Cluster coordination in a government-led emergency response in Ethiopia
By Amal Tucker Brown, Orla Mary O’Neill and Ki Yeon Yoon
Amal Tucker Brown has worked for UNICEF since 2007. She joined UNICEF Ethiopia has head of the community-based nutrition and micronutrient unit in 2015; in the same year she acted as interim team leader of the Emergency Nutrition Coordination Unit (ENCU) (nutrition cluster coordinator). Amal also has experience working for UNICEF in Madagascar, South Sudan, Somalia, Malawi and Uganda and for NGOs in Democratic Republic of Congo, Niger and Rwanda.
Orla Mary O’Neill is currently the team leader of the ENCU in Ethiopia. She has over 15 years’ experience as a nutritionist with Concern and UNICEF in Bangladesh and Ethiopia in nutrition development projects and emergency nutrition response.
Ki Yeon Yoon is a monitoring and evaluation (M&E) professional with an increasing focus on nutrition. She joined UNICEF Ethiopia as Nutrition M&E Officer in 2015. Since the El Niño-driven drought, Ki Yeon has been increasingly involved in the UNICEF emergency nutrition response, including cluster coordination and information management.
UNICEF would like to acknowledge the donors, including the governments of Sweden, the United Kingdom and the United States, who provided funds for the cluster coordination.
The findings, interpretations and conclusions in this article are those of the authors. They do not necessarily represent the views of UNICEF, its executive directors, or the countries that they represent and should not be attributed to them.
Location: Ethiopia
What we know: The Government of Ethiopia responded quickly to the El Niño drought in 2015/16 and, due to its strong leadership, established the coordination mechanism and the resilience of the health system.
What this article adds: Overall coordination is led by the Ethiopian Government’s National Disaster Risk Management Coordination Commission (NDRMCC). The UNICEF-supported Emergency Nutrition Coordination Unit (ENCU), in existence since 2000 and aligned with the cluster approach, coordinates nutrition partners at federal and sub-national levels in emergency nutrition response via a range of coordination platforms. These govern assessment, information management, response planning and implementation. Tools developed to improve coordination include a woreda (district) capacity-mapping tool, cross-referenced with the 4-W matrix (who, what, where and when) to distinguish type and level of support needed by partners, and an accountability matrix to help define roles and responsibilities, resulting in more tailored, non-duplicative support to health services. Responding to the needs of the affected pastoral communities requires mobile and innovative approaches to secure access and capacity. High-level decision-makers in emergencies are non-nutritionists; orientation on nutrition in emergencies is critical. Government leadership ensures partner activities are aligned with government priorities; government-led assessment is critical with stakeholder involvement. The cluster provides key technical support and the platform to help bring different stakeholders together.
Context
Ethiopia has come a long way in reducing poverty and child undernutrition, with stunting prevalence falling from 58 per cent in 2000 to 38 per cent in 2016 (EDHS 2000, 2006, 2011, 2016). However, widespread poverty and malnutrition persist and the country remains disaster-prone and vulnerable to weather-related shocks. Vulnerability is predominantly rural and linked to land degradation, small land-holding, population pressure, outdated farming practices and highly variable rainfall, resulting in recurrent food insecurity and disease outbreaks.
In 2015 Ethiopia experienced one of the worst droughts in decades due to El Niño. The two rainy seasons, vital for supplying water for 80 per cent of Ethiopia’s agricultural production, failed. The crop failure resulted in a massive spike in humanitarian needs, with 10.2 million out of 92.3 million people requiring food assistance, 0.4 million children with severe acute malnutrition (SAM) and 1.7 million with moderate acute malnutrition (MAM) (HRD, 2016). This was against the backdrop of eight million people already suffering from chronic food insecurity in the country.
The Government of Ethiopia (GoE) was able to cope with the humanitarian shock and respond quickly to the El Niño-driven drought owing to its strong leadership, established coordination mechanism and the resilience of the health system. The success of the 2015/2016 El Niño response compared to the 2011 Horn of Africa response and the strengthening of health system resilience are well documented (Babu et al, 2017; Tucker Brown and Ategbo, 2017). This article focuses on UNICEF support to government-led coordination in response to the nutrition emergency.
Cluster coordination structure
In Ethiopia the overall humanitarian coordination is led by the National Disaster Risk Management Coordination Commission (NDRMCC)1 of the GoE with the support of the United Nations Office for the Coordination of Humanitarian Affairs (UNOCHA). The NDRMCC leads federal and regional-level Disaster Risk Management Technical Working Groups (DRMTWGs) across Ethiopia and hosts specialised task forces that work in tandem with the clusters/sectors, including nutrition, health, water, sanitation and hygiene (WASH), food security, shelter/non-food items (NFI), protection, education and agriculture.
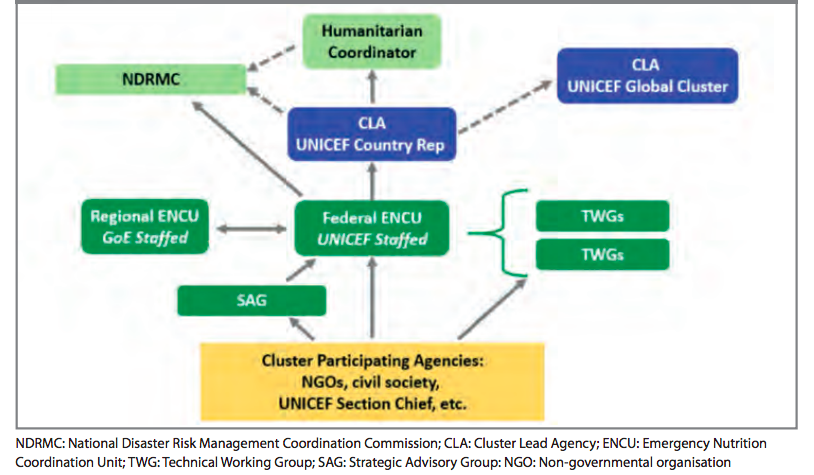
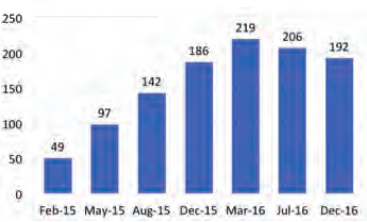
With technical support by UNICEF, the Emergency Nutrition Coordination Unit (ENCU) was formed by the GoE in 2000 within the Ministry of Agriculture to provide better coordination of NGO activity in the country. In 2007, following the introduction of the Inter-Agency Standing Committee (IASC) cluster approach, the Terms of Reference (TOR) for the ENCU were modified to be in line with the Global Nutrition Cluster (GNC). Nevertheless, the aim of the ENCU remained the same, which is to lead and coordinate nutrition partners at national and sub-national levels to provide coherent and effective emergency nutrition preparedness and response that can save lives and improve nutrition of people in Ethiopia during emergencies.The ENCU is supported by UNICEF as the Nutrition Cluster lead agency and is embedded within the NDRMCC at federal level and the Disaster Prevention and Preparedness Bureau (DPPB) in the six main regions (Afar, Amhara, Oromia, Tigray, SNNP and Somali) – a feature that is unique to Ethiopia. Both federal and regional ENCU employees were previously staffed by UNICEF; however, as part of its increased ownership of the cluster, the GoE has taken over regional staffing, while federal-level staff continue to be UNICEF employees. The federal ENCU is made up of a team leader (Nutrition Cluster Coordinator), deputy team leader, information manager and administrative assistant. The regional ENCU consists of a nutritionist and an information management officer (IMO) (see Figure 1).
Figure 1: Structure and accountability of the ENCU in Ethiopia
Coordination platforms
The ENCU participates in and chairs meetings across the GoE partners and donors to ensure cohesion of nutrition emergency-related information, planning and response. The ENCU co-chairs with NDRMCC monthly Nutrition Cluster meetings, known as the Multi-Agency Nutrition Task Force (MANTF), to address bottlenecks in planning and implementation. In addition, the ENCU and NDRMC co-chair the quarterly Strategic Advisory Group (SAG), with representation from the Federal Ministry of Health (FMoH) as well as elected partners from United Nations (UN) agencies, donors and NGOs. The SAG provides strategic guidance in formulating and reviewing the cluster strategy. Finally, extraordinary Technical Working Groups (TWGs) are established to discuss specific technical issues that may arise. At the regional level Nutrition Clusters are chaired by the Regional Health Bureau (RHB), with the ENCU nutritionist and/or IMO providing secretariat support.
In 2015, due to the severity of the drought, the FMoH established a Health and Nutrition Incident Command Post (ICP) in addition to the above mechanisms supported by the ENCU/NDRMCC. Modelled on a health sector approach, the ICP aimed at supporting the FMoH component of the emergency response. During the El Niño drought, the ICP met twice per week and worked closely with the NDRMCC and respective clusters. In 2017 the ICP was reinstated in Somali region to respond to the acute watery diarrhoea (AWD) outbreak and nutrition emergency and has proven a strong platform to trigger cross-sector engagement and government leadership2.
Coordinated assessment of the situation
Every year the NDRMCC leads two national multi-agency assessments: the meher assessment (around October/November) and the belg assessment (around June/July). These bring together some 200 government, UN, NGO and donor representatives who visit affected communities across Ethiopia. The information gathered from these visits, along with a review of current data on nutrition, health, population movement and meteorological predictions, is used to estimate the number of people in need of humanitarian assistance. This government-led, multi-agency approach increases cost-effectiveness and ownership and acceptance of the results by the humanitarian community.
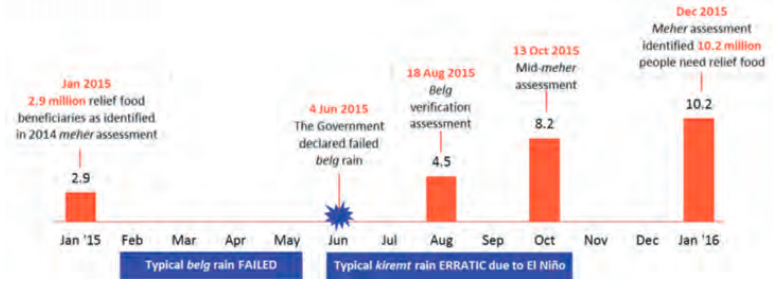
For the El Niño drought, the belg assessment in June-July 2015 concluded that 4.5 million people would be in need of emergency food assistance in August 2015. Following the erratic summer rains, the GoE decided to conduct a pre-harvest, rapid multi-agency assessment in early October 2015, which concluded that the number of people in need of assistance had increased to 8.2 million. This was followed by the meher assessment in late October, which revised the number further upwards to 10.2 million (Figure 2). This formed the basis of the 2016 HRD appeal for US$1.4 billion, of which US$115.4 million (US$135 million including NGO support) was needed for the nutrition response.
Figure 2: Timeline of the crisis
Hotspot classification
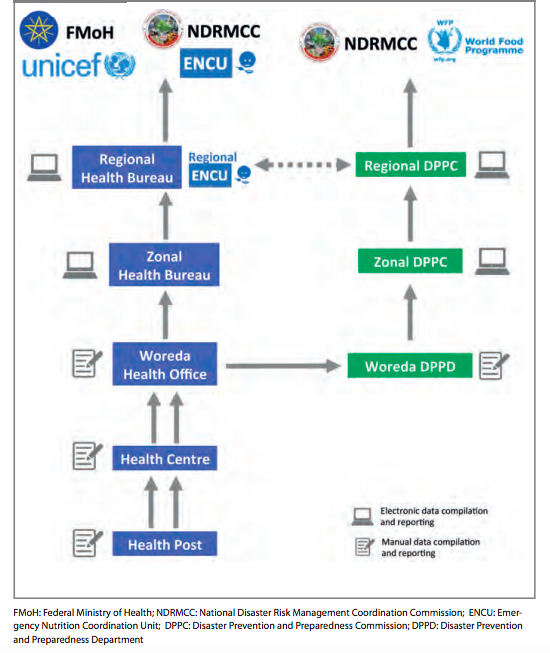
Based on the meher and belg assessments, the Household Economic Assessment (HEA) data, food security and early warning assessments, SMART surveys, disaster area assessments and routine programme data from multiple sectors, the regional and federal ENCUs lead a series of meetings at regional and then federal levels to classify woredas into different hotspot priorities to signal varying levels of vulnerabilities (Figure 3). During the El Niño drought, the number of priority one woredas – those in utmost need of humanitarian interventions –steadily increased from 49 in February 2015 to 186 in December 2015, reaching a peak of 219 in March 2016 (Figure 4).
At federal level the ENCU led a hotspot technical working group (HTWG) to review the suggested regional classification. The HTWG normally involves NDRMCC, FMoH, UNICEF and World Food Programme (WFP). In 2015/16, however, cluster leads from WASH, health, child protection, agriculture and food security were also invited to participate. This broad-based exercise contributed to building trust in the classification process and increased the use of quantitative data from different sectors. Nevertheless, the hotspot classification still heavily relies on subjective inputs and thus would benefit from inclusion of more objective criteria and cut-offs, given the increased availability of routine data from many sectors.
Based on the hotspot classification, humanitarian needs and current and past trends in acute malnutrition, the SAG collectively estimated the caseload for SAM and MAM. Prior to the El Niño emergency, caseload estimation was confined to a limited number of experts from UNICEF, WFP, FMoH and NDRMCC. Including the broader SAG members in this process led to an enhanced understanding and subsequent acceptance of the SAM and MAM estimations by the humanitarian community.
Following this process the ENCU presented the suggested hotspot classifications and caseload estimates to the NDRMCC management, who then validated the results and began planning for the response.
Figure 3: Definition and Classification of Hotspot Priority in Ethiopia
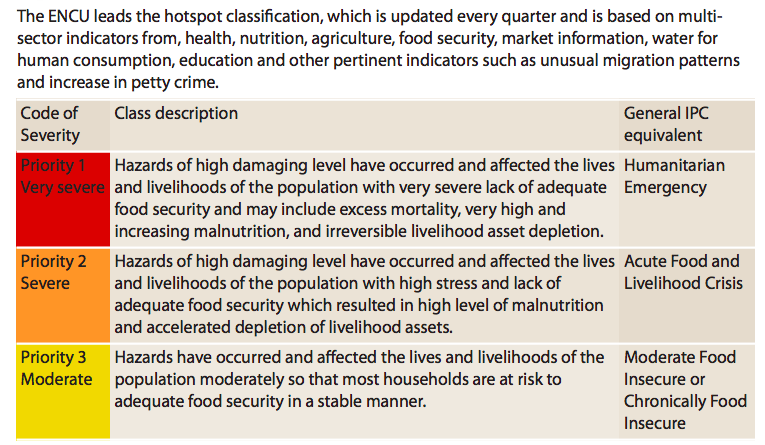
Figure 4: Trends in Priory 1 woredas 2015-2016
Coordinated planning
The SAG was responsible for drafting the response plan under the leadership of the ENCU team leader and NDRMCC representative. The response plan contributed to the HRD 2016 and was anchored in three strategic areas:
- Management of acute malnutrition, with a focus on enhancing SAM-MAM continuum of care.
- Prevention of acute malnutrition, including infant and young child feeding in emergencies (IYCF-E) and micronutrient deficiency control for children.
- Strengthening the coordination of the nutrition response, notably the core functions of the ENCU.
Cross-cutting issues were taken into account, such as inter-cluster coordination, gender and protection mainstreaming and linkages with development programmes. Advances in gender and protection mainstreaming were seen; however cross-sector programming remained challenging due to the diversity of needs.
Information management
Nutrition trends are monitored across the country via data, surveys and inputs from members of the MANTF. The ENCU manages multiple databases that consolidate data from government, UN and NGO sources, including: (1) The national therapeutic feeding programme (TFP) database for SAM management; (2) The national therapeutic supplementary feeding programme (TSFP) database for MAM management; and (3) The National database of surveys (including SMART and SQUEAC/Coverage Assessments) and rapid assessments. The flow of MAM and SAM management data is explained in Figure 5. The information system strengthening and challenges encountered during the emergency are detailed in an article by Tucker Brown and Ategbo (2017).
Figure 5: Flow for nutrition data reporting
Coordination of implementation
The El Niño response was one of the biggest emergency nutrition responses the GoE and partners encountered in terms of funding, number of stakeholders involved and complexity of implementation arrangements. The overall roles, responsibilities and achievements of each major implementing partner during the nutrition response are summarised in Box 1.
Box 1: El Niño nutrition response implementing agencies
Federal Ministry of Health
The emergency nutrition response is delivered primarily through the Health Extension Programme (HEP), implemented by government-employed health extension workers (HEWs) with support from partners. Under the HEP, the FMoH has built at least one health post and assigned two HEWs per kebele (sub-district) to provide preventative and basic curative services. At the community level the Women Development Army (WDA), a network of volunteers, links the neighbourhood with HEWs and is responsible for behaviour change communication (BCC) and community mobilisation (Figure 6). Some five health posts are supported by one health centre, staffed by nurses and providing more advanced curative services. Hospitals in densely populated towns and cities provide tertiary treatment for cases with severe complications.
In 2008 the FMoH integrated SAM management into the HEP to increase access and coverage of SAM treatment. The number of treatment facilities has since risen steadily from around 400 in 2008 to over 16,000 in 2016. At the same time, cognisant of the importance of prevention, the FMoH also introduced the Community Based Nutrition (CBN) programme. The CBN was gradually taken up by the FMoH as a key preventative and promotional nutrition programme.
These integrated nutrition programmes and community structures enabled the healthcare system to respond quickly and efficiently to the drought, reaching 350,451 SAM cases in 2015 and 320,883 in 2016, a 40 per cent and 30 per cent increase from non-emergency years, respectively.
The resilience-building efforts of the health system are further detailed in Tucker Brown and Ategbo (2017).
NDRMCC
Ethiopia adopted the community-based management of acute malnutrition (CMAM) approach to detect and treat acute malnutrition. However, the SAM management component of CMAM was integrated into the HEP, whereas MAM treatment was left under the Ministry of Agriculture and is now under the mandate of the NDRMCC. Screening for acute malnutrition is conducted by HEWs, with referral of SAM cases for treatment within the health system. MAM cases are referred to Food Distribution Centres (FDCs), where food distribution agents (FDAs) distribute MAM supplies. One FDC, equipped with two to three FDAs, caters for five health posts. WFP is supporting the GoE in the integration of MAM treatment into health posts in 44 woredas.
Partners
To avoid duplication and utilise the comparative advantage of each agency, WFP took the lead in supporting the NDRMCC with the treatment of MAM, whereas UNICEF, along with the World Health Organization (WHO), supports the FMoH in strengthening the overall health system to identify and provide quality and timely treatment for SAM and provide key preventative interventions. Considering the high caseload of acute malnutrition and the subsequent burden on the health system, NGO support to the woreda sector bureaus has been essential to ensure that quality services reach the most vulnerable and hard-to-reach. This is further illustrated in Andert et al (2016).
Following each hotspot classification, the ENCU requested NGOs to state who was doing what, where and when (4-W) to populate the 4-W matrix for effective coordination and identification of gaps (see Box 2). In the past the ENCU used a ‘one NGO to one priority one woreda’ approach for NGO support. However, with the quadrupling of priority one woredas over the course of the emergency and the serious shortage of trained nutritionists, this was not possible. (GOAL was one of the few NGOs able to expand quickly in response to the increased number of priority woredas, described in detail by Andert et al (2016)). However, as the response was mainly via the health system, many priority one woredas had the capacity to respond to the emergency with minimal support from NGOs.
To better identify the level of support needed for each priority woreda, the ENCU developed a woreda capacity-mapping tool, which was cross-referenced with the 4-W matrix to further refine the gaps and guide NGOs accordingly. The woreda capacity-mapping tool was based on routine data such as the hotspot classification history, CMAM programme performance (cure, default, death rate and reporting rate), average caseload per facility, coverage of SAM and MAM treatment sites, screening data and coverage, development programme presence, physical accessibility, and distance from regional health bureau. Data were collected by the regional ENCU and compiled into a single tool by the Federal ENCU. Using the above information and pre-defined cut-offs, it was possible to suggest the level of support that a woreda might need, ranging from high-intensity NGO support to partial support on system strengthening.
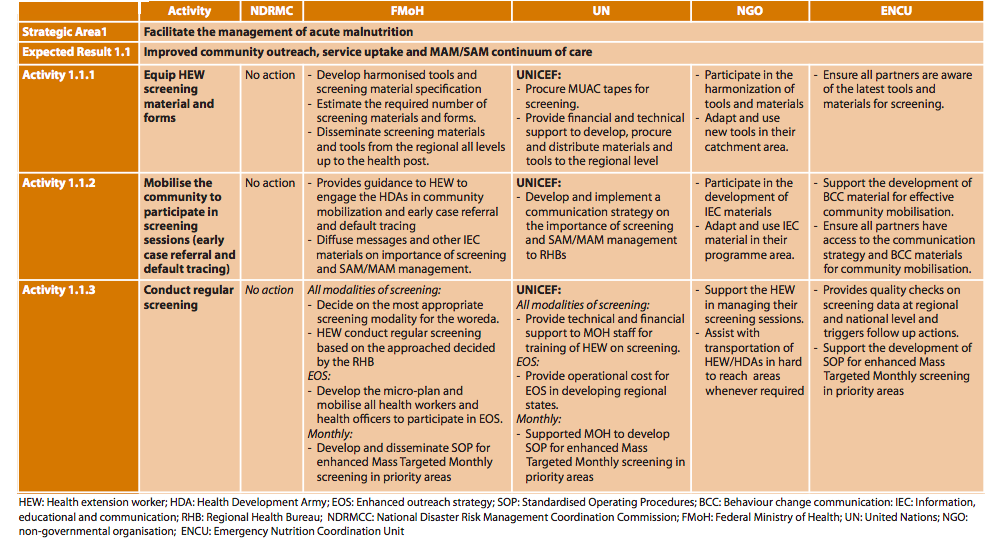
In addition, an accountability matrix was developed to clearly identify roles, responsibilities and accountabilities of each stakeholder in the response. The matrix was organised by the three strategic areas of the response plan. Under each area main activities and responsibilities/contributions were listed by each entity. The process was led by UNICEF for UN agencies, Plan International for NGOs, and the NDRMCC and FMoH for government. The ENCU consolidated the information into one coherent document (Figure 7).
Box 2: Tools for better response planning and coordination
The 4-W matrix was refined to include:
- Number of kebeles covered by each NGO to advocate for complete coverage in all woredas. - Details of the type of support provided (OTP, SC and TSFP) to encourage NGOs with limited capacity to pair up with each other to fill gaps in services.
- IYCF-E coverage to advocate for more donor and partner attention on this area.
- Hygiene-promotion activities to promote better inter-cluster coordination (it was not possible to do the same with other sectors due to the differing needs of each region).
Figure 6: Community-level health system structure in Ethiopia
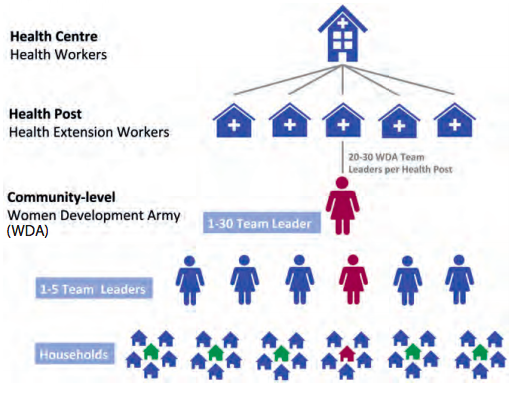
Figure 7: Example of the accountability matrix
Lessons learned
The strong and well established, government-led coordination system was key to an effective emergency response to the El Niño drought in 2015/16. However, main decision-makers at the peak of the emergency lacked technical understanding in nutrition, calling for frequent orientation on nutrition in emergencies (NiE). This likely delayed some critical decisions at the start of the emergency and highlights the need to examine how to orient high-level stakeholders on the basics of NiE. Despite this, involvement of government in cluster coordination ensured that partner activities were in line with government priorities. At the same time, decision-makers could utilise the UNICEF-supported Nutrition Cluster for technical guidance in the planning and execution of the response.
Government-led assessments are important to government ownership, including domestic resource mobilisation. In 2016 just under half of the US$1.4 billion funding needs were funded by the GoE. However, inclusion of multiple partners and sectors during the assessment, classification of priority woredas and the acute malnutrition caseload estimation proved to be essential in increasing transparency and acceptance of the results by the humanitarian community. The cluster remains the main platform to bring these different stakeholders together.
The large number of stakeholders and limited awareness with regard to supporting a government-led emergency response had the potential to lead to confusion and loss of accountability. The accountability matrix helped clarify roles and responsibilities and was developed in part in response to questions by the government on the added value of NGOs where the CMAM programme is relatively well established. The role of the NGO has, over the last ten years, been reduced to a ‘light touch’ approach, largely to gap-fill a parallel logistics system, provide refresher training and (where commodities are available) ensure monthly TSFP delivery, which remains outside the health system. There is a need to continue the dialogue on better defining the roles and responsibilities and subsequent accountability of partners in a government-led response.
With such decentralised services for the treatment of acute malnutrition, despite the peak in admission, average monthly admissions in 2015/2016 remained well within the capacity of the Government to manage; this capacity needs to be taken into account when mounting a response. The woreda capacity-mapping tool helped to identify woredas that FMoH was capable of managing and those that required a higher-level of partner engagement. This enabled more refined support to the health system to respond to the emergency, without creating a parallel system, over-stretching existing government health resources, or undermining efforts to strengthen the health system. The woreda capacity-mapping tool should be further tailored and linked to a set of region-specific triggers and responses in order to accelerate the decision-making process in identifying woredas in need of additional support to manage surges in acute malnutrition.
These newly developed tools, along with the various regional and sub-national coordination platforms, helped coordinate the multiplicity of partners and make best use of available resources, although continuous commitment from partners is needed to keep the tools updated and ready for use in future emergencies.
Immediate challenges and opportunities
In pastoral communities where the rollout of static CMAM services has lagged behind the highlands, resilience building of the health system is essential to respond rapidly to increases in SAM cases. This will require links to other sectors, given the high operational costs in pastoral areas and elevated health risks associated with disease outbreaks in areas where routine health services are challenged.
Regional leadership can better guide and promote cross-sector programming, monitoring and response, with particular attention to addressing context-specific needs at site level. The ICP model used to treat AWD was a new and successful approach in mounting an effective, multi-sector response to reduce the AWD outbreak at the time. The DPPB/RHB requested that the same strategy and approach be used to manage the nutrition crisis in Somali region, which arose in 2017 and continues.
Finally, until MAM management is fully integrated into the health system, external support will continue to be needed as this integration remains a priority. WFP and UNICEF have developed a roadmap to accelerate this integration under the leadership of the Ministry of Health and it is now under discussion between NDRMCs currently managing MAM treatment and FMoH.
For more information, contact: Amal Tucker Brown
Endnotes
1Formerly Disaster Risk Management and Food Security Sector (DRMFSS) and before that the Disaster Presentation and Preparedness Agency (DPPA).
2The ICP involved establishment of six pillars: case management, surveillance, logistics, WASH, coordination/information management, and social and behaviour change communication/communication for development (SBCC/C4D). Representatives from each cluster were appointed to chair, update and attend each of these pillars, thus ensuring that cluster inputs were well distributed across these aspects of operations, which are critical in the response.
References
Babu G, Rutishauser-Perera A and Prudhon C (2017). Assessing the differences in the scale of nutrition response efforts to El Niño in Ethiopia. Field Exchange 54, February 2017. p98. www.ennonline.net/fex/54/elninoinethiopia
Andert C, Muzeiyn Z, Barthorp H and O’Mahony S (2017). CMAM scale-up: experience from Ethiopia’s El Niño response 2016. Field Exchange 54, February 2017. p11. www.ennonline.net/fex/54/cmamelninoethiopia
Tucker Brown A and Ategbo EA (2017). Interventions to build resilience of the health system to the El Niño drought in Ethiopia. Field Exchange 55, July 2017. p94. www.ennonline.net/interventionstobuildresilienceofthehealthsystemtotheelniodroughtinethiopia
EDHS 2000, 2006, 2011, 2016. Ethiopia Democratic and Health Surveys 2000, 2006, 2011, 2016.
HRD 2016. Human Requirements Document, Ethiopia (2016). https://reliefweb.int/sites/reliefweb.int/files/resources/ethiopia_hrd_2016.pdf