Improving estimates of numbers of children with severe acute malnutrition using cohort and survey data
Summary of Research
Isanaka S, Boundy EO, Graise RF, Myatt M and Briend A. (2016). Improving Estimates of Numbers of Children With Severe Acute Malnutrition Using Cohort and Survey Data. American Journal of Epidemiology Advance Access, published November 17, 2016. DOI: 10.1093/aje/kww129
Location: Mali, Niger and Burkina Faso
What we know: National prevalence data is used to estimate the burden of severe acute malnutrition (SAM). Incidence is a more accurate measure of the burden of acute conditions such as SAM, but is more costly and time-consuming to obtain. An incidence-correction factor of 1.6, to estimate incidence from prevalence, is currently recommended.
What this article adds: A recent study developed an incidence-correction factor to estimate SAM burden from prevalence estimates and tested it with data from Mali, Niger and Burkina Faso. A pooled incidence-correction factor of 4.82 was estimated, generating a corrected SAM-burden estimate of 110.6 million (from 19 million). Country-specific incidence-correction factors varied between countries and over time, indicating context matters. Given this, a common incidence-correction factor is unlikely to be adequate. Country-level estimation of the incidence-correction factor using both survey and routine programme data with an estimate of programme coverage is necessary in the absence of prospective cohort studies.
Severe acute malnutrition (SAM) is reported to affect 19 million children worldwide (Black et al, 2013). This estimate is an extrapolation from 639 national surveys determining the prevalence of SAM in 142 countries. SAM is an acute condition, however, and affected children may recover or die within a few weeks. One consequence is that estimation of the burden of SAM by means of prevalence data collected in occasional cross-sectional surveys will miss some cases and underestimate the number of children affected. The burden of acute conditions like SAM is more appropriately represented by a measure of incidence that captures new cases over time. While prevalence estimates are relatively easy to obtain using cross-sectional surveys, estimates of incidence require longitudinal follow-up of a cohort and are more costly and time-consuming to obtain. In the absence of incidence data, a simple method for estimating disease burden has been proposed that corrects available prevalence estimates to account for incident cases using an “incidence-correction factor” (UNICEF, 2013).
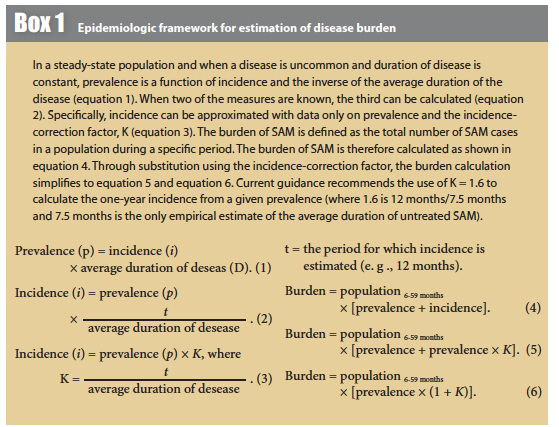
In this study, the authors used data from three West African countries (Mali, Niger and Burkina Faso) to test the hypothesis that a common incidence-correction factor may be used for estimation of SAM burden in all settings. The incidence-correction factor was estimated by the authors within the epidemiological framework described in Box 1. Meta-analysis was performed to calculate summary estimates for each country and for all three countries. Heterogeneity between countries and years was assessed using the I statistic.1
Findings
Prevalence and incidence data were available for multiple years in the three countries: Mali (2010-2012), Niger (2010-2011), and Burkina Faso (2009-2010). A pooled incidence-correction factor of 4.82 (95% confidence interval (CI): 3.15, 7.38) was estimated, although there was substantial between-country heterogeneity (I2 = 69%, P = 0.004). Within countries, there was evidence of heterogeneity over time in Niger (I2 = 80%, P = 0.02), where the country-specific incidence-correction factor ranged from 5.00 to 8.10. In contrast, there was no evidence of substantial heterogeneity across years in Mali or Burkina Faso; the pooled estimate of the incidence-correction factor was 2.53 (95% CI: 1.64, 3.89) in Mali and 13.25 (95% CI: 4.34, 40.48) in Burkina Faso. In secondary analysis, it was found that application of a mid-upper arm circumference (MUAC)-only definition of SAM (e.g. MUAC < 115 mm or oedema) resulted in little change in the incidence-correction factor compared with the primary analysis in Niger (K = 6.17 (95% CI: 3.86, 9.87) vs. K = 6.71 (95% CI: 4.81, 9.36)) or Mali (K = 2.53 (95% CI: 1.64, 3.89) vs. K = 2.67 (95% CI: 1.57, 4.57)). Variability in estimates was greater with cohort data than with survey data in Niger but lesser with cohort data in Mali.
Applying the pooled incidence-correction factor to the current global burden of SAM, the reported burden of 19 million children with SAM would be corrected to 110.6 million (95% CI: 78.9, 159.2) children affected. Given the variation in the incidence-correction factor across place and time found, the authors suggest the use of a common correction factor of 1.6 would still substantially underestimate the number of children in need and the importance of this condition.
Statistical heterogeneity suggests differences in the incidence-correction factor across settings; the pooled estimate in Mali (K = 2.57, 95% CI: 1.65, 4.00) was lower than that in Niger (K = 5.59, 95% CI: 3.31, 9.44). This between-country heterogeneity is consistent with the hypothesis that the relationship between prevalence and incidence is context-specific and may be related to differences across data sources or more general contextual differences. For example, the cohort in Mali included younger children aged 6-23 months and follow-up every three months. If incident cases were more likely to be missed in this context (due to the frequency of follow-up, for example), the incidence-correction factor would have been underestimated here. Similarly, if cases were systematically identified earlier or with fewer medical complications due to improved community-based screening or health infrastructure in Niger, the duration of SAM may generally be shorter and the incidence-correction factor larger in Niger.
There has been great interest in the expanded use of MUAC in the management of SAM. It has been suggested that use of MUAC as the single anthropometric criterion for screening, admission, monitoring and discharge would simplify management protocols, as well as target those children at highest risk of death (Briend et al, 2012), but the transition to MUAC-based management has been slowed by uncertainty surrounding the operational implications of such a change. This study shows that use of a SAM case definition employing MUAC as the sole anthropometric criterion did not materially change the estimates of the incidence-correction factor for burden estimation.
Given the potential for considerable variation in the prevalence-incidence relationship across place and time, the authors conclude that estimating the burden of SAM with a common incidence-correction factor is unlikely to be adequate. There is instead the need (as a minimum) for country-level estimation of the incidence-correction factor using a combination of survey and routine programme data with an estimate of programme coverage as an alternative to the optimal prospective (e.g. cohort) investigations. The Integrated Disease Surveillance and Response approach proposed by the World Health Organization Regional Office for Africa, which promotes the integration of multiple surveillance systems and recommends routine MUAC assessment, may also be a practical platform to obtain routine data on SAM incidence. Policy-makers and programme managers should be encouraged to explore inclusion of such sources of routine data collection so that context-specific estimates can be developed. In the absence of forthcoming data, estimates provided in this analysis may be considered for estimation of SAM burden in the countries studied.
See related article: Invited commentary: improving estimates of severe acute malnutrition requires more data
Footnotes
1A statistic that indicates the percentage of variance in a meta-analysis that is attributable to study heterogeneity.
References
Briend et al, 2012. Briend A, Maire B, Fontaine O and Garenne M. Mid-upper arm circumference and weight-for-height to identify high-risk malnourished under-five children. Matern Child Nutr. 2012; 8(1):130–133.
Black RE, Victora CG,Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382 (9890):427–451.
United Nations Children’s Fund (UNICEF). Global SAM Management Update: Summary of Findings. New York, NY: United Nations Children’s Fund; 2013


