Ten steps to successful breastfeeding programme in DRC: a cluster-randomised controlled trial
Summary of research1
Location: DRC
What we know: Whilst most mothers initiate and continue breastfeeding in DRC, exclusive breastfeeding rates remain low.
What this article adds: A recent trial cluster-randomised controlled trial in an urban clinic setting investigated the effect on breastfeeding outcomes in infants under six months of an abbreviated Ten Steps to Successful Breastfeeding programme delivered by trained antenatal clinic staff. Antenatal clinic attendance in control and intervention groups was good. Implementation of steps 1-9 tripled the prevalence of exclusive breastfeeding at six months of age compared to controls (36% v 12%) and was associated with a significant reduction in diarrhoea prevalence compared to standard care. There was no impact on early initiation of breastfeeding. Additional support offered during well-child visits (steps 1-10) did not enhance the effect and may have lessened it. The findings suggest that in settings with high breastfeeding initiation, the provision of quality breastfeeding support to mothers in clinical settings might be as effective as the provision of community support through peer counselling.
Optimisation of breastfeeding practices could reduce high mortality rates in children under five years old. In the Democratic Republic of the Congo (DRC), despite near-universal breastfeeding initiation and nine out of ten children still breastfeeding at one year of age, exclusive breastfeeding in infants under six months remains elusive. This study assessed the effect on breastfeeding outcomes of implementing a short-cut version of the Ten Steps to Successful Breastfeeding programme, the key component of the Baby-Friendly Hospital Initiative (BFHI) (see Box 1). The short-cut version does not require the usual accreditation from BFHI; this study aimed to test whether this programme would be as effective as the accredited version and could more easily be scaled-up.
Box 1: Ten Steps to Successful Breastfeeding
The Ten Steps to support successful breastfeeding serve as the basis for the Baby-Friendly Hospital Initiative. The steps are:
- Having a written breastfeeding policy that is routinely communicated to all healthcare staff;
- Training all healthcare staff in skills necessary to implement the policy;
- Informing all pregnant women about the benefits and management of breastfeeding;
- Helping mothers to initiate breastfeeding within 30 minutes of birth;
- Showing mothers how to breastfeed and maintain lactation, even if they are separated from their infants;
- Giving newborn infants no food or drink other than breastmilk, unless medically indicated, and not accepting free or low-cost breastmilk substitutes, feeding bottles, or teats;
- Allowing mothers and infants to remain together 24 hours per day;
- Encouraging breastfeeding on demand;
- Giving no artificial teats or pacifiers to breastfeeding infants; and
- Fostering the establishment of breastfeeding support groups and referring mothers to them on discharge from a hospital or clinic.
Methods
The study involved a cluster-randomised controlled trial that randomly assigned healthcare clinics in the urban centre, Kinshasa, to one of three groups: standard care (control group); BFHI steps 1-9 (steps 1-9 group); or BFHI steps 1-9 plus additional support during well-child visits (steps 1-10 group). Computer-generated random numbers were used to assign matched pairs to study groups. Mothers at these clinics who had given birth to one healthy baby during enrolment and who expressed the intention to visit a well-baby session at the same clinic were eligible and received the treatment assigned to their clinic. Mother-infant pairs were excluded if the mothers intended to attend well-baby clinic visits at a different health facility, or to travel before the child was least six months old. Participants and independent interviewers were masked to group assignment (i.e. they were recruited after randomisation and training of the clinic staff and were not informed of the study scheme), but clinical staff were unmasked.
BFHI steps 1-9 and 1-10 were given by healthcare staff trained using the WHO/UNICEF BFHI course. The steps 1-10 group also received flyers in local languages containing culturally appropriate messages addressing behaviours that contribute to sub-optimal breastfeeding practices (such as giving the baby water in the first six months of life). The primary outcomes were breastfeeding initiation within one hour of birth and exclusive breastfeeding at 14 and 24 weeks, assessed at face-to-face interviews in the clinic using both 24-hour and seven-day recall. Two secondary outcomes were assessed: the prevalence of infants with reported diarrhoea and the prevalence with reported respiratory illness (fever with cough) between 10 and 14 weeks and between 18 and 24 weeks post-partum. The researchers undertook intention-to-treat analysis, complete-case analysis and per-protocol analysis. Prevalence ratios (PR) were adjusted for cluster effects and baseline characteristics.
Results
Between May 24 and Aug 25 2012, the authors randomly assigned two eligible clinics to control, two clinics to BFHI steps 1-9, and two clinics to BFHI steps 1-10. A total of 965 mother-infant pairs were eligible. Few imbalances in baseline characteristics were noted between the intervention and control groups. Mothers in the control group were slightly older and more likely to have attended at least four antenatal visits compared with mothers in the two intervention groups. Most missed no more than one visit in all groups. With the exception of one week post-partum, attendance was consistently higher in the control group than in the intervention groups throughout the study; this difference was significant only at the week six visit. Baseline characteristics did not differ between mother-infant pairs who attended follow-up visits and those who did not.
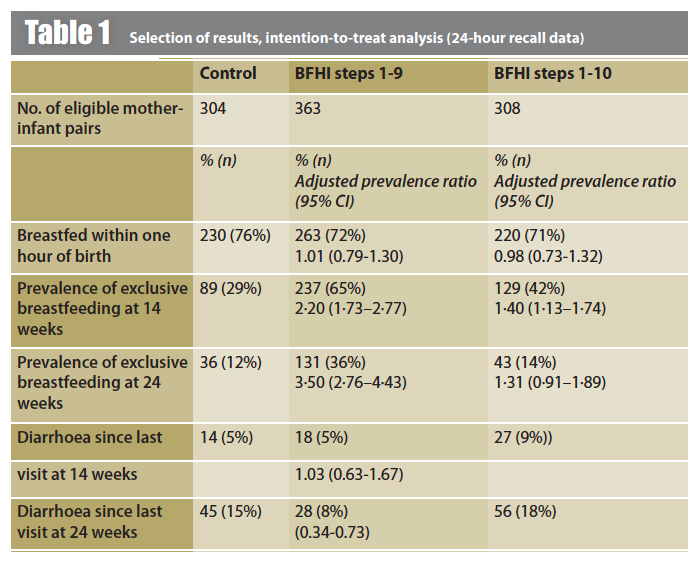
A selection of findings from the intention-to-treat analysis is summarised in Table 1. There was no significant group differences in breastfeeding within one hour of birth. However, the prevalence of exclusive breastfeeding at 14 weeks was significantly higher in both the steps 1-9 and in the steps 1-10 group. At 24 weeks, the prevalence of exclusive breastfeeding was significantly higher than the control in the steps 1-9 group only; in fact, it was three times higher than the control group and 2.6 times higher than the steps 1-10 group.
Prevalence of diarrhoea increased between week 14 and week 24 in all groups (see Table 1). The prevalence of diarrhoea at 14 weeks was similar between the control and steps 1-9 groups, but significantly higher than control in the steps 1-10 groups. The prevalence of diarrhoea at 24 weeks was significantly lower in the steps 1-9 group (8%), having similarly risen in the control (15%) and steps 1-10 groups (18%). No significant differences between groups were noted in the prevalence of reported respiratory infections at 14 or 24 weeks.
Discussion
In the setting of healthcare clinics in DRC with a high proportion of mothers initiating breastfeeding, implementation of basic training in BFHI steps 1-9 had no additional effect on initiation of breastfeeding, but significantly increased exclusive breastfeeding at six months of age (three times higher than for the control group). This finding is consistent with other recent research (PROMISE trial in South Africa; Tylleskär et al, 2011) and suggests that, in settings with high breastfeeding initiation, the provision of quality breastfeeding support to mothers in clinical settings might be as effective as the provision of community support through peer counselling. The common practice of supplementing breastfed infants with water in an environment where only 23% of the urban population has access to improved sanitation facilities and less than 50% to improved sources of drinking water could account for some of the increased risk of diarrhoea where infants are not exclusively breastfed.
Additional support based on the same training materials and locally available breastfeeding support materials, offered during well-child visits (i.e. step 10), did not enhance this effect as expected, and might have actually lessened it. The authors postulate that that the materials used might not have provided the accurate or necessary messages for this setting, or that engagement of family members might have led to misunderstandings or incorrect advice that were not sufficiently countered by group counselling from nurses during well-child visits.
The implementation of BFHI steps 1-9 by training health personnel with the WHO/UNICEF course – a fairly low-intensity, low-tech intervention that is very suitable for rapid scale-up in maternity settings – significantly raised the proportion of infants exclusively breastfeeding at six months old and decreased diarrhoea prevalence by half at this age. The authors suggest that large-scale implementation of steps 1-9 in similar settings could help to reduce mortality quickly in children under five years old.
References
1 Yotebieng M, Labbok M, Soeters HM, Chalachala JM, Lapika B., Vitta BS, Behets F. (2015). Ten steps to successful breastfeeding programme to promote early initiation and exclusive breastfeeding in DR Congo: a cluster-randomised controlled trial. Lancet Global Health 2015; 3: e546-55.
Tylleskär T, Jackson D, Meda N, et al 2011. Exclusive breastfeeding promotion by peer counsellors in sub-Saharan Africa (PROMISE-EBF): a cluster-randomised trial. Lancet 2011; 378: 420–27


