Improving community management of uncomplicated acute malnutrition in infants under six months (C-MAMI): Developing a checklist version of the C-MAMI tool
Summary of MSc project report1
 By Sonja Read
By Sonja Read
Sonja Read is a public health nutritionist from the London School of Hygiene and Tropical Medicine. She has previously worked in various support functions across different NGOs. With a background in strategic management, her passion is to contribute to effective programming and nutrition interventions.
This research was carried out as part of a Master’s dissertation. The author would like to acknowledge Dr Marko Kerac, who supervised the research, for his support throughout the project, and Marie McGrath and Nichola Connell for their input, especially at the conception stage. Thank you to Malawi Epidemiology & Intervention Research Unit for hosting the research, especially to Professor Moffat Nyirenda and Dr Amelia Crampin.
Location: Malawi
What we know: WHO recommends treating uncomplicated acute malnutrition in infants <6 months in an outpatient setting; few countries have implemented these guidelines. The C-MAMI tool was developed to help identify, assess and manage malnourished and at-risk infants <6m of age at community level. It has not yet been field-tested.
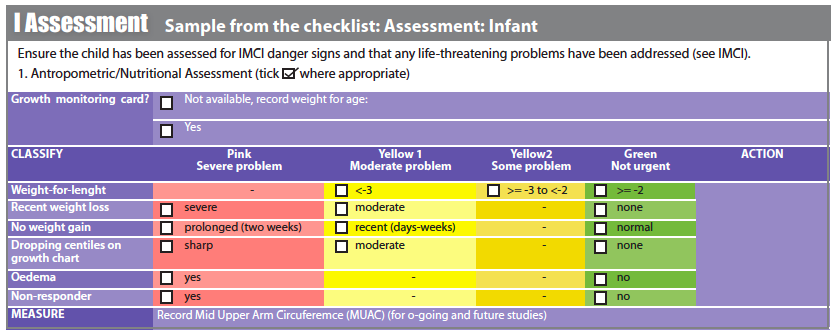
What this article adds: A study developed checklist versions of the assessment part of the C-MAMI tool and tested these and the full tool with Malawian health workers. The tool was regarded by health workers as necessary to fill an existing gap and could improve case identification and management. A shorter checklist version was largely preferred for the assessment of malnourished and at-risk infants <6m in programmatic contexts. Many reported difficulties using any form of the tool for the first time, e.g. anthropometric/nutritional assessment resulted in different treatment outcomes for the same child; several checklist items were interpreted differently; and boundaries between categories ‘severe’ and ‘moderate’ were often unclear. Recommendations include developing a management guide with support actions to accompany a C-MAMI checklist; clear definitions; and well-designed training for community health workers.
 The management of malnutrition in infants under six months (infants U6m) poses several challenges compared to older children. The exclusive breastfeeding norm and physiological/development immaturity in the age group excludes them from the use of ready-to-use therapeutic food (RUTF) as a principal treatment. Breastfeeding practices and related problems, as well as the mother’s physical and mental status, need to be assessed and potentially addressed (McGrath, 2016). Perhaps due to these challenges, only one out of 46 country SAM guidelines recently reviewed recommend outpatient management of uncomplicated infants U6m, despite the WHO recommendation to do so (McGrath, 2016).
The management of malnutrition in infants under six months (infants U6m) poses several challenges compared to older children. The exclusive breastfeeding norm and physiological/development immaturity in the age group excludes them from the use of ready-to-use therapeutic food (RUTF) as a principal treatment. Breastfeeding practices and related problems, as well as the mother’s physical and mental status, need to be assessed and potentially addressed (McGrath, 2016). Perhaps due to these challenges, only one out of 46 country SAM guidelines recently reviewed recommend outpatient management of uncomplicated infants U6m, despite the WHO recommendation to do so (McGrath, 2016).
The C-MAMI (community management of acute malnutrition in infants U6m) tool2as developed by ENN and the London School of Hygiene of Tropical Medicine (LSHTM) in a multi-agency/expert collaboration is a first step in adapting the WHO recommendation into a more operational form for front-line practitioners. Developing a checklist version of the C-MAMI tool is particularly important to make it as simple, fast and effective as possible for health workers in communities (ENN et al, 2016).
Methods
Two checklist adaptations of the C-MAMI tool were developed and piloted with the original tool in semi-structured interviews involving role play and observational data-gathering with health workers from hospitals, clinics and the community in Malawi. Data were analysed with framework and thematic analyses. Key informant interviews, including with the original tool developers, and semi-structured interviews were used to refine a C-MAMI checklist.
Results
Six themes emerged from the semi-structured interviews (n=24), key informant interviews (n=5), completed checklists and observations.
General impressions about the tool
All health workers interviewed welcomed the tool but nearly half (n=11, 46%) found first-time use difficult or considered frequent use was necessary to use it effectively. There were contradictory statements regarding the workload that the tool would add. Compared to current practice, the tool was described as systematic and comprehensive. Most respondents preferred the checklists due to their simplicity.
Training needs
All respondents agreed that training is necessary in order to use the tool effectively. Assessment outcomes varied between respondents and items in the checklist were interpreted in different ways, further suggesting training is needed.
Difference made by the tool
More malnourished infants U6m could be identified and managed as no standardised way of doing this currently exists. The comprehensiveness of the tool would help identify problems, especially those that are not explicitly expressed by the mother. Health workers would cover some but not all items on the checklist. Community-based care was thought to have benefits to the mother, saving time and money. Many respondents said they were keen to be able to handle such infants instead of having to refer them for inpatient treatment.
Potential difficulties
There was great variation in how the anthropometric/nutritional assessment was understood and completed, resulting in various treatment implications (inpatient vs outpatient) for the same scenario. Classification by weight-for-length z-scores (WFL) was particularly difficult for participants; most respondents skipped it. When probed for reasons why, interviewees mentioned unfamiliarity with the measurement and z-scores and confusion with weight-for-height. Many found the anthropometric/nutritional assessment difficult.
There are some discrepancies between current practice and the tool; e.g. wet nursing was discouraged by health workers, who also advised that lack of breastmilk was linked to mother’s diet.
Differences among health workers in understanding the tool emerged as an important factor in how the tool will be received. Respondents pointed out that some health workers have difficulties in understanding new things, while others are much quicker to grasp new practices.
Using and interpreting the tool
There was a great deal of variation in how questions were posed and interpreted. Differences between diagnostic categories were not always clear to respondents, especially the difference between ‘severe’ and moderate’. They were sometimes unsure whether they should classify based on observation or history; e.g. diagnosis of weight gain was different based on maternal report versus comparing birthweight to current weight.
Non-breastfeeding assessment and support
Non-breastfeeding is one of the most sensitive parts of the assessment and it divided opinions among key informants. All key informants agreed that the non-breastfeeding assessment should be on the checklist, but opinions differed as to where it should be positioned in the tool (i.e. middle or end). In the non-breastfeeding role play respondents often advised the mother to breastfeed, but no one identified relactation as a support action.
Discussion
The results of this study confirm the need for a community-based model of care for this age group (Angood et al, 2015) and substantiate previous findings which show that infants U6m with feeding problems are currently being neglected by health systems (McGrath, 2016). In Malawi, the tool would fill an existing gap and present a viable and welcome option in ensuring infants and feeding problems are not missed. Training is essential.
This study supports previous findings that WLZ is a troublesome measurement in infants U6m (Mwangome et al, 2016) and alternatives should urgently be explored for easier identification of at-risk infants. Clarifying the meaning of each checklist item is likely to avoid much of the variation in assessment outcomes. At implementation, practical considerations should inform adaptation to contexts. For example, community workers in Malawi currently do not conduct clinical assessments. Even with the C-MAMI tool, non-breastfeeding cases may be difficult to manage and viable options will depend greatly on the context.
The study recommends the following actions to support implementation:
-
Use of a C-MAMI checklist to identify and assess malnourished and at-risk infants U6m, accompanied by a support-action booklet containing the management actions;
-
Well-designed training needs to be carried out when implementing the C-MAMI tool and due attention should be given to the anthropometric/nutritional assessment;
-
Use of WLZ in infants U6m should be reviewed;
-
Each item in the tool needs to be clarified and clearly defined, including how information is to be collected (history vs. observation), e.g. in a training guide.
Further research should put greater focus on the management part of the C-MAMI tool and test the implementation of the tool in programmes.
For more information or to get a copy of the checklist, contact: sonja.read1@alumni.lshtm.ac.uk
Footnotes
1The full MSc report is available at: www.lshtm.ac.uk/library/resources/msc_projects/ under Nutrition for Global Health (formerly Public Health Nutrition) 2016.
2C-MAMI tool version 1.0, November, 2015. A full version is free to download at www.ennonline.net/c-mami.
References
McGrath, 2016. McGrath M. Updated review of national guidelines on MAMI: Key findings. In: Management of Acute Malnutrition in Infants under 6 months (MAMI) Interest Group MarieMeeting ENN, LSHTM & Save the Children. London, UK; 2016.
ENN et al, 2016. ENN, LSHTM and Save the Children. Management of Acute Malnutrition in Infants under 6 months (MAMI) Interest Group Meeting. Meeting Report January 2016. files.ennonline.net/attachments/2482/MAMI-Meeting-Report-Jan-2016.pdf
Angood et al, 2015. Angood C, McGrath M, Mehta S, Mwangome M, Lung’aho M, Roberfroid D, et al. Research Priorities to Improve the Management of Acute Malnutrition in Infants Aged Less Than Six Months (MAMI). PLoS Med. 2015;12(4).
Mwangome MK, Fegan G, Mbunya R, Prentice AM, Berkley JA. Reliability and accuracy of anthropometry performed by community health workers among infants under 6months in rural Kenya. Trop Med Int Heal. 2012;17(5):622–9


