Experiences of implementing CMAM in Yemen and number of deaths averted
By Najwa Al-Dheeb, Anna Ziolkovska and Stanley Chitekwe
Najwa Al-Dheeb is the Health and Nutrition Specialist for UNICEF Yemen and the central zone Nutrition Cluster Coordinator. Najwa holds two Masters degrees in Public Health and Community Medicine. She has over 13 years’ experience in the public sector and nutrition in both emergency and development contexts. She has worked on projects in Yemen, Nepal, Nigeria, Kenya, UK and United Arab Emirates (UAE).
Anna Ziolkovska is the Nutrition Cluster Coordinator in Yemen. Anna has a PhD and over ten years’ experience in nutrition, humanitarian assistance, cluster coordination, information management, capacity-building and project management at HQ and country level, including in South Sudan, Somalia, Philippines, Ukraine, Afghanistan and Yemen.
Stanley Chitekwe is the Chief of Nutrition for UNICEF Nepal, providing support in the writing of this article. He has worked with UNICEF in Africa and now south Asia for more than 18 years. He has a special interest in the prevention and treatment of acute malnutrition, micronutrient deficiency and stunting and is a mentor to many nutrition professionals.
Location: Yemen
What we know: Yemen is home to one of the worst protracted humanitarian crises globally.
What this article adds: The estimated prevalence of acute malnutrition in Yemen has risen during the current conflict. Community-based management of acute malnutrition (CMAM) programming, introduced in 2009, has evolved to meet increased caseload and now includes mobile teams, integration with vaccination and community health worker services, and increased geographical coverage. Progress is reflected in significant improvement in cure rates, defaulter rates and estimated number of deaths averted (over 221,669 deaths of children under five years old were averted between 2012 and 2017). Management of acute malnutrition (MAM) treatment scale-up has not kept pace with severe acute malnutrition (SAM) treatment (48% versus 72% geographical coverage). Further quality improvements and coverage are hampered by low funding for CMAM in 2016-2017, import restrictions on supplies, limited access, limited numbers of community health volunteers (CHVs) and unpaid health worker salaries. Critical actions being taken to scale-up quality CMAM programmes further focus on outreach; greater scale-up of MAM treatment; securing urgent funding to support life-saving treatment services, especially in high-risk districts; and livelihood interventions to help alleviate food insecurity.
Background
Yemen is one of the poorest countries in the world, ranked 168 out of 188 (2016) on the United Nations Development Programme (UNDP) Human Development Index (UNDP, 2016) with a poverty rate in 2017 of over 62% (World Bank, 2017). Yemen has suffered from internal conflicts and clashes for several years, resulting in severe disruptions of services, lack of security for the population and 3.2 million internally displaced people (IDPs) (YHNO, 2018). One of the worst protracted humanitarian crises globally, the country now faces unprecedented displacement, a sharp rise in the price of basic commodities, food insecurity, high levels of unemployment, poverty and malnutrition, outbreaks of communicable diseases (particularly water-borne diseases) and risk of famine. An estimated 22.2 million people (76% of the population) are now in need of humanitarian or protection assistance, including 11.3 million who are in acute need (YHNO, 2018). More than 274 health facilities have been destroyed or damaged due to air strikes or ground fighting and only half of all health facilities are functioning; even these face severe shortages in medicines, equipment and staff, with non-payment of salaries being a common problem (YHNO, 2018).

The situation in the country is greatly affected by the huge deterioration in the economy. Gross domestic product (GDP) fell by 41.8% between 2015 and 2017 and continues to decline, while the Yemeni Riyal (YR) has devalued at an alarming rate (from YR215 to the US dollar in 2015 to YR500 to the US dollar in 2017)1. Prices of fuel and basic commodities continue to rise as the purchasing power of Yemeni families falls and livelihood opportunities continue to diminish or disappear, further limiting people’s access to healthcare and food. As a result, millions of people are now unable to meet their basic needs independently; recent estimates are that 17.8 million people (60% of the population) are food-insecure and 8.4 million (29% of the population) are severely food-insecure and at risk of starvation. These factors combined are bringing the country ever closer to famine: a total of 107 out of 333 districts are now facing heightened risk of famine, an increase of 13% since April 2017 (YHNO, 2018).
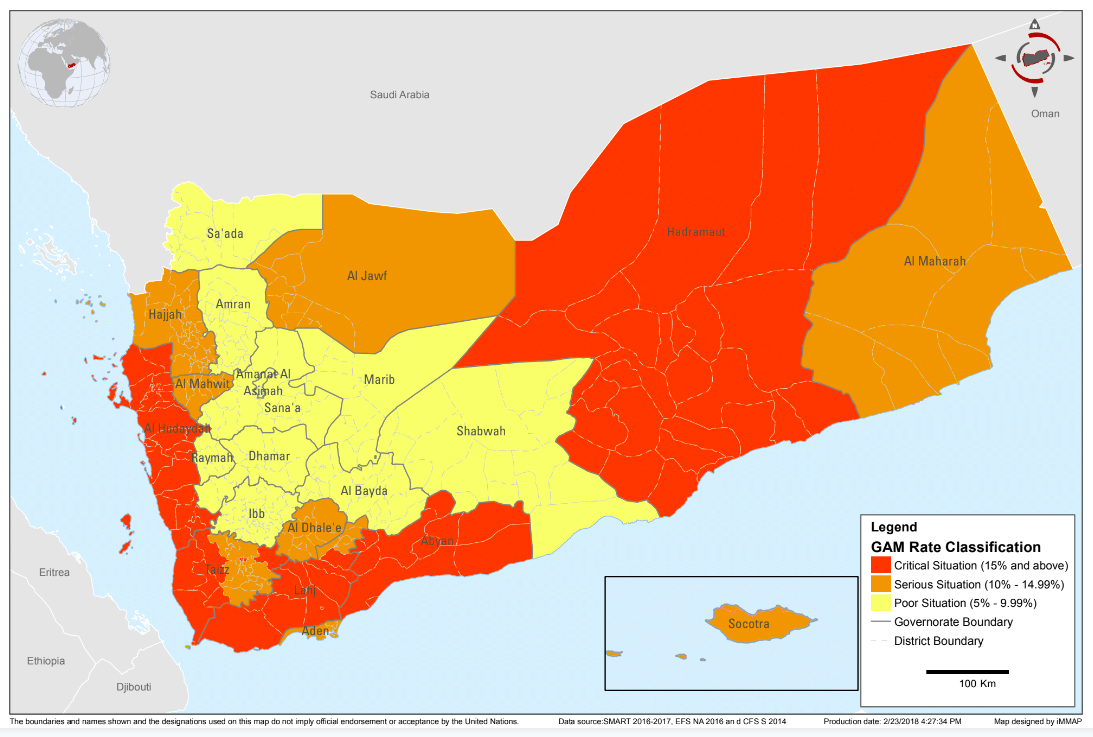
Yemen has historically had one of the highest rates of chronic malnutrition in the world; close to 60% of children were stunted in 20032, which had reduced to 41% in 2013 before conflict broke out3. Recent estimates are that 1.8 million children under five years old (15%) and 1.1 million pregnant or lactating women (PLW) are now acutely malnourished, including approximately 400,000 children under five years old who are suffering from severe acute malnutrition (SAM) (YHNO 2018). Global acute malnutrition (GAM) rates are as high as 27-31% in some locations (YHNO, 2018). The severity of GAM according to district is shown in Figure 1.
Figure 1: Yemen Nutrition Cluster GAM rate classification, February 2018
This article shares the experiences of managing acute malnutrition in the Yemeni context, including the many challenges but also progress made in spite of a hugely difficult operational environment and escalating needs.
Approaches used in Yemen to manage acute malnutrition
In response to the prevalence of SAM in Yemen the first SAM management protocol was developed in 2005. The Government of Yemen and partners subsequently initiated emergency nutrition interventions in 2009, including community-based management of acute malnutrition (CMAM). The nutrition-cluster approach was adopted and initiated in Yemen in August 2009. The steady increase in the acute malnutrition caseload necessitated the development of an interim CMAM guideline in 2013 (based on the 2005 guideline), which was revised in 20174, including training modules and a community-outreach strategy to increase coverage.
The CMAM programme is implemented through fixed health facilities, mobile teams (MTs) and integrated immunisation campaigns, outreach5 and community health volunteers (CHVs) (see Figure 2). The programme was initially implemented through fixed health facilities only; however, only 60% of the population had access to health services, a situation which deteriorated further as a result of the conflict; by 2018 only 50% of health facilities were functional (YHNO, 2018). The Government and partners broadened the implementation modalities to improve access and coverage; for example, by integrating the nutrition component into vaccination campaigns and using MTs to reach remote areas with no existing fixed health institutions, conflict-affected areas where services have been obstructed, and displacement areas. This was guided by a 2015 Ministry of Health (MoH) technical and financial plan to aid implementation and standardise partner efforts. The Government has also invested in growth monitoring of children under five years of age and the promotion of appropriate infant and young child feeding (IYCF) practices. The number of IYCF ‘corners’ located in health facilities increased from 17 in 2012 to 826 in 2017 as a result (although this still falls far short of needs and is not currently growing in line with CMAM expansion). IYCF awareness-raising is included in the MTs through health workers and/or CHVs.
Figure 2: CMAM implementation modality and information flow in Yemen
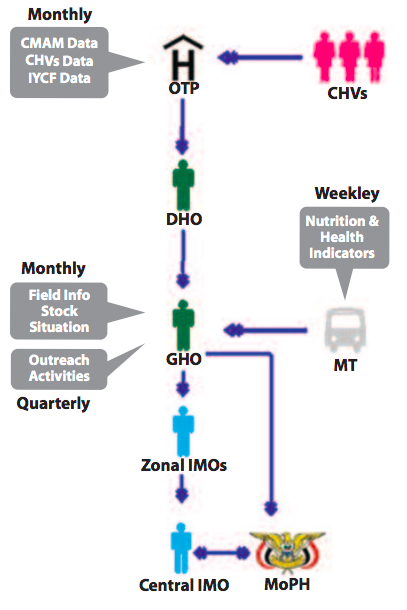
CHVs: community health volunteers; OTP: outpatient therapeutic programme; CMAM: community-based management of acute malnutrition; IYCF: infant and young child feeding; MT: mobile team; DHO: District Health Office; GHO: Governorate Health Office; IMOs: information management officers; MoPH: Ministry of Public Health.
Scaling up CMAM in Yemen
To track CMAM scale-up and improve quality and standardisation of data collected, the Government and partners developed a unified reporting tool and mechanism in 2013-2014, which has since been revised on a yearly basis to accommodate latest information needs. Data flows from community level via CHV reports to each health facility outpatient therapeutic programme (OTP), to the district-level health office then to governorate-level health office and finally to the Ministry of Public Health and Population (MoPHP), as shown in Figure 2.
While the majority of interventions were originally implemented through the MoPHP, the presence of humanitarian agencies implementing CMAM has doubled since 2013 to 34 partners. There is now an increased interest by the international community in funding CMAM programmes in Yemen and since the risk of famine was declared in 2017, additional resources have been mobilised. A number of ‘traditional’ donors such as the United States Agency for International Development (USAID), European Civil Protection and Humanitarian Aid Operations (ECHO) and the UK Department for International Development (DFID) provided funding to both United Nations (UN) agencies and non-governmental organisations (NGOs), while pooled funding (Yemen Humanitarian Pooled Funds and the Central Emergency Response Fund (CERF)) managed by the United Nations Office for the Coordination of Humanitarian Affairs (UNOCHA) is used to fund priority locations and projects with funding gaps. In 2017 the World Bank also began funding projects in Yemen that directly and indirectly support the scaling-up of the CMAM programmes. This resulted in US$127.1 million (69.7% of requirements) received for Nutrition Cluster interventions in 2017, compared to US$39.8 million (56.4% of requirements) in 2014 before the escalation of the conflict. Some of these funds have been used to build the capacity of the MoPHP to monitor and evaluate CMAM programmes and carry out joint CMAM missions between the MoPHP, NGOs and UN agencies.
Standard CMAM training packages were developed for health workers and CHVs by the MoPHP with technical and financial support from UNICEF. The training was rolled out across the country by a pool of MoPHP-qualified trainers to both government and NGO workers. Over 10,000 health workers have been trained on the CMAM package to date; training has been delivered on the provision of nutrition services as part of the primary healthcare package in OTPs and the integration of nutrition services into MTs and vaccination outreach. In addition, to increase CMAM coverage, over 16,500 CHVs have been trained in community sensitisation and the provision of basic services, including awareness-raising, screening, referral and follow-up of acutely malnourished children and PLWs.
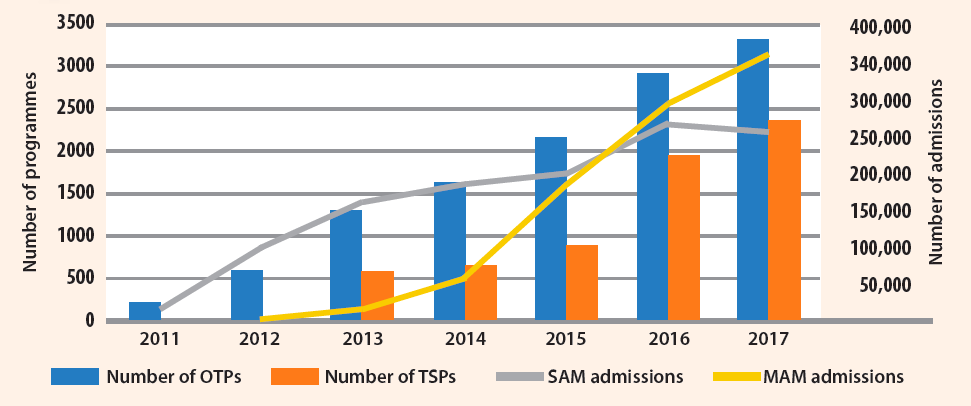
The programme has scaled up steadily since 2011, as shown in Figure 3. In 2017, 330 (11% more than in 2016) additional OTPs and 436 (22% more than in 2016) additional therapeutic supplementary feeding programmes (TSFPs) were established. Over half a million children were admitted to the CMAM programme in 2017, which is one quarter of the projected caseload. However, in spite of the geographical scale-up (72% and 48% for OTPs and TSFPs respectively), the number of admissions remained similar in 2017 compared to 2016 for both SAM and MAM treatment programmes (as per the data currently available in the Nutrition Cluster). In addition, TSFP scale-up did not match OTP scale-up, which explains the low admission rate of MAM cases from 2009 to 2016, even though MAM caseload is four to five times the SAM caseload (as shown in Figure 3).
There are several contributing factors to this: first, not all reports for CMAM treatment have yet been received (there are still 117 reports missing from OTPs and 30 reports missing from TSFPs from MoPHP); these are expected to significantly increase the number of new admissions to CMAM programmes. Second, outreach services in Yemen remain weak, with less than 25% of needed CHVs currently in place and a limited number of mobile teams. Third, health workers have not received salaries for more than two years and there are competing priorities in the health system, such as the cholera outbreak, which impacted CMAM programme implementation. Fourth, the deteriorated economic situation has severely affected the population’s ability to seek services, including those for malnutrition treatment. The integration of MUAC screening into the polio campaign in October 2017 increased active case findings; over 65,500 and 227,000 children under five years old were found to be severely acutely malnourished and moderately acutely malnourished respectively.
Figure 3: Progress of CMAM scale-up
Performance of the CMAM programme in Yemen
Many quality issues remain in the CMAM programme in Yemen and some standards fall below SPHERE indicators, although there has been encouraging improvement in programming quality over the last few years.
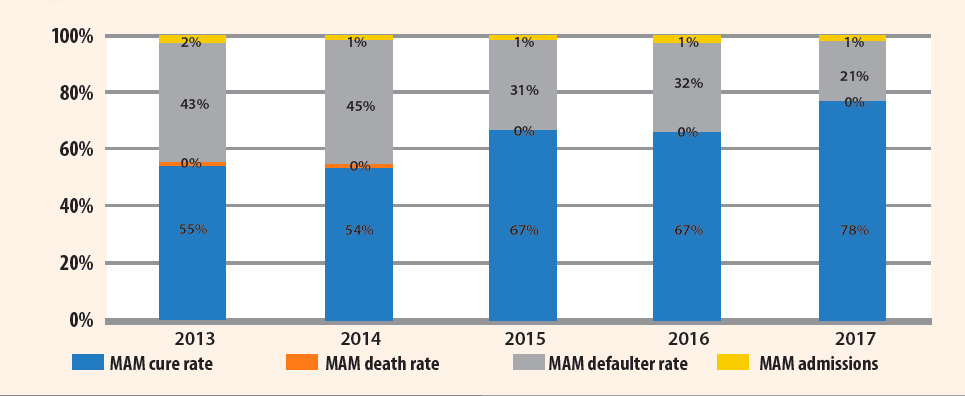
SAM cure rates increased significantly from 64% in 2013 to 77% in 2017 and the numbers of defaulters and deaths among children also reduced (Figure 4). Similarly, for MAM treatment, cure rates increased from 55% to 78% in the districts where the programmes were implemented, also due to decreased number of defaulters, which correlates with less stockouts of supplies (Figure 5).
Figure 4. SAM performance indicators (2013-2017)
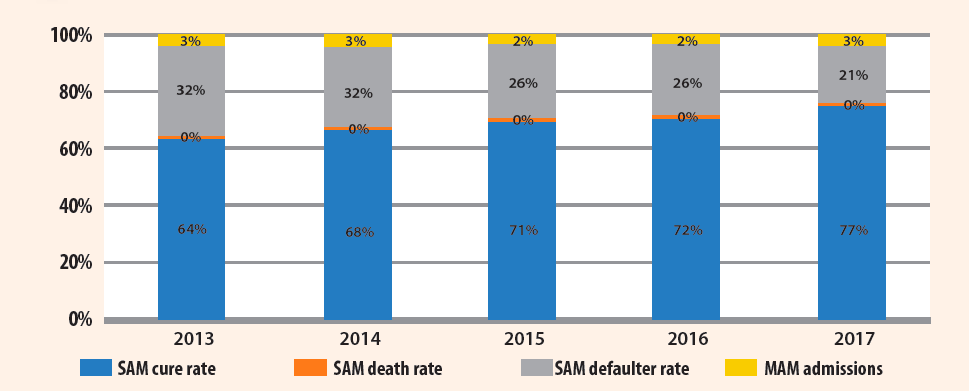
Figure 5. MAM performance indicators (2013-2017)
Despite this progress, the programme faces many bottlenecks. While there have been significant increases in funding (described above), funding remains below necessary levels (the CMAM programme was only 69.7% funded in 2017), especially for the MAM and PLW acute malnutrition treatment component. Another constraint is the restrictions on commercial and humanitarian imports and distribution, which has led to general reduction in food availability in the country, thus leading to increased food insecurity and increased caseloads for CMAM programmes. Furthermore, access, movement and activities in certain governorates/districts are restricted due to the escalation in the conflict, cumbersome bureaucratic impediments and complex clearance mechanisms. The capacity of NGOs in Yemen also remains low; one of the main contributing factors to this is the difficulty of obtaining visas and bringing international humanitarian personnel into the country to complement and build national capacity. Limited numbers of CHVs and cessation of health workers’ income create additional pressures, as previously mentioned.
Deaths averted by the CMAM programme in Yemen
SAM carries a high risk of death and requires therapeutic treatment for recovery, which highlights the importance of CMAM scale-up. To estimate deaths averted by the CMAM programme in Yemen, the same equation as used in a CMAM programme in Nigeria (Bulti et al, 2015) was applied, as recommended by the Global Nutrition Cluster (GNC) to estimate the number of lives saved in one year for use in advocacy. In this equation, DA= EM* PC* NT (where DA is the estimated number of deaths averted by the CMAM programme; EM is the expected excess mortality in untreated SAM cases with similar severity of wasting to those treated by the programme; PC is the proportion of SAM cases cured by the programme and NT is the number of SAM cases treated by the programme). Yemen’s cure rate, caseload and under-five mortality for the last six years were used and, similar to the Nigerian study, an estimate of mortality associated with MUAC was used, based on published data on mortality associated with MUAC in untreated SAM cases (Briend and Zimicki, 1986; Briend et al, 1987 and Vella et al, 1994). Using these calculations, in 2017 alone 260,000 children under five years old were admitted to the SAM programme (OTPs), over 50,000 of whom were saved from death, which is around 20% of cases admitted. Over the last six years, during which time around 1.2 million children under five years old were admitted to OTPs, it is estimated that over 221,600,000 children were saved from death, which is around 19% of the cases admitted. These calculations serve to emphasise the impact of the programme on deaths averted; the limitations addressed in the original study apply here also. While this is a good achievement, quality CMAM scale-up in Yemen with increased focus on equity to reduce defaulters and increase access would save many more children’s lives in the country.
Future recommendations for CMAM programming in Yemen
In light of progress made in the treatment of acute malnutrition, challenges experienced and lessons learned, several key actions are needed in Yemen to improve CMAM programming.
Further scale-up of quality CMAM programmes is necessary, focusing on community outreach-supported activities to improve access and utilisation. CMAM components must be scaled up in parallel to cover SAM, SAM with complication and MAM children; slow scale-up of MAM services for children is an important bottleneck. An urgent appeal should be issued to all major humanitarian donors to fund CMAM as a critical life-saving activity, especially in districts at high risk of sliding into famine. Continuous advocacy for secure humanitarian access and facilitation of importation and distribution of goods is also critical.
Plans for 2018 aim to address some of the constraints mentioned in this article. Cluster’s geographical coverage of CMAM will be increased to 85% of functional health facilities (for SAM treatment throughout the country and for MAM treatment in priority districts), including scaling up MTs from 113 to 200. This also includes scaling up current TFCs in the country from 49 to 85 during 2018, based on a detailed scale-up plan. To avoid duplication and fill gaps, all new programmes are now mandatorily coordinated with the DHOs and GHOs and are open in those areas most in need, based on the results of micro-assessments and knowledge of the situation. An additional 15,000 CHVs will be trained and supervised to support scale-up, and several capacity-building activities will take place among different cadres through the MoPHP for sustainability of nutrition efforts in the field.
In 2018 the MoPHP, with UNICEF support as the Nutrition Cluster lead, aims to improve the quality of monitoring and supervision visits by the GHOs and DHOs by ensuring that each monitoring visit provides an opportunity to increase programme quality through the provision of immediate mentoring to overcome identified problems. An online system for CMAM reporting is also being finalised to improve the quality of reports submitted and availability of information for all partners.
Additionally UNICEF, World Health Organization (WHO) and UNDP projects, funded by the World Bank, aim to support the functioning of health facilities. This will indirectly contribute to better coverage of CMAM services and support CMAM scale-up.
IYCF activities, an important prevention component of CMAM programmes, while also scaled up year by year, remain below necessary levels. In response the Nutrition Cluster is planning to develop guidance on ‘IYCF corners’ to make them standard within all services and to more than double the number of CHVs trained in IYCF to provide health education in communities.
A bottleneck analysis is planned for CMAM programmes in Yemen in 2018 to identify key bottlenecks and to develop a plan on addressing them to improve CMAM programming further.
Addressing the immediate and underlying causes of acute malnutrition is also necessary in order to decrease the CMAM caseload in the country. The Nutrition; Water, sanitation and hygiene (WASH); Health; Food Security; and Agriculture Clusters are now working together to develop and pilot an integrated famine-risk reduction approach in Yemen.
For more information, please contact Najwa Al Dheeb.
Endnotes
1Socioeconomic update, Ministry of Planning and International Cooperation, issue 30, December 2017.
2Yemen Family Health Survey, 2003.
3Yemen Demographic Health Survey, 2013.
4CMAM interim guideline, 2013.
5Yemen Health System Profile. WHO, 2006.
References
Briend A, Zimicki S, Validation of arm circumference as an indicator of risk of death in one to four-year-old children, Nutr Res, 1986;6:249-261
Briend A, Wojtyniak B, Rowland MGM, Arm circumference and other factors in children at high risk of death in rural Bangladesh, Lancet, 1987;26:725-727
Bulti A, Chitekwe S, Puett C and Myatt M. (2015). How many lives do our CMAM programmes save? A sampling-based approach to estimating the number of deaths averted by the Nigerian CMAM programme. Field Exchange 50, August 2015. p38. www.ennonline.net/fex/50/deathsavertedcmamnigeria
Vella V, Tomkins A, Ndiku J, Marshal T, Cortinovis I, Anthropometry as a predictor for mortality among Ugandan children allowing for socio-economic status, Eur J Clin Nutr, 1994;48:189–197
UNDP (2016) Human Development Index. Available from: http://hdr.undp.org/en/content/human-development-index-hdi
World Bank (2017) Toward a blueprint for the recovery and reconstruction of Yemen.
YHNO (2018). Yemen Humanitarian needs overview, 2018. Available from: www.unocha.org/yemen


