Risk factors for severe acute malnutrition in infants <6 months old in semi-urban Bangladesh: A prospective cohort study to inform future assessment/treatment tools
Summary of conference abstract1
Presented at the ACF research conference, November 9th, 2016.
By M Munirul Islam, Yasir Arafat, Nicki Connell, Golam Mothabbir, Marie McGrath, James Berkley, Tahmeed Ahmed, and Marko Kerac
M Munirul Islam and Tahmeed Ahmed both work at the Nutrition and Clinical Services Division, International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b). Yasir Arafat and Golam Mothabbir work in the Health Nutrition and HIV/AIDS Sector, Save the Children, Bangladesh. Nicki Connell works in the Department of Global Health, Save the Children USA. Marie McGrath works with the Emergency Nutrition Network, UK. James Berkley is based with the KEMRI/Wellcome Trust Research Programme, Kenya. Marko Kerac is based at the Department of Population Health, London School of Hygiene & Tropical Medicine,
Video footage of the conference presentation is available here.
Location: Bangladesh
What we know: The burden of acute malnutrition in infants < 6 months varies by country. Community-based case management for uncomplicated cases is lacking.
What this article adds: A recent study investigated the prevalence of acute malnutrition in infants<6m in semi-urban Bangladesh (two seasons) and undertook a prospective cohort study to describe current outcomes of identified cases at six months (180 days) of age. Prevalence of acute malnutrition was low post-harvest but increased pre-harvest; from 0.4% to 5.9% for severe acute malnutrition (SAM) and 2.8% to 10.1% for global acute malnutrition. At age six months, 24% of identified SAM cases (by eight weeks of age) and referred for available treatment (inpatient), remained severely malnourished. A range of infant and maternal risk factors for infant SAM were identified, involving breastfeeding status, the nutrition and mental health of the mother, infectious disease and water/sanitation/hygiene. A package of care is warranted in this age group.
Current WHO guidelines on severe acute malnutrition (SAM) management recommend outpatient management of uncomplicated acute malnutrition in infants under six months of age (infants <6m), in line with the now-established treatment approach for older children (WHO, 2013). However, there is a lack of practical guidance on how to identify those infants <6m at risk and how to manage them. Current WHO case definition for SAM in infants <6m is weight-for-length of less than -3 Z-score (WLZ); visible severe wasting; and/or bilateral pitting oedema.
To inform the development of assessment tools and treatment approaches for SAM in infants <6m, a study was conducted in semi-urban Bangladesh in 2015/2016 with the following objectives:
- To estimate the prevalence of infants <6m with acute malnutrition in the community;
- To develop an assessment tool/case definition checklist for infants <6m with acute malnutrition; and
- To describe current outcomes following infant <6m with acute malnutrition.
The study involved two prevalence surveys (in distinct seasons) and a prospective cohort study of three infant groups (77 in each group), followed from 4-8 weeks to 180 days post-partum. The groups comprised:
Standard SAM: WLZ <-3 and/or bipedal oedema;
Normal: WLZ ≥-2 to <+2 z-scores, no oedema;
Expanded SAM: MUAC <115mm but WLZ ≥-2, no oedema.
MUAC case definition does not exist for infants <6m; data were collected for research purposes only. Mother/caregiver interviews at enrolment assessed potential risk factors. Infants with ‘Standard SAM’ were referred to existing services for treatment (inpatient care) according to existing protocols. The primary outcome was nutritional status at age completion of 180 days.
Preliminary results
Prevalence survey
The prevalence of GAM and SAM were low in the post-harvest period but increased pre-harvest; from 0.4% to 5.9% for SAM and 2.8% to 10.1% for GAM. Severe underweight (weight for age < -3 Z- score (WAZ)) slightly increased (severe: 5% to 6.1% and severe/moderate combined, from 14.4% and 16.3%).
Cohort study
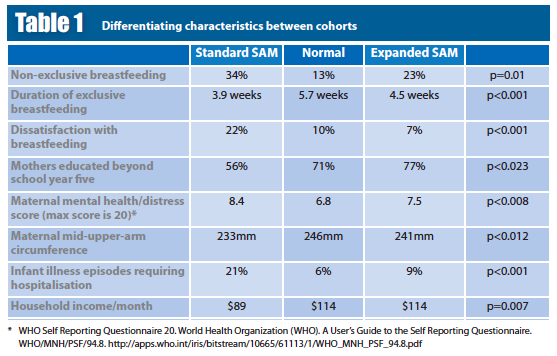
At enrolment, ‘Standard SAM’ and ‘Expanded SAM’ were younger than ‘Normal’ infants (5.1, 5.5, 6.5 weeks respectively, p<0.001). A selection of characteristics that differed between these groups at enrolment is shown in Table 1. Type of toilet was significantly different among the groups; Standard SAM had more people with a pit latrine vs. a flushing toilet compared to the other two groups. Handwashing and source of water were not significantly different among the groups. Duration of breastfeeding was not significantly different among the groups.
At age six months, ~24% of ‘Standard SAM’, 1% of the “Normal”, and 5% of ‘expanded SAM’ infants had SAM (p≤0.001). Three infants with ‘Standard SAM’ died; compared to none in the ‘Normal’ group and one in the ‘Expanded SAM’ group.
In the Standard and Expanded SAM groups, significantly fewer infants were still being breastfed, more infants were fed anything other than breastmilk at enrolment and endline, and more infants were given animal milk at an earlier age, compared to the Normal group. Duration of exclusive breastfeeding was also shorter in both groups, mothers breastfed less often, had higher mental health/distress score and were significantly less satisfied when asked how breastfeeding was going. Maternal Body Mass Index (BMI) and MUAC were lower in the Standard SAM group. More infants in the Standard SAM group had at least one episode of illness that required hospitalisation at enrolment; this proportion (21%) had increased to 40% by endline.
Challenges to implementing the research included:
- Access to villages in the rainy season; surveyors had to cross many bodies of water with equipment including motorbikes.
- Randomly selected villages were geographically spread out, so travel time was high.
- Measuring anthropometry in infants <6m is difficult, especially length.
- The number of questions in the questionnaire was a challenge as many were necessary to ensure comprehensiveness.
Discussion and conclusions
A range of maternal, infant and environmental risk factors are associated with SAM among infants <6m. Successful future treatments should focus on a package of care rather than single interventions that include breastfeeding support; the nutrition, physical and mental health of mothers; infectious disease management; and water/sanitation/hygiene conditions. Over one quarter of the infants identified with SAM at the outset remained severely malnourished at six months of age; this suggests inadequate provision and/or access to treatment of SAM and a risky environment. It is necessary to distinguish these vulnerable infants from those who had recovered by six months; indicators in addition to anthropometry are probably necessary.
For more information, contact: Nicki Connell, email: nconnell@savechildren.org
References
WHO. Guideline: Updates on the management of severe acute malnutrition in infants and children. Geneva: World Health Organization; 2013.
1Presented at the ACF research conference, November 9th, 2016.


