MUAC vs WHZ in predicting mortality in hospitalised children under five years of age
Summary of research1
This research contributes to the evidence base regarding which anthropometric indicators identify malnourished sick children most at risk of death. Low MUAC hospitalised children were twice as likely to die as low WHZ children. While it makes sense to prioritise these low MUAC children, the case remains that one third of the children with WHZ< -3 not identified by MUAC had an elevated risk of dying. Arguably, intervention for these children is still justified (Eds).
Location: India
What we know: Both weight-for-height z score (WHZ) and mid-upper arm circumference (MUAC) identify children at increased risk of death.
What this article adds: A diagnostic test accuracy study was carried out in a paediatric emergency department in India to determine the performance of MUAC compared with WHZ as a predictor of mortality among children aged 6-59 months (n=1,663). MUAC < 11·5cm, WHZ<−3 and weight-for-age z-score (WAZ)<−3 all independently predicted inpatient mortality. However, MUAC was a significantly better predictor of mortality than WHZ, WAZ and height-for-age z-score (HAZ) in these hospitalised sick children. Using MUAC <11.5cm as the sole criterion misses one third of children at risk of dying but identifies those most at risk of death; risk of death in children with MUAC<11·5cm was more than twice the risk than for children with WHZ<−3 and MUAC>11·5cm. MUAC of <11·5cm is suggested as a priority indicator to triage children for therapeutic interventions in resource-limited settings.
 In hospitalised Indian children, malnutrition increases six-fold the risk of mortality associated with both diarrhoea (Behera et al, 1980) and acute respiratory tract infections (Sehgal et al, 1997). Weight-for-height z score (WHZ) for identi?cation of SAM has practical challenges, including difficulties in accurately weighing and measuring length in sick children; unavailability of calibrated weighing scales and height boards; the need for reference charts; and the complex calculations to derive and interpret WHZ. Recognising these operational dif?culties, mid-upper arm circumference (MUAC) <11·5cm is recognised internationally as an age- and sex-independent diagnostic criterion for SAM, alongside WHZ<−3. However, WHZ and MUAC often do not identify the same children. In addition, very few studies have directly compared MUAC<11·5cm with WHZ<−3 for predicting child mortality. The purpose of this study was to determine the performance of MUAC compared with WHZ for predicting deaths among hospitalised children aged six months to five years in Indian settings and to determine the optimum cut-off value of MUAC to predict mortality in these children.
In hospitalised Indian children, malnutrition increases six-fold the risk of mortality associated with both diarrhoea (Behera et al, 1980) and acute respiratory tract infections (Sehgal et al, 1997). Weight-for-height z score (WHZ) for identi?cation of SAM has practical challenges, including difficulties in accurately weighing and measuring length in sick children; unavailability of calibrated weighing scales and height boards; the need for reference charts; and the complex calculations to derive and interpret WHZ. Recognising these operational dif?culties, mid-upper arm circumference (MUAC) <11·5cm is recognised internationally as an age- and sex-independent diagnostic criterion for SAM, alongside WHZ<−3. However, WHZ and MUAC often do not identify the same children. In addition, very few studies have directly compared MUAC<11·5cm with WHZ<−3 for predicting child mortality. The purpose of this study was to determine the performance of MUAC compared with WHZ for predicting deaths among hospitalised children aged six months to five years in Indian settings and to determine the optimum cut-off value of MUAC to predict mortality in these children.
Method
The authors used a diagnostic test accuracy study in a paediatric emergency department of a tertiary care hospital catering to a semi-urban and rural population in Delhi, India. Hospitalised children aged six months to five years were consecutively recruited over 14 months. Children admitted for diagnostic purpose with obesity, congenital anomalies, gross ascites, generalised anasarca, non-nutritional short stature and for whom outcome on discharge could not be recorded (left against medical advice, referred to other hospitals) were excluded after thorough clinical examination.
MUAC (cm), weight (kg), height (cm), clinical details and the outcome were recorded. MUAC was measured with a non-stretchable Te?on measuring tape. Infants were weighed on a pan-type of digital weighing scale; older children who could stand by themselves were weighed on a platform-type weighing scale. Length was measured in children less than two years old using an infantometer; standing height was measured for children more than two years old on a stadiometer. MUAC was compared with WHZ based on the 2006 WHO growth standards for predicting the outcome. Receiver operating characteristic (ROC) curves were constructed to ascertain the predictive values of MUAC, WHZ, weight-for-age z score (WAZ) and height-for-age z score (HAZ) for inpatient mortality in terms of area under the curve (AUC) with 95% con?dence interval (CI). Areas under ROC curves were compared using the χ2 test and multiple pairwise comparisons were done, with P<0·01 considered signi?cant.
Results
Of 2,389 children aged six months to five years hospitalised during the study period, 1,959 (82·0%) were eligible for inclusion. Of the 1,663 children ?nally included, 24·5% (n=407) were infants aged 6-11 months. The median age of the study population was 23 months.
The most common diagnoses on admission were seizure disorder (32·1%, n=533), pneumonia (19.4%, n=323) and diarrhoea (12·4%, n=206). Others included nutritional anaemia (4·6%, n=77), meningoencephalitis (6.4% n=106, 6·4%), poisoning (5.5%, n=92), septicaemia 2.9%, n=48), infection (malaria and dengue fever (1.6% each, n=26 each), enteric fever (1.5%, n=25) and tuberculosis (n=26, 1·6%).
Mean WHZ, WAZ and HAZ for the enrolled children were −1·5(SD 2·0), −2·2(SD 1·6) and −1·9(SD 1·7), respectively. Overall, 849 (51·1%) children were underweight, 788 (47·4%) were stunted and 643 (38·7%) were wasted. Severe underweight, severe stunting and severe wasting were present in 482 (29·0%), 420 (25·3%) and 372 (22·4%) children, respectively.
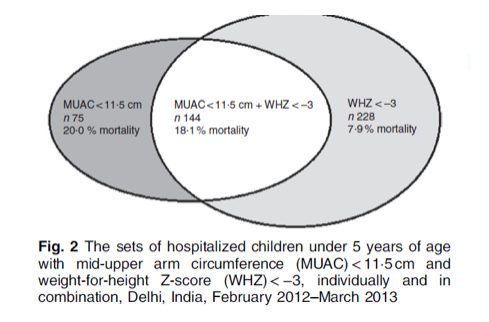
The median MUAC was 13·0 (IQR 12·2–14·0) cm. MUAC<11·5cm was seen in 219 (13·2%) children; of these, 75 (34.3%) had MUAC<11·5cm but WHZ≥ −3, while 144 children (65.7%) had both WHZ<−3 and MUAC <11·5 cm (see Figure 1). Sixty-one per cent (n=228) of children with WHZ <-3 had MUAC≥11·5cm. Only 17 children had oedematous malnutrition.
Seven per cent (n=124) of children died during the study. Children who died had significantly
lower values for MUAC, head circumference, body mass index (BMI), WAZ and HAZ. The mortality percentages for MUAC<11·5 cm, severe wasting and severe stunting were 18·7% (41/219), 11·8% (44/372) and 8·1% (34/420), respectively.
MUAC < 11·5cm (adjusted OR (95% CI): 3·7 (2·43, 5·60), P<0·001); WHZ<−3 (2·0 (1·37, 2·99), P<0·001) and WAZ<−3 (adjusted OR=1·602; 95% CI 1·096, 2·340; P=0·015) served as independent predictors of inpatient mortality. However, MUAC was a significantly better predictor of mortality with AUC=0·698 (95% CI 0·650, 0·746), compared with AUC=0·541 (95% CI 0·480, 0·602) for WHZ, AUC=0·574 (95% CI 0·520, 0·629) for WAZ and AUC=0·562 (95% CI 0·513, 0·611) for HAZ. There was no signi?cant difference among the AUC of WHZ, WAZ and HAZ (P value: HAZ v. WAZ= 0·68, HAZ v. WHZ=0·60, WAZ v. WHZ=0·04).
Although the sensitivity and specificity of MUAC<11·5 cm and WHZ<−3 for children at risk of dying appeared roughly similar, the sets of children identified by these nutritional indices differed, with only partial overlap (see Figure 1). The risk of death in children having MUAC<11·5cm was more than twice the risk in children having WHZ<−3 and MUAC>11·5cm. Combining MUAC<11·5cm with WHZ<−3 did not signi?cantly improve the diagnostic performance of MUAC<11·5cm. On balance, MUAC of <11·5cm had the best combination of sensitivity and speci?city (sensitivity 33·0%, speci?city 88·4%) for predicting inpatient mortality.
Figure 1: Hospitalised children 6-59 months of age: Overlap of MUAC and WHZ criteria
Discussion
In this study among hospitalised children aged six months to five years, MUAC was found to be a signi?cantly better predictor of mortality compared with WHZ<−3. WAZ was also identified as an independent predictor of mortality. MUAC <11.5cm and WHZ <-3 identify different sets of children with only partial overlap; using MUAC <11.5cm as the sole criterion missed one third of children at risk of dying but identified those at higher risk of mortality. The authors conclude that MUAC <11.5cm should be used to triage children for therapeutic interventions in resource-limited settings and that more focused studies are needed to identify anthropometric predictors of short-term mortality in children.
Footnotes
1Sachdeva S, Dewan P, Shah D, Kumar R, Malhotra RK and Gupta P. (2017). Mid-upper arm circumference v. weight-for-height Z-score for predicting mortality in hospitalized children under 5 years of age. Public Health Nutrition: 19(14), 2513–2520.
References
Behera SK, Mohapatra SS, Kar S et al. (1980) Incidence and mortality of hospitalized diarrhea cases. Part III. Indian Pediatr 17, 607–612.
Sehgal V, Sethi GR, Sachdev HP et al. (1997) Predictors of mortality in subjects hospitalized with acute lower respiratory tract infections. Indian Pediatr 34, 213 –219. 7. Deivanayagam N, Neduncheli


