Alert and rapid response to nutritional crisis in DRC
By Alain Georges Tchamba
Alain Georges Tchamba is the Nutrition coordinator at Cooperazione Internazionale (COOPI) in the Democratic Republic of the Congo, in post since 2010. He is responsible for the nutrition strategy and the design, implementation, monitoring and evaluation of nutrition activities.
The author acknowledges the support of ECHO, UNICEF and PRONANUT to the programme. Special thanks to Lucia Pantella, Nutrition Adviser for COOPI, for her contribution to the development of this article.
Or read the podcast transcript in Français or English.
Location: Democratic Republic of Congo (DRC)
What we know: While national prevalence of acute malnutrition has fallen in DRC, the severe acute malnutrition (SAM) caseload remains significant in many provinces, linked to chronic crisis and longstanding structural causes.
What this article adds: A three-year (2013-15) Rapid Response to Nutritional Crisis Project (RRCN) was implemented by COOPI, in collaboration with the government and UNICEF, to rapidly respond to surges in the SAM caseload. It involved six-month interventions (technical support, capacity-building, therapeutic food and medicine supplies) in response to confirmed alerts, integrated within existing health centres at district level. Geographical coverage in 21 districts increased considerably to 77%. Sphere targets were met and the project exceeded performance targets for numbers treated; providing RUTF supplies and free treatment were important success factors. Continuation of services post-intervention proved limited, despite government-backed exit plans from the outset; only four out of 21 health zones continued services. Lack of RUTF supplies and medicines; limited national agency capacity to sustain staff supervision; lack of development partners for transition of services; and reverting to paid treatment services proved key limiting factors to sustainable SAM treatment.
Background

For the past two decades, the nutrition situation in the Democratic Republic of Congo (DRC) has been critical. While national prevalence of global acute malnutrition (GAM) has fallen significantly from 16% in 2001 to 9% in 2014, there are areas of high wasting prevalence at provincial level, such as Maniema Province (22%), Bas-Congo (11%) and ranging from 3.5% to 9.8% in other provinces. About two million children aged 6 to 59 months are wasted (PRONAUT, 2015). An estimated 15% to 20% of severe cases are covered by the Integrated Management of Acute Malnutrition (IMAM) service available in 420 of 516 health zones (Ministère de la Santé Publique, 2016); IMAM is available in three to four out of 20 health centres in a given zone and service continuity may vary. There has been no evaluation of national SAM treatment coverage.
In order to better monitor the nutritional situation and promptly identify nutritional crises in the DRC, a system of nutritional surveillance, the Food Security and Early Warning system (SNSAP)1 was piloted in 2009 and established by the National Nutrition Programme (PRONANUT) at the end of 2010. In this context, from 2009 to 2010, COOPI managed an emergency intervention, the Nutritional Pool in DRC (PUNC), funded by UNICEF. This involved a mechanism to detect and quickly respond to a nutritional crisis, with a three-month follow-up/intervention period. This proved very difficult in practice, given the limited intervention period to treat malnourished children without a strong exit strategy. To address these obstacles a new project, Scaling up Nutrition, was developed in 2011, funded by UNICEF (UNICEF, 2013). This involved the use of SMART (Standardised Monitoring and Assessment of Relief and Transitions) surveys conducted by PRONANUT and an 18-month planned intervention period in all areas identified with a GAM prevalence >15%. However, this approach lacked the flexibility that characterised PUNC to react and scale up response to new nutritional crises.
Given this, the Rapid Response to Nutritional Crisis Project (RRCN) was established in 2013 by COOPI, funded by the Humanitarian Aid and Civil Protection of the European Commission (ECHO) through UNICEF, and has become part of the national health policy and strategy. Given that malnutrition is recurrent in several health areas, the RRCN integrates water, sanitation and hygiene (WASH) components (as reflected in the ‘Wash in Nut’ strategy that is national policy), and has a better exit strategy, which involves strengthening the capacity of the health authorities to treat and prevent SAM2. The target population is acutely malnourished children aged six months to five years and adults (particularly pregnant and lactating women (PLW)).
This article describes how the RRCN interventions were put in place between 2013 and 2015 and their relevance, coverage, effectiveness and lessons learned.
Method
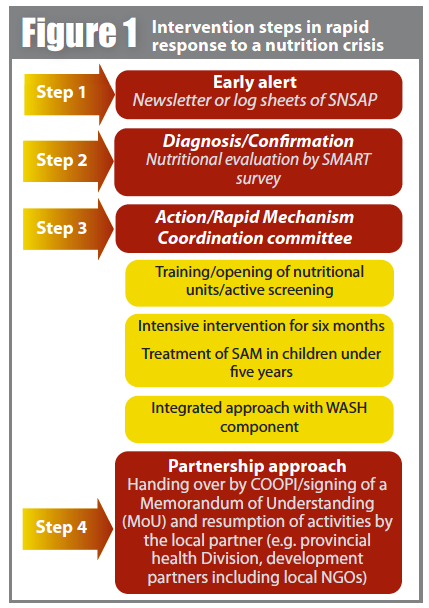
The RRCN aims to quickly and effectively respond to a nutritional crisis in an area with prevalence of GAM>15% or where the prevalence of SAM is >5%. The interventions steps, outlined in Figure 1, are as follows:
Early alert
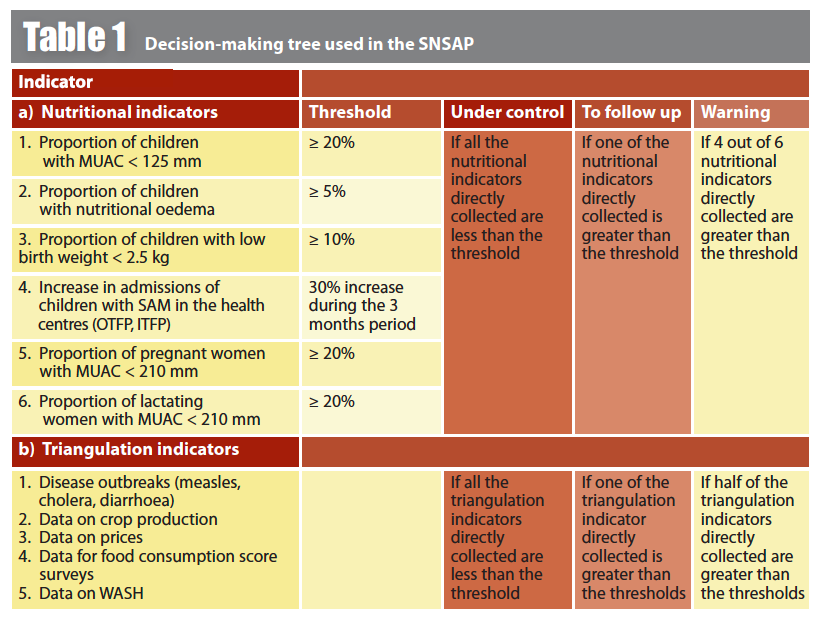
The PRONANUT uses monthly factsheets or quarterly bulletins to alert to nutritional crisis generated from SNSAP data. The SNSAP tracks nutritional indicators using quarterly routine data gathered from 776 sentinel sites at healthcare centres throughout all provinces (PRONAUT, 2016). The objective is not to get data statistically representative of one health area but to observe and record any change, identify trends and compare the results throughout the year. Nutrition data gathered are: mid-upper-arm circumference (MUAC) in children aged 6-59 months and PLW healthcare; child oedema; birth weight; and number of cases of malnutrition admitted to healthcare structures. These data are triangulated with indicators on food security (Food Consumption Score, Coping Strategy Index (CSI), food basket price), health (measles, cholera and diarrhoea outbreaks) and WASH. An alert is declared if the indicators reach the ‘red’ threshold for three consecutive months, according to a decision tree (see Table 1). SNSAP bulletins analyse patterns, although seasonal trends have not been possible to identify.
Diagnosis
Alerts are confirmed by a SMART survey, carried out within one month of an alert.
Action
A Rapid Mechanism Coordination Committee (RMCC) is set up under the supervision of PRONANUT to act following alert confirmation. The operational response will begin four weeks after the alert is confirmed for a period of six months. This involves setting up or strengthening IMAM and promoting Infant and Young Child Feeding (IYCF).
Multi-sector approach
The WASH component involves the distribution of WASH kits (antiseptic, bucket or jerrycan and soap) to the caregivers of malnourished children, hygiene messaging and improving WASH facilities in health centres (building toilets, constructing water sources and providing water storage kits).
Partnership approach
A partnership mechanism is developed between COOPI, PRONANUT and the Central Health Office Area (BCZ) to facilitate implementation (technical support, capacity-building) and handover of activities at the end of the intervention (within one month).
Relevance
Under the RRCN project, the management of SAM is integrated into health centre activities for the period of the intervention. The community component relies on community health workers (CHWs) and volunteers for screening, referral, outreach and home monitoring of cases or dropouts. The project has enabled mothers of malnourished children to monitor their children’s nutritional status using simple, coloured MUAC plastic tapes.
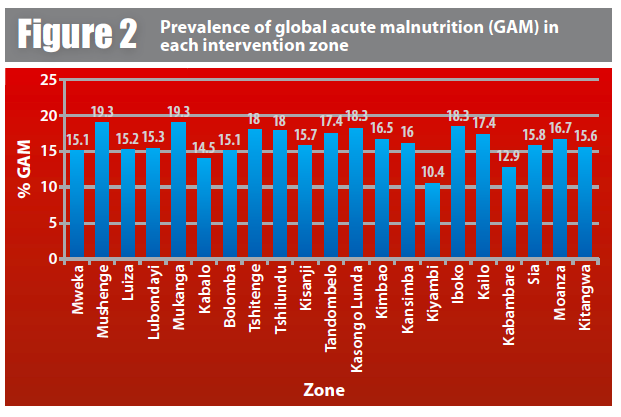
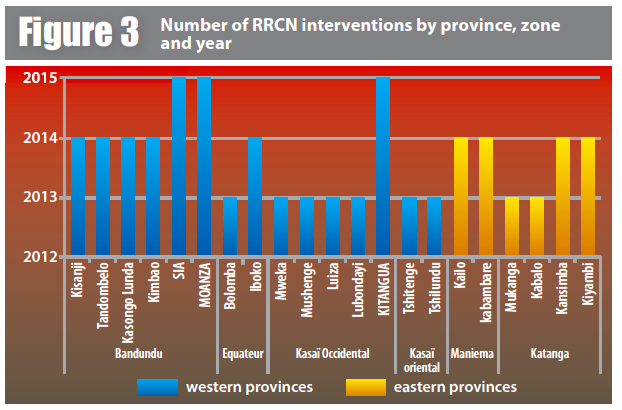
Targeting based on GAM>15% and SAM >5%3 improved geographical coverage where it was most needed and extended services to remote health zones of the country (see Figure 2). Pre-RRCN, IMAM activities were largely concentrated in conflict-affected eastern provinces where insecurity and displacement were the main causes of acute malnutrition. Since 2013, 15 of the 21 RRCN health zones (71%) are located in western provinces (Figure 3, blue); malnutrition here is a result of economic factors, combined with poor harvests, inadequate food, nutrition and hygiene practices, and chronic food insecurity. According to routine health zone data, 40% of under-fives child deaths in the health zone pre-RRCN were due to severe malnutrition; this fell to 2% during RRCN implementation, attributable to increased access to free treatment at health centres.
Coverage
During its three-year period, the RRCN project supported 21 health zones and enrolled 254 (out of 408) health centres to achieve 62% clinic coverage. None of these health posts had a structured IMAM programme or mobile units in place pre-RRCN. Implementation involved setup of 254 outpatient/community therapeutic feeding programmes (OTFPs) and 21 inpatient therapeutic feeding programmes (ITFPs). Outreach activities were put in place through 70 health posts and 45 mobile clinics to reach remote/difficult-to-access villages. Mobile units were connected to the closest fixed stations for monthly statistics and to coordinate activities. The minimum mobile team package comprised MUAC screening, referral of severely malnourished children with medical complications to hospital, and treatment of severely malnourished children without medical complications. Uncomplicated case management is protocol-led, providing ready-to-use therapeutic food (RUTF) and antibiotics (amoxicillin), with fortnightly follow-up by the mobile clinic, and community worker follow-up at village level between clinic visits. As a result, each health zone improved to an average 77% geographical coverage.
Efficiency
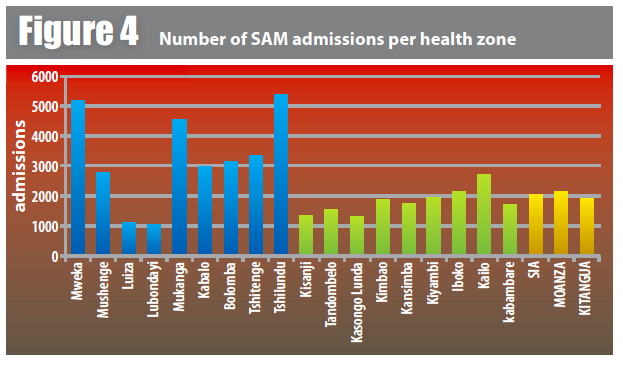
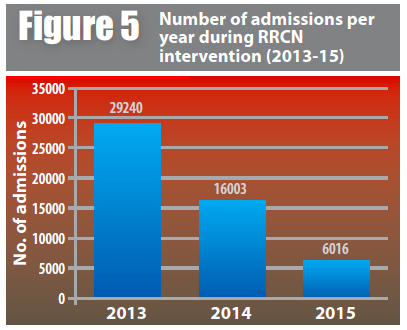
Over the three-year project period, the cumulative number of children registered with SAM was 51,259 against an estimated target of 37,000 (see Figure 4), with a performance rate4 of 138% (29,240 in 2013, 16,003 in 2014 and 6,016 in 2015). The performance rate is higher than expected because children from other geographical areas beyond the project boundaries were also treated. Children from six months to five years represented 90% of the beneficiaries, while PLW comprised 10%. The recovery rate (97.7%), death rate (0.2%) and defaulter rate (2.1%) were well within Sphere targets (<75%, <10% and <15% respectively). The average length of stay in OTFP was 32 days.
A total of 1,315 healthcare providers (target 800) were trained on the IMAM approach, in addition to 1,676 community volunteers. The project also established 87 community support groups to promote IYCF and best WASH practice. WASH kits were distributed to all 20,376 malnourished children. The mean number of SAM admissions per health zone was 2,440 patients; three health zones had admissions of up to 4,000 (see Figure 4).
The decrease in admissions from one year to the next, reflected in Figure 5, is partly due to reduced funding that mainly concerned areas not affected by rapid-onset emergency or conflict; nutritional insecurity in the DRC is due more to structural causes and chronic crisis, so is not a priority for emergency funding. While the reduction in funding reduced the number of interventions from nine (2013, 2014) to three per year (2015), there was an increase in intervention coverage in each health zone from 60% in 2013-2014 to 80% in 2015. This was achieved by each RRCN covering more health centres within the health zone. There are several confirmed alerts in the DRC in 2016 without a response due to funding limitations. Within the nutrition cluster, COOPI, together with RRCN partners, advocates for interventions in ‘alert’ areas to be implemented by other agencies.
Note: Figures are for COOPI operations only; acute malnutrition treatment services are also provided by other agencies.
Sustainability
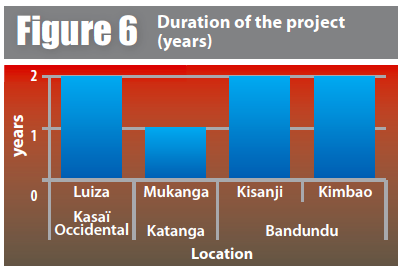
Following the six-month RRCN intervention, it is necessary for another partner and funder to step in; most often, health zones will have other serious structural problems such as food insecurity or WASH problems that require external donor support. The Nutrition Cluster has played an advocacy role to try to secure longer-term intervention follow-up. However, only four health zones out of 21 have continued, with an average intervention of 18 months post RRCN (see Figure 6).
In general, healthcare workers gained technical skills to enable continuity of services. Promoting IYCF and WASH is a considered investment in longer-term practices. The health zone teams’ participation and their support to the project contributed to its reach.
During the RRCN intervention, RUTF is sourced from UNICEF, who supplies it to COOPI; COOPI and BCZ manage the RUTF and distribute it to the health centres. A three-month stock of RUTF is left in the health zone at the end of the intervention; however lack of supplies has proved a barrier to sustaining services (see below).
Lessons learned
Key lessons learned over the three-year experience include the following:
Prioritising diagnosis, context analysis and flexibility
The RRCN project provided the means and tools to diagnose, analyse the intervention context and identify the most vulnerable communities. Although alert confirmation by SMART survey requires a significant investment in time and resources, we consider it an essential step. Effective functioning of the SNSAP mechanism is necessary to track the nutritional situation, with a SMART confirmation sensitivity of 80% (PRONAUT, 2015).
PRONANUT receives monthly data from the sentinel site but issues a quarterly bulletin; a time lag between data gathered and bulletin delays decision-making. As a result, in some cases an intervention took place months after the initial ‘alert’ warning. The time between data alert and bulletin alert must be reduced to enable a quicker response.
Increasing the timeliness of rapid response interventions
A SMART survey is organised and delivered within one month of an alert. The time between alert confirmation by SMART and start of activities should be reduced to less than four weeks (in practice this could happen quickly or take up to two months). The full cooperation of local-level MoH officials is a precondition to speed-up this process. More rapid response would be helped by an immediate green light to intervene from all authorities in the concerned areas; training of national and regional staff by PRONANUT; and provincial pre-positioning of RUTF stock (noting that capacities for stock management within PRONANUT are limited). Implementing partners should have a contingency stock of RUTF available and trained teams to minimise the planning and preparation phases, before field deployment. Once a project ends, COOPI staff are ‘recycled’; they may be deployed to another nutrition project to provide support until required for a new RRCN intervention. Staff are reactivated one month before the start of a new project, for preparation.
Working on improved coverage, targeting and project monitoring
The availability of fixed services, mobile units and outposts has helped to cover most malnourished children; this strategy should be encouraged. There is still room for improvement on geographic coverage, ultimately aiming to target 100% of health areas in a health zone. The estimated caseload of RRCN intervention areas was 81,610 severely malnourished children; 51,259 cases were treated (estimated 63% coverage). No SQUEAC coverage surveys were conducted within the RRCN due to limited time.
Building the capacity of caregivers to screen using MUAC and distribution of MUAC tapes to the caregivers of admitted SAM children to facilitate nutritional surveillance in their home communities should be encouraged; this allows early detection and referral of malnourished children and empowers the caregivers.
State involvement, coordination and transition
Several state government institutions (PRONANUT, Provincial Health Division (DSP)) are directly or indirectly involved in managing the various crises under the RRCN. Cooperation with government actors is important to sustain efforts by building capacity. Despite transition agreements from the outset, the continuation of activities proved a major challenge. PRONANUT does not have the means to supervise nutrition activities at health-zone level. Once the intervention stops, lack of RUTF and medicines means that BCZ staff can only screen for cases and share data, without commitment to treat. Similarly, there is a lack of resources to support BCZ staff transportation to supervise health centres and activities. Takeover of the intervention by development partners or by the DSP post-six month intervention has proved weak. The Nutrition Cluster has advocated for local NGOs as partners, but their lack of access to funds has prevented this.
Partnership with the MoH in some provinces has faced challenges during implementation. For example, administrative issues in signing MoUs delayed the start of activities for a month in some areas. Coordination between various MoH departments is not well developed; improvement could help establish closer relations with other activities or development programmes. The protracted nature of the crisis in the DRC requires longer-term interventions, necessitating greater synergies between humanitarian and development service providers.
Strengthening the health system
Good management and quality services require competent, committed, motivated and results-oriented people with effective leadership. It is therefore necessary to make relatively large investments in the capacity-building component for staff at all levels as part of the programme. Change in behaviour and practices of health centre staff requires more than simple transfer of skills; it requires improvement in the working conditions and salaries of health personnel. It is also necessary to expand the network to include partners from non-government sectors (local NGOs) to access further resources and expertise. Promoting good IYCF and WASH practices through community support groups can improve beneficiary knowledge and attitude change; this approach should be expanded in all areas of intervention.
Improvement of accessibility to health services
Free health and nutrition services for all children and mothers affected by acute malnutrition was a strength of the project; usually patients must pay for malnutrition consultation and care. RUTF is commonly sold (although it should be provided for free) in order to cover the costs of the health centres. Ensuring free transportation of referred children (with accompanying persons) and feeding during their staying in the ITFP helped mothers to accept the referral of their child. Maintaining free services for malnourished children after the end of the project is a key challenge to sustainability.
Consideration of project logistics
The logistical assessments conducted within RRCN interventions provide a critical understanding of intervention areas in terms of accessibility, transportation, communication and storage needs that inform how to reduce the time gap between the alert and start of activities. Accessibility problems during RRCN implementation created delays in the supply of inputs, causing stock-outs of RUTF. Logistics assessments should be conducted before field deployment of nutrition staff, with a final evaluation to identify bottlenecks and lessons learnt.
The challenge to ensure follow-up interventions
Funding agencies, government institutions and civil society actors involved in this project must build links between the rapid response mechanism and longer-term interventions. Development programmes that commonly focus on reducing malnutrition by addressing its underlying causes can strengthen and enhance livelihoods in a sustainable manner. In this context, the RMCC plays an important advocacy role with the actors involved in health-system strengthening programmes in order to include and integrate IMAM in the minimum package of activities.
One of the key challenges to continuity of nutritional activities is the supply of therapeutic nutritional inputs (RUTF). Health zones usually do not have RUTF supplies when there is no nutrition intervention.
The long distances between villages and the lack of sufficient high-calibre staff hinder access to health services by the communities. High health centre staff turnover undermines continuity of malnutrition treatment, while extreme poverty also forces staff to undertake essential livelihood activities rather than be permanently deployed in health facilities.
The absence of roads and poor state road infrastructure generate high logistics costs, complicate the movements of field teams and make their missions strenuous; most RRCN interventions are located in remote and isolated areas.
Conclusion
The RRCN has proved a flexible and responsive short-term intervention to treat acute malnutrition and save lives; admissions and surveillance data show the caseload of malnourished children has decreased significantly in the targeted areas. Providing RUTF supplies and access to free treatment were important success factors. Linking the rapid responses to longer-term interventions has had little success, impeded by lack of RUTF supplies and medicines; limited national-agency capacity to sustain supervision; lack of development partners for transition, and discontinuation of free treatment. Establishing the role of development and government agencies in providing longer-term interventions to build and sustain health service capacity and address the underlying causes of malnutrition is critical to reduce nutrition insecurity in the long run.
For more information, contact: Lucia Pantella nutrition@coopi.org, Alain Tchamba nutrition.rdc@coopi.org
References
Ministère de la Santé Publique, 2016. Protocole National de Prise en Charge Intégrée de la Malnutrition Aiguë, version de Mai 2016.
PRONAUT, 2015. Rapport Annuel du PRONANUT, 2015.
PRONAUT, 2016. Bulletin de la Surveillance Nutritionnelle, Sécurité Alimentaire et Alerte Précoce (SNSAP), September 2016.
UNICEF, 2013. Rapport final du projêt Scaling Up Nutrition, 2013
1Surveillance Nutritionnelle, Sécurité Alimentaire et Alerte Précoce. For more information, visit: www.pronanut-rdc.org/telechargements/bulletin-snsap.html
2The RRCN does not extend to MAM treatment. Where there are RRCN interventions for SAM, there may be support from WFP for MAM treatment.
3Exceptions were made in two health zones where intervention decision was based on the SAM rates: 5.1% for Kyambi (GAM 10.4%) and Kambabaré (GAM 12.9%).
4The performance rate is the proportion of treated children compared to the expected caseload of children with SAM (according to the SMART SAM rate prevalence, the population in the area and an incidence factor of 2.6% for six months) and coverage.


