Interventions to build resilience of the health system to the El Niño drought in Ethiopia
By Amal Tucker Brown and Eric Alain Ategbo
Amal Tucker Brown has worked for UNICEF since 2007 and joined UNICEF Ethiopia office in February 2015 as the head of the Community based nutrition and micronutrient unit. In 2015 Amal led the UNICEF emergency nutrition response and acted as interim nutrition cluster coordinator. Amal has previously worked for UNICEF in Madagascar, South Sudan, Somali, Malawi and Uganda and for NGOs in DRC, Niger and Rwanda.
Eric-Alain Ategbo has worked for UNICEF since 2003 in DRC, Niger, Uganda and India. He became Chief of Nutrition for UNICEF Ethiopia country office in 2016. Prior to UNICEF, Eric-Alain was the Head of Department of Nutrition and Food Technology of Faculty of Agriculture, Abomey-Calavi University (Republic of Benin).
UNICEF would like to acknowledge donors of this programme, including the Bill & Melinda Gates Foundation, ECHO, the Governments of Canada, Germany, Japan, Sweden, United Kingdom and United States who provided funds for the emergency response and cluster coordination.
The findings, interpretations, and conclusions in this article are those of the authors. They do not necessarily represent the views of UNICEF, its Executive Directors, or the countries that they represent and should not be attributed to them.
Location: Ethiopia
What we know: The resilience of the health system to withstand shocks and surge to meet caseload demands is critical in emergency-prone contexts.
What this article adds: Applying a resilience lens, UNICEF Ethiopia examined the experiences and impact of linking nutrition development programmes with a well-coordinated emergency response to the El Niño drought in 2015/16. Integration of severe acute malnutrition (SAM) treatment into routine health services and scale-up of the national Community Based Nutrition (CBN) programme were key to a quick, high-quality response that averted a humanitarian catastrophe. A strong, comprehensive nutrition information system was important for risk-informed planning and to inform nutrition-sensitive interventions; more real-time capture and use of data will build on these strengths (RapidPro is being explored). Challenges related to nutrition commodity and essential medicines supply were addressed, but these resources require further integration into the government supply chain. Greater awareness and capacity on infant feeding in emergencies (IFE) response is needed by government, donors and non-governmental organisations (NGOs). UNICEF is piloting a project to improve the link between nutrition services and the Productive Safety Nets Programme (PSNP) to better meet the needs of the most vulnerable and those at risk of shocks.
Background
Despite encouraging reductions in child undernutrition since 2000, the burden of malnutrition is still widely felt in Ethiopia. Stunting rates among children under five (U5) years old have decreased sharply (from 58 % in 2000 to 38 % in 2016); however nearly two out of five children are still stunted (CSAE, 2016). Nearly a quarter of children U5 are still underweight, and wasting affects one tenth of children country-wide (CSAE, 2016). Furthermore, a significant proportion of Ethiopia’s population is highly vulnerable to different forms of natural and complex disasters. Ethiopia’s vulnerability is a function of its geographical location, topography and its adaptive capacity. Agriculture-dependent livelihoods and pastoral economies are particularly vulnerable as unreliable rains impact food and nutrition security, which in turn particularly affects pastoralist households and smallholder farmers. Most of the Ethiopian population rely on rain-fed crop and livestock production (World Bank, 2015). In view of this precarious situation and following the 2011 Horn of Africa crisis, the concept of resilience was introduced into the development discourse in Ethiopia.
Rationale for resilience
Reducing malnutrition is a starting point in making households more resilient (Dufour, 2014). Given the high prevalence of malnutrition in Ethiopia, it is important to strengthen the resilience of the health system to withstand and recover from external shocks (such as drought) and stressors (long-term processes such as climate change) to meet high caseload demands.
Resilience includes the dimensions of absorptive capacity (coping skills to buffer the impact of shocks), adaptive capacity (adjustment to the impacts of a stressor) and transformative capacity (the ability to create a new system or way of life as required) (Hoddinott, 2014). To improve the country’s ability to withstand an emergency, programmes must use interventions that strengthen the absorptive, adaptive and transformative capacities of individuals, households and communities, as well as the health system as a whole.
In 2015 and 2016, Ethiopia was hit by the worst drought in decades. The failed 2015 summer rains (kiremt) that provide 80-85% of the country’s agricultural harvest threatened the food and nutrition security of the whole country, devastating livelihoods and increasing malnutrition levels. Recognising the gravity of the situation and increased needs, the Government of Ethiopia presented the 2016 Humanitarian Requirements Document (HRD), which estimated that 9.7 million people needed food aid on top of the existing eight million who are chronically food-insecure. The HRD predicted that 420,000 children would require treatment for severe acute malnutrition (SAM) and 3.2 million children and pregnant and lactating women (PLW) would be affected by moderate acute malnutrition (MAM).
Resilience in practice
Using the three dimensions of resilience, we examine how UNICEF supported Ethiopia by linking nutrition development programmes with a well-coordinated emergency response to the El Niño drought.
Absorptive capacity of the health system (ability to withstand the impact of shocks)
Due to the high SAM caseload in Ethiopia, in 2008 the Federal Ministry of Health (FMoH) integrated SAM management into the Health Extension Programme (HEP) at health-post level (village level) to increase year-round access and coverage of SAM treatment. The number of facilities equipped to treat SAM has since risen steadily: from around 400 in 2008 to over 15,000 just before the onset of the El Niño drought emergency, with a recovery rate today of over 90% and a death rate of less than 1% (Figure 1).
Figure 1: Trends in SAM programme quality 2008-2016
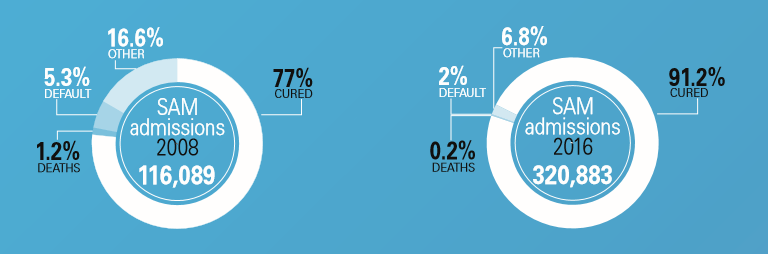
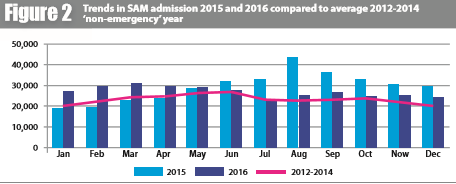
This improved resilience enabled the healthcare system to respond quickly and efficiently to the drought, reaching 350,451 SAM cases in 2015; a 40% increase compared to non-emergency years, and 320,883 cases in 2016; a 28% increase (Figure 2). The success of the 2015/2016 El Niño response compared to the 2011 Horn of Africa response is well documented (Babu et al, 2017).
Figure 2: Trends in SAM admission 2015 and 2016 compared to average 2012-2014 ‘non-emergency’ year
The UNICEF-supported emergency nutrition coordination unit (ENCU), which functions as the nutrition cluster in Ethiopia, has been compiling woreda-level1 SAM admission and programme quality data since 2008. This has enabled the ENCU to track monthly admissions for the whole country, establish seasonal trends and compare current admission levels to previous ‘good’ or ‘bad’ years. This allowed for timely alert of the upcoming emergency, ensuing early commitment of resources by donors, which resulted in the largest-ever procurement and decentralised preposition of ready-to-use therapeutic food (RUTF).2
In 2008, the Government of Ethiopia also introduced the Community Based Nutrition programme (CBN), the objective of which is to improve the nutritional status of mothers and children through cost-effective and sustainable interventions in communities. In 2012, the CBN was integrated into the HEP, with health extension workers (HEWs) responsible for implementing the activities and community volunteers, known as the health development armies (HDAs), responsible for mobilising community members to participate in the full range of CBN activities.
CBN coverage increased gradually from 39 woredas to 386 woredas in 2016, covering 55% of all children under two years old. CBN has been successful in reducing underweight prevalence among its participants from around 25% in 2008 to only 5% in 2016. To maintain the gains achieved in the prevalence of underweight, the programme was maintained during the emergency, resulting in only a slight increase in underweight prevalence to just under 6% compared to the regional average of 20%.3
Box 1: The Community Based Nutrition programme (CBN)
CBN activities include:
- Monthly growth monitoring and promotion (GMP) of children under two years of age for growth-faltering identification and appropriate counselling in agrarian regions.
- Targeted counselling on appropriate infant and young child feeding (IYCF) and childcare practices; water, sanitation and hygiene (WASH) practices; and maternal nutrition (individual, group and house-to-house counselling as needed).
- Community mobilisation and conversations on nutrition, WASH and health issues.
- Micronutrient deficiency control through vitamin A supplementation and deworming of children U5, deworming of pregnant women and supplementation of PLW with iron and folic acid.
- Screening for acute malnutrition in children U5 and PLW and referral for the treatment of acute malnutrition.
- Referral to health facility-based services for treatment of childhood illness (based on integrated management of childhood illness (ICCM)) and the HIV programme.
Figure 3: Underweight prevalence and participation in CBN programme compared to regional underweight prevalence (EDHS 2016)4
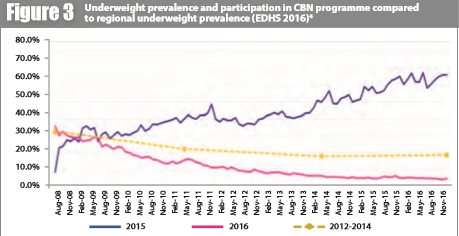
The CBN programme also contributed to increased quality of CMAM services during the emergency. Compared to non-CBN supported woredas, the UNICEF-supported CBN woredas5 had better CMAM cure rate (92% vs. 90%; a difference of 8,400 SAM cases), reporting rate (93% vs 55%), SAM treatment coverage (95% vs 76%) and screening coverage (71% vs 61%). In addition, they had lower death rates (1% vs 2%) and default rates (0% vs 3%). In the CBN woredas the children were therefore not only less likely to be malnourished, they were also more likely to be identified, treated and cured and less likely to default or die once admitted to the CMAM programme. This suggests that CBN, a development programme, was important in strengthening the system to enable it to respond quickly to the emergency and identify children who require SAM treatment.
Adaptive capacity of the health system (adjustment to stress)
The ENCU leads a woreda-level hotspot classification system, with hotspot priority one being equivalent to a humanitarian emergency. This enables improved risk-informed planning of response according to the severity of the situation.
The SAM nutrition information system was enhanced by harmonising the regional and federal databases and aligning the SAM data schedule with the Health Management Information System (HMIS) schedule, thus reducing the minimum lag-time for data to reach federal level from eight-ten weeks to six weeks. This enabled improved risk-informed planning (see below); however the six-week lag-time remained a challenge in timely risk-informed planning throughout the emergency. Nevertheless, the improved analysis of the data highlighted health facilities with overwhelmingly high caseloads. In response, additional facilities were equipped to treat SAM cases and by the end of 2016, the total number of such facilities was 16,687, plus an additional 49 mobile health and nutrition teams (MHNTs) for hard-to-reach and underserved areas.
Prior to the emergency, active screening was conducted every three months in agrarian regions and every six months in pastoralist areas, with passive screening conducted all year round as and when the population accessed the health facility. This resulted in large peaks in admissions, as well as late referral of SAM cases for treatment. In July 2015, the FMoH sent out a directive to all health facilities to shift from quarterly to monthly active screening in all hotspot priority-one woredas. This resulted in a marked increase in the number of SAM cases identified and a reduction in the number of SAM cases with complications. However, this approach also caused screening fatigue (of the population and the HEW), leading to a reduction in screening coverage over time, as well as an increased workload on the HEW. This highlighted a need to review existing screening methods.
Transformative capacity of the health system (new ways of working)

In Ethiopia the role of international non-governmental organisations (INGOs) has shifted from direct service delivery in 2003 to technical backstopping, capacity-building and logistic support in priority-one woredas (Andert et al, 2017). But, with as many as 219 priority-one woredas during the emergency, further prioritisation was needed. ENCU developed a woreda capacity-mapping tool to assess each woreda’s capacity to support the increased need. The tool was developed using routine data, such as CMAM programme quality indicators, caseload per facility, proxy prevalence of MAM and SAM as defined by mid-upper arm circumference (MUAC) screening, physical accessibility and distance from regional health bureau. This guided INGOs towards woredas with limited capacity and was used to alert donors for additional funds. Local non-governmental organisations (NGOs) were not able to access emergency funds and had limited capacity to respond at woreda level. However, as described in Andert et al, 2017, GOAL sub-granted funds to local NGOs and provided technical oversight.
UNICEF is responsible for procuring and distributing nutrition supplies at regional level; the government distributes these supplies to lower-level health tiers, along with essential medication to treat SAM cases with complications. This dual delivery system was uncoordinated and affected the quality of SAM treatment. To address this, UNICEF worked with the government to provide and distribute standardised treatment kits. The World Health Organization (WHO) supported the FMoH to coordinate the health cluster and ensured that the essential drugs from FMoH were sufficient to meet the SAM caseloads as well as the paediatric needs of the country.
Protecting infant and young child feeding (IYCF) practices is essential to prevent increases in mortality, disease and malnutrition. Protecting IYCF during an emergency (IYCF-E) is even more important as crowded living conditions and lack of water in some communities, particularly those displaced by the drought, increase the risk of disease incidence.
Field visits by UNICEF and partners found that breastfeeding was being interrupted during the emergency. Following UNICEF and partners’ advocacy efforts, the FMoH introduced IYCF-E into the response for the first time, using the CMAM platform and development programmes such as the CBN to reach a higher number of caregivers. However, IYCF-E implementation, namely training of HEW on IYCF-E support to women at the lower level,6 was delayed due to late prioritisation of IYCF-E by donors and lack of IYCF-E skills by many partners. The FMoH recognised the importance of IYCF-E and will be incorporating it (specifically how to identify the risks in the community during an emergency and how to support mothers/caregivers in assuring optimal IYCF) into the national integrated refresher training for HEWs and into all future trainings for health staff. Additional capacity-building of INGOs is necessary to ensure they are equipped to support the FMoH on IYCF-E in future emergencies.
Nutrition data were used by the food security cluster to prioritise general food distribution (GFD). This helped ensure that woredas with a high SAM/MAM caseload were reached first. The data were also used by the water, sanitation and hygiene (WASH) sector to identify woredas requiring immediate WASH interventions. This convergence of activity and better targeting proved to be an essential part of the response. However, further work is needed to develop a minimum package of WASH/nutrition/GFD intervention and to take account of protection issues in order to deliver a multisector response.
Lessons learned
The integration of SAM treatment into the routine health service package, along with the scale-up of the CBN programme, were key to responding quickly with high-quality services to the emergency, thereby averting a humanitarian catastrophe. There is a need now to look at how HEWs can be strengthened to identify local triggers to shocks and tailor their activities to respond to the emergency context before a full emergency is declared. A strong and comprehensive nutrition information system was important for risk-informed planning, which ensured adaptive and transformative actions. However, real-time monitoring is necessary to accelerate the availability of data from health posts for quicker planning and action at all levels. High-quality nutrition information was also essential for other clusters to prioritise woredas for nutrition-sensitive interventions.
Moving forward
The Productive Safety Net Programme (PSNP) was introduced in Ethiopia in 2005. It is one of the largest social protection programmes in Africa, covering approximately eight million people, including 11% of all rural households (15% of all female-headed households in rural areas). In 2015, the PNSP was modified to be more nutrition-sensitive and the new PSNP4 was launched in 2016. At the higher level, nutrition indicators (stunting in children U5 and household dietary diversity (HDD)) were included as a major programme outcome. At the grass-roots level, provision was made to exempt pregnant women in PSNP households from public work; non-PSNP households with SAM cases could become transient beneficiaries of PSNP and PSNP public workers (mainly men) could trade half a day of labour to attend an education session including nutrition, child protection and hygiene, and sanitation. The emergency showed that only 60% of SAM cases in PSNP households were reached. In addition, there was no referral system for SAM children from non-PSNP households to receive temporary support. UNICEF is piloting a project to improve the link between nutrition services and the PSNP which will not only strengthen the resilience of the health system to respond to emergencies, but also contribute to household resilience, thus protecting the malnourished child.
RUTF is already part of the government essential medicines list. UNICEF, along with WHO, is part of the technical working group supporting the government in the integration of nutrition commodities into the government pharmaceutical supplies management system for a more sustainable and coordinated delivery of nutrition supplies in emergencies.
Finally, UNICEF is in continuous discussions with the government to introduce real-time monitoring, such as RapidPro (Box 2), into the health system to reduce lag time from facility to regional and federal level for quicker risk-informed planning.
Box 2: RapidPro
UNICEF Innovation has been working with SMS systems since 2007; RapidPro was developed in 2014. It is a free, open-source framework designed to send and receive data using basic mobile phones, manage complex workflows, automate analysis and present data in real-time.
UNICEF Ethiopia has been exploring with FMoH the possibility of introducing RapidPro for improved and speedy data collection into Ethiopia. HEWs can use their personal mobile phones to register and send data, so there is no need to procure special IT materials, tablets or phones. Following a one-day training on how to register their phone and send programme data to the RapidPro server, the HEW can start to share key programme data such as screening data, SAM admissions and nutrition commodity stocks rapidly.
By having the server at FMoH, sensitive information will be contained within Ethiopia and approval at every level will ensure that sharing of sensitive data is controlled. As there is only one telephone provider in the country, negotiation with this provider will ensure that the HEW does not incur any cost when sending/receiving SMS.
The system can be tailored to the Ethiopian context, designed to recognise critical events and immediately send warnings to those responsible for responding. The system would also produce regular automated reports to send to all necessary programme staff from district to national level.
For more information, contact: Amal Tucker Brown, email: atuckerbrown@unicef.org
References
Andert C, Muzeiyn Z, Barthorp H and O’Mahony S. (2017). CMAM scale-up: experience from Ethiopia’s El Niño response 2016. Field Exchange 54, February 2017. p11. www.ennonline.net/fex/54/cmamelninoethiopia
Babu G, Rutishauser-Perera A and Prudhon C. (2017). Assessing the differences in the scale of nutrition response efforts to El Niño in Ethiopia. Field Exchange 54, February 2017. p98. www.ennonline.net/fex/54/elninoinethiopia
CSAE 2016. Central Statistics Agency Ethiopia, 2016. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. October 2016.
Dufour AO. (2014). Strengthening the Links between Resilience and Nutrition: A proposed Approach, IFPRI.
Hoddinott J. (2014). Understanding Resilience for Food and Nutrition Security, IFPRI.
World Bank (2015). Ethiopia Poverty Assessment, 2014.
1Districts, or woredas, are the third tier of administrative unit in Ethiopia. They are further subdivided into wards (kebele) or neighbourhood associations, which are the smallest unit of local government.
2http://www.unicef.org/esaro/5440_eth2016_therapeutic-food.html
3Taking into account woredas that were supported by an NGO during the emergency.
4See footnote [3]
5See footnote [3]
6Establishment of breastfeeding friendly spaces were deemed not necessary in the majority of cases (IYCF indicators were integrated in all displaced population rapid assessments) apart for Siti Zone in Somali region where the drought affected population movement.


