Extending support through CMAM to older people in Ethiopia
By Kidist Negash Weldeyohannis
Kidist Negash Weldeyohannis is a Regional Health and Nutrition Programme Manager for HelpAge International, Africa region, with a special focus on humanitarian programming and response. She has previously worked with UNICEF and CARE in related fields and has a Masters in Public Health.
The author acknowledges the United Nations Office for the Coordination of Humanitarian Affairs Humanitarian Response Fund (UNOCHA-HRF) for financing the project described here, as well as Dr Luca Saraceno and Dr Juma Khudonazarov for reviewing this article and providing constructive feedback.
Location: Ethiopia
What we know: Africa has one of the most rapidly increasing populations of older people. There is a lack of national data on socioeconomic conditions and disease burden of older people in developing countries.
What this article adds: In 2016 a rapid assessment by HelpAge International identified high prevalence of global acute malnutrition (GAM) among older people in two drought-prone zones of Ethiopia (10 to 15 per cent). In response, HelpAge International intervened with a nutrition, water, sanitation and hygiene and livelihood intervention. Community-based management of acute malnutrition was limited to use of supplementary food in this age group due to ready-to-use therapeutic food shortfalls, health worker resistance and lack of relevant national guidelines. Complicated cases were referred to government services for treatment; a proportion received free care. External end-of-project evaluation was positive in terms of reported improvement in wellbeing, health conditions and weight gain (not quantitatively assessed). One quarter (26 per cent) of respondents were receiving relief food aid and 28 per cent were enrolled in the productive safety net programme. Challenges included lack of national guidelines on acute malnutrition management, data on older people not included in regular facility reporting, and older people not routinely included in needs assessments. Advocacy, capacity-building among local and international agencies to include and manage the older-age caseload and greater investment by donors are needed.
Situation of older people in Ethiopia
Africa has one of the most rapidly increasing populations of older people. Despite the impact of HIV/AIDS and other communicable diseases on life expectancy across the continent, people are living longer than ever before and the proportion of older people in Africa has increased almost fivefold. Over 40 million older people aged 60 years and over live in Africa; three million of whom are over 80 years of age. By 2050 the population of older people in Africa is projected to increase to 204 million.
Due to limited availability of age-disaggregated data, it is difficult to provide detailed analysis of the socioeconomic conditions of older people in Ethiopia. However, the 2007 Central Statistics Agency (CSA) census report indicated that 3,565,161 (about 4.8 per cent) of the total population are 60 years old and above (CSA, 2012). Of these, about 532,093 (14.9 per cent) live in urban settings, while the rest (85.1 per cent) live in rural areas, which follows a similar pattern to the whole population. The total number of older people is predicted to reach 5.3 million by 2020 (CSA, 2012).
Like many other developing countries, older people in Ethiopia are vulnerable to poverty, food insecurity, malnutrition, limited access to social and health services, and limited options for livelihoods diversification and security, regardless where they live (HelpAge, 2013). Furthermore, many older people require double protection in that they require care and protection themselves and at the same time support children, grandchildren and ageing spouses.

There is also global evidence of a large increase in the burden of non-communicable diseases (NCDs) among older people in low and middle-income countries, including cardiovascular diseases, hypertension, stroke, diabetes and dementia. In Ethiopia there is currently no countrywide research that shows the effect of NCDs on the health of older people, although the HelpAge study in 2012 found that 75 per cent of older people surveyed were suffering from one or more NCDs and, of these, only 75 per cent were receiving medical care (HelpAge, 2013). The shortage or non-existence of people trained in geriatrics and the management of NCDs, the deprioritising of older people for essential services, unaffordable healthcare costs and distance from health facilities all present major healthcare problems for older people in Ethiopia (HelpAge, 2013).
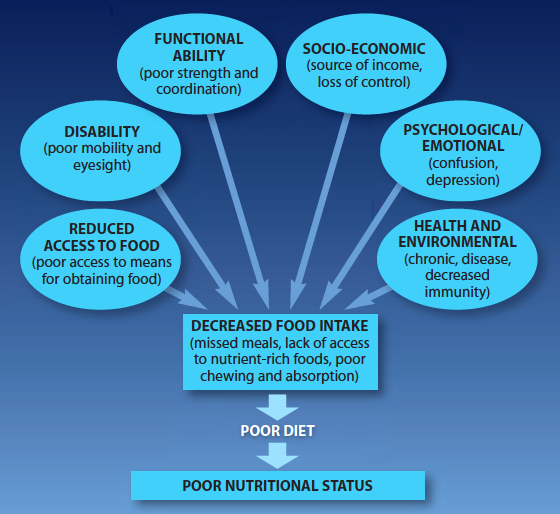
Adequate food and nutritional intake are critical for maintaining good health and are a key determinant of people’s ability to survive and recover from stresses and shocks in disaster-prone areas of developing countries. Older people have specific needs in relation to their general food intake, micronutrient requirements and palatability of food (See figure 1). This makes them particularly vulnerable to disruptions in food security in times of crisis. In droughts and food shortage situations, where the price of food is generally high, older people, who are often among the poorest, are frequently unable to afford enough food for themselves and their families. Furthermore, in cases of food insecurity, older people may choose to give their ration to younger members of their family.
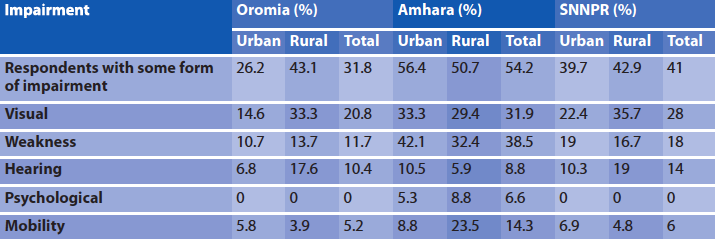
In addition to the worst impact of food insecurity, various (physical, sensory and cognitive) negatively affect older people’s food intake and increase their vulnerability to malnutrition. The risk factors underpinning undernutrition among older people are multiple and interconnected (see figure 1). According to the 2013 vulnerability assessment among older people conducted by HelpAge International in the Oromia, Amhara and Southern Nations and Nationalities Region (SNNPR) regions of Ethiopia, the percentage of older people with impairments ranged from 31.8 per cent in Oromia to 54.2 per cent in Amhara regions (HelpAge and EEPNA, 2013). Common forms of impairments reported were visual, physical weakness, mobility and hearing, which are highly related to poor production capacity, less income, poor food intake and malnutrition (see table 1).
Table 1: Impairment among older people per region in Ethiopia, 2013
Despite the growing body of evidence related to older people’s challenges in meeting their nutritional needs in emergencies, there are very few nutrition-specific interventions targeting older people in humanitarian situations, in contrast to pregnant and lactating women (PLW) and children under five years old, for whom intensive and targeted nutrition assistance is well-established practice. The lack of nutrition programmes tailored to older people also contrasts with basic humanitarian principles affirming that everyone has the right to humanitarian assistance which is impartial and non-discriminatory.
Figure 1: Nutritional risk factors for older people
HelpAge assessments and response
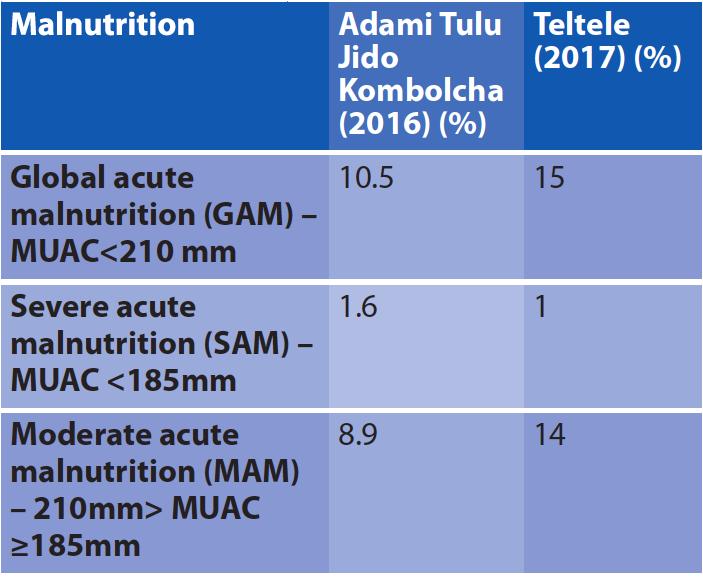
HelpAge conducted two rapid health and nutrition assessments in Adami Tulu Jido Kombolcha woreda1 of East Shewa zone (2016) and Teltele woreda of Borena zone (2017). Both indicated very high levels of acute malnutrition among older people, including a “serious” global acute malnutrition (GAM) rate in Adami Tulu Jido Kombolcha of 10.5 per cent and a “crucial” GAM rate in Teltele of 15 per cent. The Adami Tulu Jido Kombolcha assessment was conducted in a belg-producing area2 following the failure of the Meher harvest, which explains to some extent the high level of malnutrition (although no baseline data are available to compare with other seasons). The assessments were based on the rapid assessment method for older people (RAM-OP) which was developed in 2013 by HelpAge in collaboration with Brixton Health and Valid International. It is not recommended to assess bilateral pitting oedema in older people as oedema may be present due to other common health conditions in this age bracket. Table 2 summarises the findings of both assessments.
Table 2: Result of rapid nutrition assessment by HelpAgeBy Kidist Negash Weldeyohannis
Results of the 2016 assessment were used to advocate with donors for support to improve the conditions of older people in this area and meet their urgent needs. The United Nations Office for the Coordination of Humanitarian Affairs-Humanitarian Response Fund (UNOCHA-HRF) subsequently funded a project to provide life-saving support to older people for eight months between April and December 2016, implemented by HelpAge Ethiopia in four woredas of Oromia region (Adami Tullu Jido Kombolcha,Girar Jarso, Ziway Dugda and Abote). The project was implemented as a multi-sector response, integrating nutrition with water, sanitation and hygiene (WASH) and livelihood interventions, where the nutrition component was implemented only in Adami Tulu Jido Kombolcha and Girar Jarso woredas. While these two woredas benefited from nutrition, WASH and livelihood, the rest were targeted for WASH only. Major activities undertaken under each sector:
- Nutrition: Community mobilisation and screening, identification of acutely malnourished older people, referral of cases, provision of supplementary food, follow-up and referral of SAM cases to health facilities for further medical support.
- WASH: Rehabilitation of 15 water schemes that benefited 35,834 individuals, training of 124 WASH committees who manage the water points, promotion of hygiene and sanitation.
- Livelihoods: Provision of seeds and agricultural tools for 9,118 households (wheat, maize and teff3), training of agricultural extension agents and facilitation of follow-up and support in cultivating the seeds. As a vulnerable group, all older people identified as malnourished have benefitted from the seed support.
Project activities and achievements
The project areas are among the most drought-prone woredas in Ethiopia, where agricultural production regularly suffers from erratic rainfall and periods of drought. As a result, communities are highly vulnerable to food insecurity and other disasters. In January 2016 both woredas targeted for the nutrition support were categorised by the NDRMC/ENCU4 as hotspot priority one, following widespread El Niño-induced drought, which affected mainly the central highland part of six regional states during 2015 and 2016.
HelpAge implemented the nutrition component of the project using the community-based management of acute malnutrition (CMAM) approach, commonly used for the treatment of children and PLW with acute malnutrition. This is in line with HelpAge guidelines, based on experience with Médecins Sans Frontières in South Sudan, which recommend implementation of all four components of CMAM: community mobilisation; targeted supplementary feeding for treatment of moderate acute malnutrition (MAM); outpatient therapeutic programme (OTP) for treatment of SAM without complications (using ready-to-use supplementary food (RUTF)); and stabilisation centres (SCs) (using therapeutic milks) for treatment of SAM with complications. In practice it was not possible to implement the full CMAM guidelines due to supply shortages, resistance of some health workers and the lack of a national guideline; RUTF was not supplied by the regional health bureau to support this project, so only supplementary food was given for the treatment of MAM and SAM.
The activities were implemented through two local partners: Rift Valley Children and Women Development Organisation (RCWDO) and Sewasew Genet Children Development Organisation (SGCDO). Before the start of the project HelpAge trained 54 health workers (nurses and health officers), health extension workers (HEWs) and partners on basic principles of malnutrition among older people, including risk factors, diagnosis, treatment, follow-up and prevention of acute malnutrition. The HelpAge guideline for emergency nutrition response for older people was used to conduct the training (HelpAge, 2011). Practical demonstrations were given on how to use mid upper arm circumference (MUAC) tapes and how to screen for admission to SAM and MAM treatment programmes. As this was a new approach, 15 community health workers (CHWs) were also recruited and trained to lead and support the HEWs.
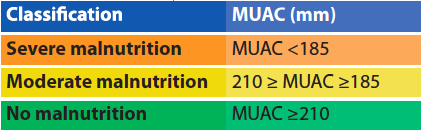
Intensive community mobilisation was conducted as part of the intervention by the project team, with the support of government at woreda and community levels in the two districts (HEWs, development agents and community management). Following mobilisation, people aged 60 years and above were screened for acute malnutrition by the HEWs with the support of project staff, using simple colour-coded MUAC tapes (see Table 2 for classification).
Due to funding constraints it was not possible to cover the whole of both woredas, only selected kebeles. These were selected in consultation with woreda officials and community leaders on the basis of the worst effect observed of the drought. As the HEWs and CHWs were used to identify and refer older people, it was assumed that maximum coverage could be achieved, although no coverage survey was undertaken to provide evidence of this.
Table 3: MUAC cut-offs for older people used in the TSFP
 Identified cases of SAM and MAM were provided with a ration card for the receipt of supplementary food through a targeted supplementary feeding programme (TSFP) established by the project. A monthly ration comprised 6.5kg of corn soya blend (CSB), 1 litre of vegetable oil and 1.5 kg of haricot beans. This was provided for three to four months. This basket of supplementary food provided 1,186 kcal and 41.8g of protein per person per day. This intervention was the first of its kind in both woredas and among the first emergency nutrition responses in the country to consider older people as a vulnerable target group.
Identified cases of SAM and MAM were provided with a ration card for the receipt of supplementary food through a targeted supplementary feeding programme (TSFP) established by the project. A monthly ration comprised 6.5kg of corn soya blend (CSB), 1 litre of vegetable oil and 1.5 kg of haricot beans. This was provided for three to four months. This basket of supplementary food provided 1,186 kcal and 41.8g of protein per person per day. This intervention was the first of its kind in both woredas and among the first emergency nutrition responses in the country to consider older people as a vulnerable target group.
The World Food Programme (WFP) ran a concurrent SFP in both target woredas, as with all priority one woredas; however, this was only targeted to children and PLW. It was not possible to procure supplementary food from WFP for older people within this programme due to significant funding constraints; therefore HelpAge ran a parallel programme, using food procured in country. Discussion is ongoing with WFP and the Nutrition Cluster for future streamlining of programmes if the funding situation allows.
During the seven-month project period, supplementary food was provided to 1,898 older people (965 of whom were older women) in the two districts. Of these, 1,733 were identified as MAM. The remaining 165 were older people with SAM. Since the project had no resources for supplies for the management of SAM or capacity to treat associated medical conditions, SAM cases were provided with a supplementary ration and referred to government facilities for further treatment. Through continued discussion and collaboration with the health office at the district level, it was possible for 29 cases of SAM with other medical conditions to receive free medical care in the health centre of Adami Tulu Jido Kombolcha woreda, in addition to receiving supplementary food from the project. No information on associated medical conditions or follow-up data was available for these referrals. The remaining SAM cases received supplementary food only.
MUAC of each beneficiary was measured monthly by HEWs and CHWs to determine whether discharge criteria were met. However, reliable data were not recorded and therefore it is not possible to know how many beneficiaries reached the discharge criteria within what timeframe. Data collection is an area that will be improved in the future.
The Government of Ethiopia, WFP and development partners assist chronically food-insecure people through transfers of food and cash during food-deficit periods under the Productive Safety Net Programme (PSNP). There is provision within this strategy for unconditional inclusion of older people in food-insecure households. However, no analysis was made of how many of the project’s beneficiaries were in receipt of PSNP support, although during the final project evaluation it was reported that 26 per cent of respondents were receiving relief food aid and 28 per cent were enrolled in the PSNP. HelpAge plans to focus on advocacy for access to the PSNP by older people in the future.
Feedback from partners and beneficiaries
An external final project evaluation was conducted in February 2017. A total of 390 households of older people were selected from the targeted beneficiaries using proportion-to-population size (PPS) sampling technique after selecting 50 per cent of the targeted communities purposively. A desk review of relevant documents complemented seven focus group discussions (FGDs) with project beneficiaries and 26 key informant interviews (KIIs).
Beneficiaries, local officials and stakeholders stated that the project contributed to a reduction in suffering and the prevention of life-threatening conditions among older people, particularly related to critical food insecurity. Older people reported they felt valued in the community when their nutritional needs were addressed, which was not the case during previous emergencies. Although quantitative evidence was gathered on recovery from malnutrition, older people reported that they had regained sufficient strength to perform their day-to-day activities.
Reported positive impact on the wellbeing of older people included improved physical condition and health status, such as weight gain, increased strength and greater ability to move from place to place. According to the household survey, 45.6 per cent of respondents reported improvements in their health conditions; 26.9 per cent reported improvements in their physical conditions; such as weight gain and increased strength; and 23.1 per cent reported that their health status was maintained. Eight-two per cent of older people (321/390) surveyed felt the TSFP was very important and relevant to their situation, while an additional 16 per cent reported it as important.
Challenges and lessons learned
Poor attention and priority are given to older people compared to children and women in emergency situations, particularly in terms of a lack of life-saving interventions. While lack of resources is the main constraint, there is also limited evidence of the vulnerability of older people and the impact of addressing their needs on household wellbeing. There is also poor visibility; older people are rarely included in national-level needs assessments.
There is no nationally adopted guideline in Ethiopia for management of acute malnutrition among older people and no mandate to include older people in screening for acute malnutrition. This contributes to resistance of donors and partners to include older people as a vulnerable group.
Although the needs in the project area were great, available resources for the project were limited, so it was only possible to implement the project in parts of the target woredas (focusing on hotspot kebeles).
Data collection and reporting of this activity was not included in regular health facility reporting tools; this greatly affected the quality and availability of data required to calculate important performance indicators such as cure rate, default rate and death rate of enrolled beneficiaries. This issue will be mitigated in future programing by developing a strong monitoring and evaluation system to be rolled out at the beginning of the project. Opportunities to integrate this into the existing Health Management Information System (HMIS) are being explored.
Engagement of and creating awareness among decision-makers on the magnitude and seriousness of malnutrition among older people has been crucial to the success of the programme. In Adami Tulu Jido Kombolcha woreda a decision was taken by the woreda administration and health office to use the available resources and admit SAM cases for medical treatment, even though this was not specifically budgeted for.
It has also been observed that CMAM is well integrated and resourced within government systems in Ethiopia. The increase in caseload that would result from prioritising older people as a vulnerable group in nutrition emergencies could be absorbed at community-level (assuming food supplies are available); however resources may be lacking to treat SAM cases with medical complications (diabetes, high blood pressure and cardiovascular disease are common underlying conditions) due to the lack of availability of therapeutic supplies. Discussion with the Ministry of Health (MoH), ENCU and UNICEF is underway to make the required resources available.
Recommendations
Older people should be prioritised for support in all humanitarian nutrition interventions, given their vulnerability to malnutrition, their important role in the community and on the basis of humanitarian principles.
Advocacy and capacity-building work is needed among local and international humanitarian agencies to work towards the inclusion of older people in routine screening for acute malnutrition and treatment programmes for acute malnutrition, and to encourage the use of age and gender-disaggregated data to improve monitoring for this age group.
National guidelines on the management of acute malnutrition in Ethiopia must be revised urgently to ensure that older people are included in all aspects from assessment to service delivery. HelpAge has developed a guideline on emergency nutrition interventions for older people, which can be easily adapted to the local context of Ethiopia.
Nutritional guidelines for food distribution suitable for older people must be integrated into all health planning and response plans.
Health management information system (HMIS) data should be disaggregated by age and sex and key indicators for older people included. Alongside this, HelpAge will develop strong monitoring and evaluation systems to enhance learning and improve performance of future projects.
The needs of older people should be routinely included in all four components of CMAM protocols and programmes in Ethiopia, including community mobilisation, supplementary feeding programme, outpatient therapeutic programme and stabilisation centre. Discussions with the MoH and ENCU have already begun to this effect.
Within the health care system, conditions and needs common to older people should be integrated into patient triage, clinical evaluation, treatment, the emergency medical response system and specialty care for SAM cases. Resources must be mobilised to support the inpatient treatment of older people with SAM with medical complications. Greater investment is needed by donors to achieve this.
For more information, contact Kidist Negash.
Endnotes
1The woreda is the third tier of administrative division of Ethiopia. Woredas are further subdivided into kebeles or wards.
2Belg is one of two rainy seasons per year (the shorter season between February and April), followed by the main meher rainy season from May to September.
3An annual species of lovegrass native to Ethiopia and Eritrea raised for its edible seeds and a staple ingredient of the Ethiopian diet.
4The Government’s National Disaster Risk Management Coordination Commission (NDRMCC) and the UNICEF-supported Emergency Nutrition Coordination Unit (ENCU).
References
Borrel 2001, Addressing the nutritional needs of older people in emergency situations in Africa: Ideas for action. HelpAge International, Africa Regional Development Centre, Nairobi.
CSA 2012. 2007 population and housing census of Ethiopia. Central Statistical Authority, April 2012, Addis Ababa.
HelpAge 2011. Nutrition interventions for older people in emergencies: HelpAge Guidelines. Available from: file:///C:/Users/Chloe/Downloads/GuidelineNutrition.pdf
HelpAge 2013. The state of health and ageing in Ethiopia: A survey of health needs and challenges of service provisions. HelpAge International Ethiopia, Addis Ababa.
HelpAge 2013a. Nutrition interventions for older people in emergencies.
HelpAge and EEPNA (2013) Vulnerability of older people in Ethiopia: The case of Oromia, Amhara and SNNP Regional States. HelpAge International Ethiopia, Addis Ababa.


