii
References
Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427-451. doi:10.1016/S0140-6736(13)60937-X.
Iannotti L, & Lesorogol C,. Animal milk sustains micronutrient nutrition and child anthropometry among pastoralists in Samburu, Kenya. Am J Phys Anthropol. 2014;155(1):66-76. doi:10.1002/ajpa.22547.
KNBS, 2009. Kenya National Bureau of Statistics and Ministry of Planning National Develpment and Vision 2030. Kenya – 2009 Kenya Population and Housing Census ( 10 Per Cent Sample , Every 10th Household ), Population and Housing Census.; 2009.
Khara T, & Dolan C. Technical Briefing Paper: The Relationship between Wasting and Stunting, Policy, Programming and Research Implications.; 2014. doi:10.1016/S0306-3747(96)90467-4.
KDHS, 2010. Kenya Demographic and Health Survey 2008-09.; 2010.
KDHS, 2010. Macro KNB of S (Knbs) and I. Kenya Demographic and Health Survey 2008-09.; 2010.
MPHS, 2011. Kenya Comprehensive Multi-Year Plan for Immunization 2011-2015.; 2011.
MPHS, 2012. National Nutrition Action Plan 2012-2017.; 2012.
WHO Global Database. World Health Organization Global Database on Child Growth and Malnutrition.
UNICEF, WHO, World Bank, 2016. Update of UNICEF/WHO/World Bank database on child malnutrition | Field Exchange . Accessed March 2, 2016.