Impact of nutrition education alongside treatment of moderate acute malnutrition in Madagascar
By Paul Sanyas, Brigitte Audras, Margot Magnin and Voahangy Rajaobelina
Paul Sanyas is a paediatrician who was in charge of the neonatology department of La Rochelle Hospital, France until 2014 (now retired). He worked for four years with Miray, a non-governmental organisation (NGO) in Madagascar. He is a member of the Board of Directors of L’APPEL, an international NGO.
Brigitte Audras is a paediatrician who worked for La Protection Maternelle et Infantile (PMI), a French public sector organisation. She is responsible for the development of the Nutricartes® method and is the former president of L’APPEL.
Margot Magnin is a dietician with a Masters Degree in Public Health from the University of Geneva.
Voahangy Rajaobelina is a doctor responsible for the Centres de Réhabilitation Nutritionnelle Ambulatoire de la Malnutrition Aiguë Modérée (CRENAM) for Miray in Antananarivo, Madagascar.
This article includes findings of a published study of the programme between 2010 and 20131
Location: Madagascar
What we know: The benefits of including nutrition education in moderate acute malnutrition (MAM) treatment programmes and long-term outcomes for programme beneficiaries are poorly documented.
What this article adds: In 2006, French non-governmental organisation (NGO) APPEL set up a programme in Antananarivo, Madagascar, to treat MAM children under five years of age. It includes treatment (locally produced fortified food) and maternal nutrition education (using a game-based participatory method called Nutricartes®), with a minimum stay (35 days from 2010-2013; 42 days from 2014 onwards) as per Ministry of Health protocol. A published retrospective, longitudinal study evaluated outcomes of 573 children aged 6-59 months enrolled in the MAM treatment programme between 2010 and 2013. During this period, supplementation was provided of 720kcal/d with nutrition education. Children attended an average of 38 days. On discharge, 82.2% had recovered (weight-for-height z score (WHZ) >-2) and 16.2% were mildly malnourished (WHZ <-1 and ≥-2). One year post-discharge, 79.1% remained recovered and 15% had mild malnutrition. Children from homes that chlorinated their water were 1.8 times more likely to have maintained their recovery at one year, compared to households with untreated water. In 2015 and 2016 dietary supplementation was reduced further while sustaining active nutrition education; recovery rates remained high. Findings suggest that a comprehensive MAM programme that includes nutrition education can achieve high short and long-term recovery rates.
Acute malnutrition affects 52 million children below the age of five worldwide (UNICEF, 2012) and is responsible for around 12% of deaths in this age group (Black et al, 2013). The prevalence of acute malnutrition in children below the age of five in Madagascar is 13% (ONN, 2010). In Madagascar and elsewhere malnutrition is often treated by programmes that are principally based on dietary supplements. Although the necessity of including educational and nutrition advice in malnutrition management protocols is often stressed, there is less evidence of the impact of these kinds of interventions. In addition, as the real challenge of a programme to treat malnutrition is to maintain acceptable recovery rates in the long term, there is a lack of information about long-term outcomes for post-programme bene?ciaries.
Programme to treat moderate acute malnutrition (MAM)
In 2006, APPEL (www.lappel.org), a French international non-governmental organisation (NGO), set up a programme at the request of the European Union (EU) and the medical branch of the Protestant church on the outskirts of Antananarivo to treat moderate acute malnutrition (MAM) in children under five years of age. Miray, a Madagascan NGO, runs 15 nutrition rehabilitation outpatient centres for MAM treatment (CRENAM) from the clinic. The staff of four midwives and four nutrition assistants work shifts in teams of two in the CRENAM once per week. Each year the outpatient programme admits around 2,400 malnourished children aged 6-59 months in the lower districts of Antananarivo.
The protocol for treatment of MAM has evolved over the last ten years but has always featured two aspects:
- A treatment component, with a dietary supplement in the form of Koba Aina (an enriched flour of high nutrition quality, made up of 99% local ingredients), which is made in Madagascar.2
- Educational component to prevent relapse, involving information, education and counselling (IEC), targeted mainly to mothers. This nutrition education is based on a participatory pedagogical method developed by Nutricartes® (see Box 1).
The acute malnutrition assessment criteria are based on the WHO 2006 weight-for-height Z score (WHZ), in accordance with the Malagasy Ministry of Public Health (MoPH). Nutrition status is graded as recovery (WHZ ≥ -1), mild acute malnutrition (WHZ < -1 and ≥-2), moderate acute malnutrition (MAM) (WHZ < -2 and ≥-3) and severe acute malnutrition (SAM) (WHZ < -3). Weekly screening is undertaken by community workers using mid-upper arm circumference (MUAC); MUAC <115mm indicates SAM, MUAC ≥115mm<125mm indicates MAM. An evaluation of screened children is then carried out by nutrition assistants who calculate WHZ. Children whose MUAC is <125mm but who do not meet WHZ admission criteria are reviewed after one month (there are no MoPH MUAC criteria for admission). Children with complicated SAM (with oedema and lack of appetite) are referred to hospital for inpatient treatment.
MAM children and an accompanying person, usually the mother, are enrolled into a group of about 10-12 children3 for a predefined period of treatment, as required by MoPH protocol (35 days from 2010-13; 42 days from 2014-2017). Children and their accompanying adult attend weekly sessions that last around two hours and include: anthropometric assessment; IEC for the accompanying person; a cooking demonstration; the on-site consumption of one portion of cooked Koba Aina; and the distribution of Koba Aina for the week ahead. The mother is most often present at the sessions, but sometimes the father comes alone or accompanies his wife. Occasionally, only the grandmother attends with the child. Height is measured at the beginning and end of the treatment programme.
Box 1: Nutricartes® learning tool
The Nutricartes® learning tool is made up of two games:
1. A food-based game made up of 150 cards with photos of different foods found in local markets and a game board with four colours: red (growth), yellow (energy), green (protection and micronutrients) and blue (hydration).
2. A health and hygiene game: 24 problem cards (such as dirty water and basic hygiene issues) and 24 solution cards (such as clean water, mosquito net) in the form of pictograms.
Half a day a week for six weeks, a group of 10 to 12 mothers whose children are receiving treatment participate actively in educational sessions on food and hygiene, based on this interactive, play-based and inclusive teaching model. The sessions are led by the nurse-midwife and the nutrition assistant according to the ‘Care Groups’ principles. This enables the participants to reveal their habits while playing cards, exchange information and share practices, and be encouraged to develop new habits. The sessions end with a cooking demonstration and food tasting. This educational programme is completed with the addition of family-planning advice, support on parenting and vaccination updates for children.
For more information, visit: www.nutricartes.org
Programme experience and developments
Between 2010 and 2013, the supplementary ration provided 720kcal per day, compared with the 1,000-1,500kcal per day recommended by the Malagasy MoPH; official authorisation was granted to lower the daily supplementation dose in favour of providing more nutrition and general education. The education component of the programme was based on Nutricartes® (see Box 1). The children ?nished the programme once they had reached the recovery threshold of WHZ >-1 and had completed a minimum of four week’s education. Published findings of a review of the programme for the period 2010 to 2013 are summarised in Box 2.
Box 2: Published review of nutrition programme in Madagascar (2010-2013)
A retrospective, longitudinal study was undertaken in 2013 to evaluate changes in the nutrition status of moderately malnourished children who took part in the supplementation/nutrition education programme between 2010 and 2013 (see main text for details). The study examined nutrition status (WHZ) on discharge and one year later and change in nutrition status over that period.
Study method
The study used data routinely gathered on programme completion and one year later. As part of the programme, randomly selected children were visited at home one year after discharge for anthropometric assessment and to complete a questionnaire covering personal, socioeconomic, clinical, food and general data. All 622 questionnaires completed between 2010 and 2013 were assessed as part of this study; 573 were included in the final analysis (49 were excluded due to errors, missing data or admission WHZ >-2). Children with uncomplicated SAM who were enrolled on the programme were also included. Children who did not have a four-week minimum stay were excluded.
It was not possible to locate all previously selected children at follow-up; hence they were replaced by other children from the nearest neighbourhood who had previously been enrolled in the programme. The extent of such substitution was not documented. Morbidity data was not reliable enough to include in the analysis.
Results
Study participants were aged between six months and five years on admission, except for one five-month old (0.02%). Average length of stay was 38 days (programme target was 35 days). Most children (94.4%) were admitted with MAM; 5.6% were SAM cases. At the end of the programme, 82.2% of the children met the recovery criteria (WHZ ≥ -1) and 16.2% had improved to mild acute malnutrition (WHZ < -1 and ≥-2). The recovery rate was higher among children admitted with MAM (83.9%) than those admitted with SAM (53.2%) (p = 0.0001). Those with MAM were four times more likely to achieve the recovery threshold than those with SAM, with an odds ratio (OR) of 4.0 and 95% confidence interval (95% CI) of 1.89–8.81.
At one-year follow-up, the global recovery rate was 79.1%; 14.8% were mildly malnourished, 3.5% were moderately malnourished and 1.6% were severely malnourished (see Table 1). Children admitted with MAM were more likely to be recovered at one-year post-discharge than those admitted with SAM (OR 2.6 (95% CI 1.25–5.74), univariate analysis). Children who had recovered at the time of exit were more than twice as likely to maintain that recovery after one year (OR 2.1, 95% CI 1.32–3.54). The recovery rate was statistically higher for children under 24 months old than for children older than 24 months at the end of the programme (OR 1.7, 95% CI 1.11– 2.75) and one year after the programme (OR 2.9, 95% CI 1.93–4.59). Children of families that used chlorination to treat water were 1.8 times more likely to have maintained their recovery at one year than households that did not treat their water (OR 1.8, 95% CI 1.12–2.95).
Multivariate analysis confirmed the significant effect of age (OR 2.0, 95% CI 1.23-3.13, p=0.004), admission WHZ (OR 4.6, 95% CI 2.08-10.09, p<0.001) and gender (OR 2.0, 95% CI 1.29-3.17, p=0.002) on the recovery rate at the time of programme exit. The multivariate analysis also demonstrated that age (OR 3.2, 95% CI 2.07-5.04, p<0.001), admission WHZ (OR 2.6, 95% CI 1.13-5.96, P=0.024) and water treatment (OR 1.2, 95% CI 1.01-1.42, p=0.031) significantly influenced nutrition status at one year after the programme, while gender (OR 1.2, 95% CI 0.76-1.86, p=0.422) no longer played a significant role. Contrary to the result of the univariate analysis, in the multivariate regression the effect of the exit WHZ (OR 1.7, 95% CI 0.99-2.85) was no longer significant, with a p-value of 0.052.
The 2010-2013 study demonstrated that this comprehensive outpatient MAM treatment programme, which puts a strong emphasis on nutrition education, enabled a good recovery rate (82.2%) that exceeded Sphere Standards (75%) and was sustained one-year post-treatment (79.1%). These results were possible even though the quantity of flour distributed was 30-50% below national recommendations.
Source: Magnin M, Stoll B, Voahang R and Jeanno E. (2017). Most children who took part in a comprehensive malnutrition programme in Madagascar reached and maintained the recovery threshold. Acta Paediatr, 2017. June;106(6);960-966.
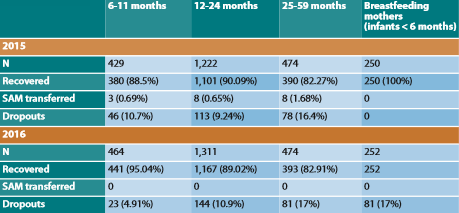
Post-2013, the programme continued with some modifications, based on the results of the published study. Most significantly, the dietary supplement was reduced to 308kcal/day for infants aged six to <12 months and 428kcal/day for children aged between 12 and 59 months. This supplement was provided for 42 days in accordance with MoPH guidance on minimum stay. On this reduced level of supplementation, combined with the same level of nutrition education using Nutricartes®, outcome data since 2014 are comparable to those recorded previously. Analysis of 2016 data finds that 95.04% of children under 12 months, 89.02% of children aged between 12 and 24 months and 82.91% of children over 24 months recover after 42 days of treatment (see Table 1; 2015 data also shown). One-year follow-up data is collected by the programme but is not formally analysed due to limited resources. Internal review of 50-80 cases per year suggests that recovery is sustained, although this is not scientifically proven.
Since 2015, the programme has also treated per year 250 undernourished lactating mothers (MUAC < 210 mm) with an infant under six months old. Some of these infants were likely low birth weight, although birth weight is not usually available to confirm this; none were acutely malnourished. These mothers received five weeks of therapeutic nutrition education and five weeks of the enriched flour (360kcal/day). All infants were exclusively breastfed and received no food supplements. All mothers achieved MUAC > 210mm by the end of the programme; 96.7% of infants had improved nutrition status. One year post-discharge, most infants remained on their normal growth curve or around WHZ -1; a small proportion (3.3%) were between WHZ -1.5 and -2.
Table 1: Outcomes on programme completion (42 days) among MAM children and mothers treated in 2015 and 2016
Discussion
The results from the 2013 study and subsequent programme experience provide reassurance that sustained recovery is possible using the described approach to MAM treatment. This approach includes nutrition IEC for mothers in small groups using Nutricartes® and advice on preparing balanced meals.
An important factor in achieving and sustaining nutrition recovery is exposure to and management of infectious diseases. While good nutrition of children will not suppress infectious diseases, a nourished child will have greater resistance to infection and will be better able to cope. An additional focus in small groups is therefore basic health and hygiene practices. The Nutricartes® game includes 24 ‘Hygiene’ cards that teach families how to prevent diarrhoea by drinking clean water (with advice on water chlorination) and how to reduce the risk of malaria through use of mosquito nets. One of the qualitative evaluation criteria for this programme, six months or one year after patient discharge, is the number of diarrhoeal episodes in the month preceding the survey and the number of medical consultations for infections within two to three months preceding the survey. Unreliability of this data has limited morbidity analysis.
Small groups also provide an opportunity to address other household constraints. Nutricartes® includes images such as alcohol, games, telephones and playing cards, which can be helpful in bringing to light financial constraints the family is experiencing and can help facilitate discussion about associated challenges and ideas on where savings can be made. The role of fathers is also important. Programme experience shows that fathers often become a supportive and positive influence in the family as they see their child rapidly recovering from undernutrition and associated illness.
The MoPH has been closely involved and consulted throughout the evolution of this programme. The programme is currently aiming to steadily decrease the amount of enriched flour given per day and the number of days it is administered. Ideally, children would be discharged as soon they have reached the target WHZ, rather than remain for the four-week minimum stay; however the MoPH directive must be complied with for the time being.
While continuing the MAM programme, the next proposed development is an additional approach to provide targeted nutrition education, in groups of 10-12, to mothers of children under two years of age who attend a health centre. This intervention will be provided for a five-week period, irrespective of nutrition status. No food supplementation will be provided. Children will be assessed on admission, on discharge and followed up after one year. We will compare the prevalence of acute malnutrition of these children to those attending another health centre where there is no education component. The hypothesis is that malnutrition can be reduced through nutrition education alone. This research will commence in 2018, pending funding. If successful, the aim is to introduce this method of nutrition education, based on the Nutricartes® tool, across all APPEL healthcare centres, to prevent undernutrition in children. Treatment for undernutrition using this method has also been developed by APPEL in Chad and Burkina Faso.
Conclusion
The context is complex and malnutrition in Madagascar is multifactorial, caused by poverty, poorly adapted nutrition practices and lack of access to clean drinking water. However, findings from the 2013 study show that following a four-week programme of nutrition and general educational sessions based on the Nutricartes® methodology, food supplementation, access to clean drinking water, improved vaccination coverage and parental support, nearly eight out of 10 children recovered from MAM on programme completion and had maintained that recovery one year later.
Routine treatment of MAM in Madagascar is based on daily nutrition support provided through supplementation with fortified food. However, findings from this study show that this approach must also be accompanied by nutrition education for families to reduce recovery time and avoid relapse, while taking family budget constraints into account. A game-based approach has enabled active participation by mothers attending the sessions to achieve this.
Findings of the 2013 study show that high levels of sustained recovery are possible with nutrition education even when the quantity of enriched flour distributed was 30-50% below national recommendations (1,000-1,500kcal/day). High rates of recovery were sustained when this was reduced further to 20-30% supplementation for infants aged six to <12 months and 29-43% supplementation for children aged 12-59 months, although more analysis is needed to confirm the effect one year later. Future pilots will test the efficacy of a nutrition education-only intervention to treat and prevent MAM. Current and future findings may have important cost-benefit implications, given that food supplements are generally the most expensive aspect of MAM programmes.
For more information, contact: Paul Sanyas, paul.sanyas@wanadoo.fr
1Magnin M, Stoll B, Voahangy R and Jeannot E. (2017). Most children who took part in a comprehensive malnutrition programme in Madagascar reached and maintained the recovery threshold. Acta Paediatr, 2017. June;106(6);960-966.
2Koba Aina is manufactured in Madagascar by Nutri’zaza, a local company. The product was created by GRET, a French company. It is purchased in bags weighing 20 to 30kg and staff distribute the weekly dose in small packets to the family. It is made of corn flour, Malagasy red rice flour, soy flour, peanuts, sugar, iodised salt, mineral salts and vitamins. Each 100g of the flour contains 360kcal, 10.9g of protein, 8.4g of lipids, 23.3mg of iron and 219mg of calcium, together with zinc and vitamin A.
3There were 20 children per group for the first couple of months of the study; this was subsequently reduced.
References
Black R, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child under nutrition and overweight in low-income and middle-income countries. Lancet 2013; 382: 427–51
Office National de Nutrition (ONN) (National Nutrition Office). Evaluation du plan national d’actions pour la nutrition (PNAN 2005–2009) (Evaluation of the National Nutrition Action Plan 2005–2009). Antananarivo: ONN, 2010.
United Nations International Children’s Emergency Fund (UNICEF), World Health Organization (WHO) and the World Bank. UNICEF-WHO-World Bank Joint Child Malnutrition Estimates. Levels and trends in child malnutrition. New York, NY: UNICEF; Geneva: WHO; Washington, DC: The World Bank, 2012.


