Effectiveness of a community-based infant and young child feeding support group programme among ethnic minorities in Vietnam
By Md Masud Rana, Huan Nguyen Van and Thach Nguyen Ngoc
Md Masud Rana is a Nutrition Advisor with Save the Children with a particular focus on supporting nutrition programmes in Asia region. Masud has worked for more than ten years in the design, delivery and evaluation of nutrition, food security and livelihoods programmes in Asia and Africa.
Huan Nguyen Van is the Health and Nutrition Program Development Manager with Save the Children International in Vietnam. He has an MSc in Project Management and nearly 10 years’ experience in health and nutrition development projects.
Thach Nguyen Ngoc is a Public Health Specialist with a BA in Public Health from Hanoi School of Public Health, Vietnam. He currently works with Save the Children International in Vietnam as the Health and Nutrition Coordinator of Northern Mountain Integrated Child Nutrition Improvement Project, Vietnam.
The authors acknowledge support from local partners, including Thanh Hoa Department of Health, Thanh Hoa Reproductive Health Centre, Thuong Xuan District Health Centre and four Commune Health Centres (Xuan Loc, Xuan Chinh, Ngoc Phung and Van Xuan) in Thuong Xuan district, Thanh Hoa province, for their support. Special gratitude is offered to mothers and children from Thuong Xuan district, Thanh Hoa province for volunteering to take part in the study, sharing their knowledge on local child-feeding practices and sparing their valuable time. The authors would also like to acknowledge Irish Aid’s contribution and their generous support in funding the project and this study, and the support of Save the Children staff in Vietnam.
Location: Vietnam
What we know: A quarter of children under five years old are stunted in Vietnam; prevalence is higher amongst ethnic minority groups.
What this article adds: Community-based infant and young child feeding (IYCF) support groups were established in a remote northern region of Vietnam from 2012 to 2017 to provide breastfeeding support, complementary feeding support and IYCF information to community members. An impact evaluation was carried out in July 2017 using propensity score matching to compare changes in IYCF knowledge and practices and prevalence of stunting in children under two years old between a group that received the intervention (149 households) versus a control group (227 households) from 37 villages. Findings showed some impact on IYCF knowledge (among mothers and caregivers on breastfeeding and complementary feeding practices), but limited impact on practice (significant impact only for minimum dietary diversity and handwashing) and no impact on stunting or acute malnutrition. In future, the authors propose that similar interventions should be informed by barrier analysis; care groups should be delivered at greater intensity; and multiple channels should be used to delivery social and behaviour change communication interventions (including antenatal clinics and health facilities).
Background
Despite significant reductions in child malnutrition over the past two decades, a quarter of all children under five years old in Vietnam are stunted. Prevalence is higher among ethnic minority children in the northern mountainous region, where it ranges from 41 to 55%. Research suggests inappropriate infant and young child feeding (IYCF) practices are the key determinants of stunting in Vietnam (Chaparro, Oot & Sethuraman, 2014). As these communities live in remote areas and have limited access to health facilities, Save the Children International in Vietnam (SCiV) and Alive & Thrive jointly designed a community-based IYCF support group intervention as an alternative model using social behaviour change communication (SBCC). SCiV, with funding from Irish Aid, implemented a project based on this design in Thuong Xuan District, Than Hoa province in Northern Vietnam between 2012 and 2016. The project was later extended for one more year and aligned more closely with the Government of Vietnam’s poverty alleviation programme for ethnic minorities.
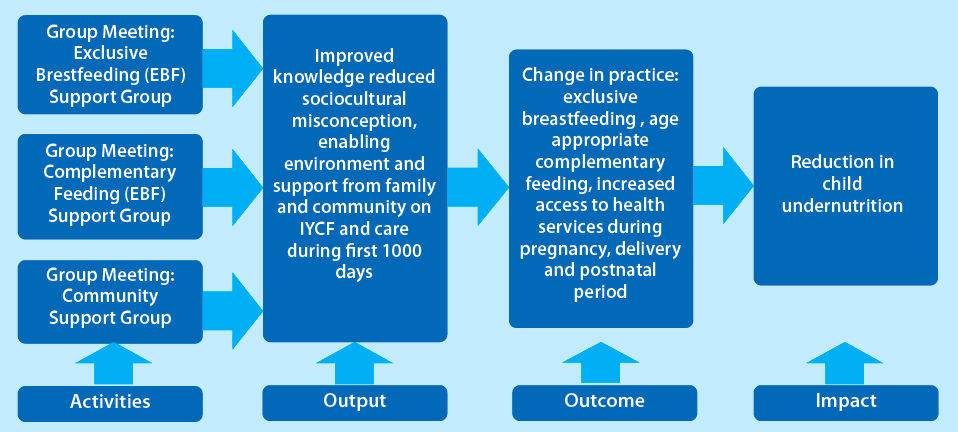
The IYCF support group model (described in Figure 1) is based on three types of support groups facilitated by trained staff, including a monthly breastfeeding group for pregnant women and mothers with infants aged 0-6 months; a monthly complementary feeding group for mothers and caregivers of children aged 6-24 months; and a community support group for fathers, grandparents and village leaders. Information about appropriate IYCF practices and to address IYCF misconceptions was delivered through the groups. The purpose of this research was to evaluate the impact of the IYCF support group in improving child-feeding practices and reducing stunting among children under two years old. Based on the theory of change (Figure 1), the study sought to determine whether the intervention significantly changed IYCF practices among the target population and identify the effect of the intervention on stunting among children under two years of age.
Figure 1: Simplified theory of change for the community-based IYCF support group model
Methods
A quasi-experimental impact evaluation was undertaken in July 2017 to compare individuals and households with children under two years old who received the intervention (i.e. those from villages where IYCF support groups were formed and maintained) with those from neighbouring communities with similar background characteristics who did not receive the intervention. Probability-proportionate-to-size (PPS) sampling was used to select both the intervention and control group. A total of 376 households (149 intervention households and 227 comparison households) was surveyed from 37 villages in five communes.
The primary analysis approach for this effectiveness review was propensity score matching (PSM). The matching variables were selected based on two key factors: (i) the variables considered to be most important in influencing ‘project participation’; and (ii) the variables with the potential to affect both the intervention outcome and the likelihood of project participation (Caliendo & Kopeinig, 2008). Robustness was tested by estimating outcomes using alternative PSM models and multivariate regression models. More details of the data analysis process and methodological limitations can be found in the full report (Rana, Nguyen Van & Nguyen Ngoc, 2017).
Key findings
In the overall sample, 91% of households were male-headed and in 57% of households the primary occupation was farming. One in every five household heads (19%) had no formal education; around 11% had completed primary school; 58% had attained a secondary-level qualification; and one in every 20 household heads was educated beyond this level. Based on the government poverty measurement system, over one third (36%) of households were categorised as ‘poor’ (total income < one million VND/person/month). Around 90% of the intervention and 87% of the comparison mothers gave birth in a health facility during the delivery of their last child. One quarter of all child births were through caesarean section (which reflects national C-section figures) and almost all pregnant women reported visiting the health facility for antenatal care (ANC) services.
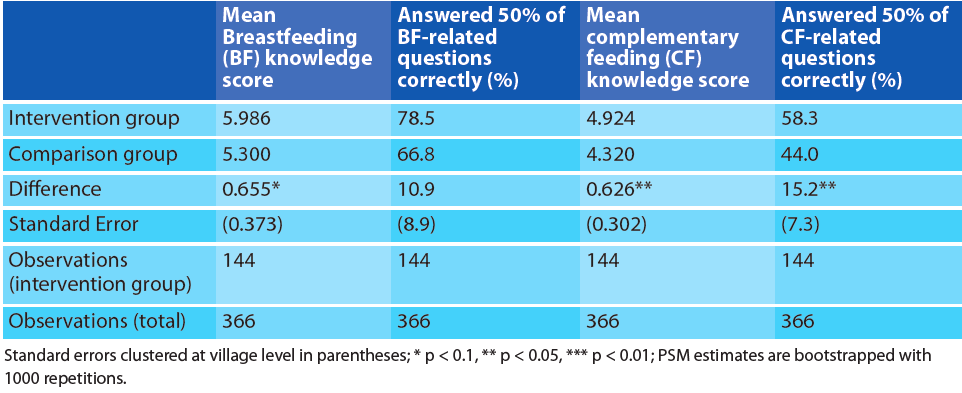
Caregiver’s knowledge on IYCF
A set of ten questions was developed to assess mothers’ knowledge on breastfeeding (BF) and complementary feeding (CF), which were combined to create a BF knowledge score and a CF knowledge score. As indicated in Table 1, on average mothers from intervention villages scored 6.0 out of 10 on the breastfeeding knowledge scale, compared to an average score of 5.3 among the comparison group. Statistical evidence supporting this difference is weak in the primary analytical model. However, considering the fact that the robustness tests (with alternate models) suggest very strong significance, the project is likely to have had a positive impact on knowledge of breastfeeding (please contact the authors to see the full report).
On average mothers from the intervention villages scored an average of 4.9 out of 10 on the complementary feeding knowledge scale, compared to an average score of 4.3 among the comparison group; this difference was statistically significant (p<0.05).
Table 1: Knowledge of caregivers (mothers) from intervention and comparison households on appropriate IYCF
Nutrition practices
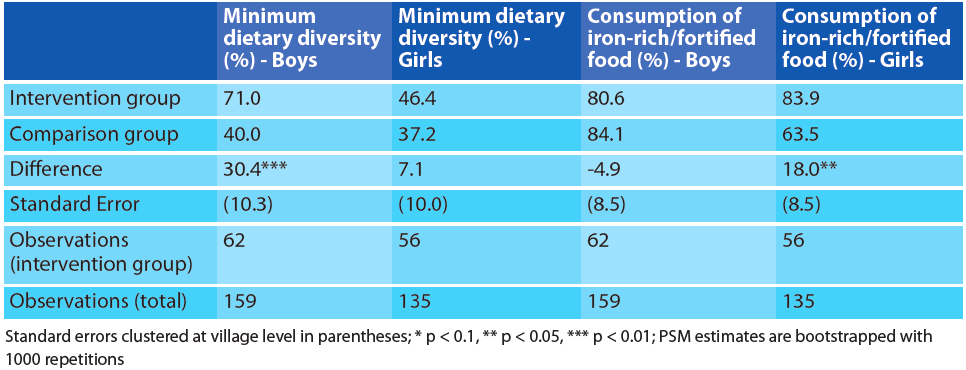
Nutrition practices were measured according to WHO-IYCF core indicators (see Figure 2). A statistically significant (p<0.05) positive impact of the intervention was found only on minimum dietary diversity (MDD). On average, 59% of intervention group mothers reported that their child had received food from a minimum of four food groups during the 24 hours preceding the survey, compared to only 39% among the comparison group. This finding is likely to be primarily due to the significant variation in MDD between boys in the intervention (71% and 40% in intervention and control groups respectively), while for girls the difference (46% and 37%) was not found to be statistically significant.
However, the percentage of children receiving a minimum acceptable diet (MAD) was actually higher among comparison group (17%) compared to the intervention group (13%), although the difference was not statistically significant. The evaluation did not find any evidence of impact on the early initiation of breastfeeding and no significant impact on exclusive breastfeeding (24 hour recall). There was strong evidence that the intervention had a positive impact on girls’ consumption of iron-rich or iron-fortified foods, although the overall impact across both genders was not statistically significant (Table 2).
Figure 2: IYCF practices in intervention and comparison households
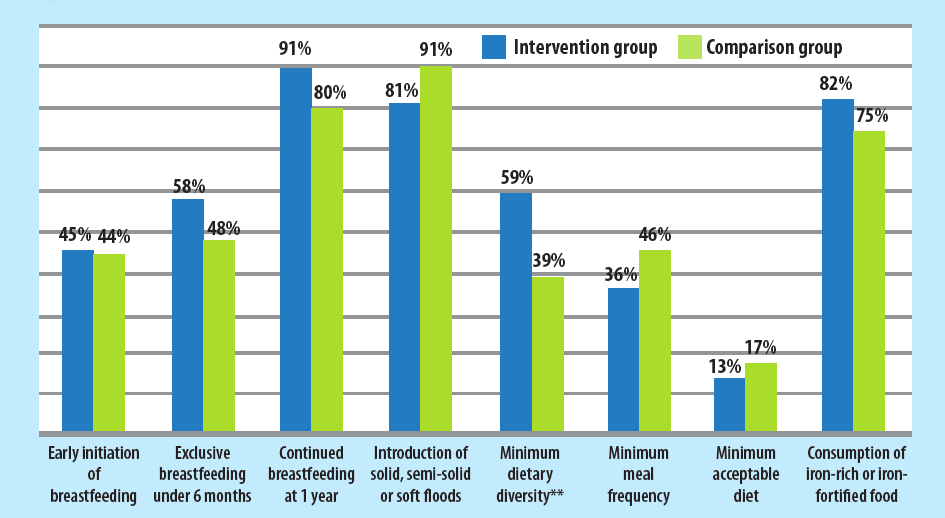
* p < 0.1, ** p < 0.05, *** p < 0.01
Table 2: Minimum dietary diversity and consumption of iron-rich/fortified food in intervention and comparison households, disaggregated by sex
Handwashing
As messages relating to personal hygiene and appropriate hand-washing practices were an integral part of the SBCC module, the effect of the intervention on these practices was also evaluated. Results show that the intervention had a statistically significant positive impact on reported hand-washing practices. Overall, 38% of mothers from intervention villages reported washing their hands at all five critical times with water and soap, compared to 26% from the comparison group (P<0.1) (Figure 3).
Figure 3: Reported hand-washing practices by caregivers from intervention and comparison groups
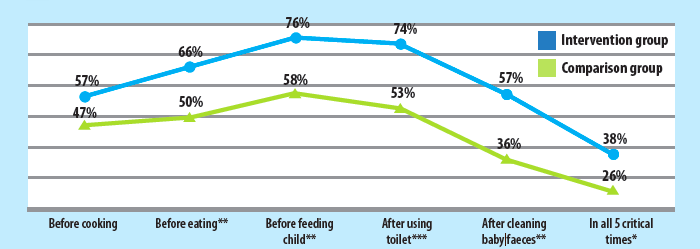
* p < 0.1, ** p < 0.05, *** p < 0.01
Child nutritional status
Anthropometry was used to measure child nutritional status. Anthropometric measurements (i.e. sex, height, weight and date of birth) of an index child1 were taken from every participating household. No significant difference between children in intervention and comparison households was found in terms of stunting (14% compared to 15%) or underweight (10% compared to 13%), as measured by height-for-age and weight-for-age z-scores respectively (Figure 4). Wasting was found to be lower among intervention group households; however the proportion of children who were stunted and wasted concurrently was slightly higher in the intervention group (2% compared to 1%).
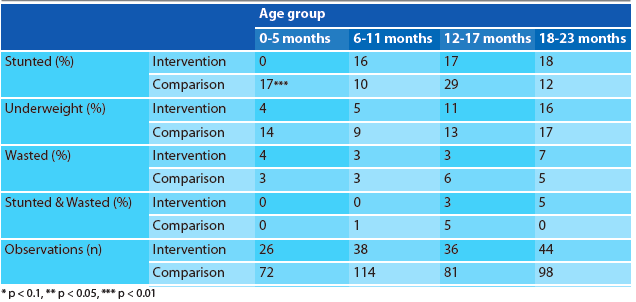
When disaggregated by age group (Table 3), it was observed that the prevalence of malnutrition was higher among older children compared to younger children in both intervention and comparison groups. There was no statistically significant difference between the two groups in terms of any of the types of malnutrition except stunting among children aged 0-5 months; there were no stunted infants in the intervention group, compared to 17% in the comparison group.
Prevalence of severe stunting was similar between the two groups (4%), as was severe underweight (1%) and overweight (1%). Nearly 2% of children in the intervention group children were severely wasted, compared to less than 1% of children in the comparison group.
Figure 4: Mean nutrition status of children < 2 years old from intervention and comparison households
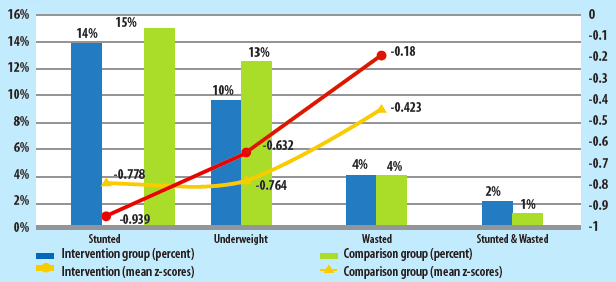
* p < 0.1, ** p < 0.05, *** p < 0.01
Table 3: Nutrition status of children < 2 years old from intervention and comparison households disaggregated by age-groups
Programme learning consideration
Establish multiple channels for information dissemination: Despite increases in knowledge, the change in IYCF practices was minimal. Future programme designs should consider multiple contact points for information sharing in addition to regular group meetings and group counselling. Nutrition counselling could also be delivered during ANC check-ups, given the good availability and access of ANC at commune and district levels. Individual counselling could also be provided through home visits, depending on the context and resource availability.
Design the intervention based on analysis of existing barriers to behaviour change: The messages and intervention activities should address not only knowledge but context-specific barriers to adopting recommended behaviours, which should be determined through barrier analysis. The findings of this analysis should be used to develop a project-specific behaviour change framework.
Improve efficiency of programme implementation: Improvement in IYCF practice was found only for MDD among boys, consumption of iron-rich or iron-fortified food among girls, and caregiver handwashing at critical times. There was no evidence that the intervention positively affected child nutrition status. While there could be many different factors contributing to the lack of positive impact, efficiency of programme implementation is likely an important one. During 2017, only 45.5% of intended group meetings took place (518 out of a target of 1,140 meetings across 38 villages, with 30 meetings/village). To address this, frontline staff must strictly adhere to the implementation plan, which stipulates monthly group meetings on BF and CF and bi-monthly community group meetings.
Future projects should work closely with the Department of Health, Provincial and District People’s Committees, the central and local level Women’s Union and other government agencies to ensure the adherence to the implementation plan.
Conduct a gender-context analysis during future programme design phase: This review has found that, even at end-line, there was disparity between boys and girls with regard to some of the outcome-level nutrition practice indicators. This indicates that gender may influence child-feeding decisions. It was beyond the scope of this study to explore this fully, but future interventions and activities should be designed in light of a gender-context analysis.
Conclusions
Review of this project demonstrates the potential but also the progamming and likely social and economic complexities behind delivery of an effective, community-based IYCF support group model. The intervention impacted IYCF knowledge but had limited impact on practice and no impact on stunting or acute malnutrition. Future community-based IYCF support group interventions should be informed by barrier analysis, delivered at the intensity stipulated in the intervention plan, and use multiple channels for the delivery of SBCC activities. Given the high attendance at ANC and facility delivery (with significant C-section rate) in this population, engaging health facility staff in interventions to influence early breastfeeding practices is necessary. The programme should also be complemented by other poverty-reduction and food-security interventions to enable participants to practice recommended behaviours.
For more information, please contact Md Masud Rana.
Endnotes
1 ‘Index Child’ was the youngest child of the household, who was also under 24 months old at the time of the survey.
References
Caliendo M & Kopeinig S. (2008). Some Practical Guidance for the Implementation of Propensity Score Matching. Journal of Economic Surveys, Wiley Blackwell, vol. 22(1), pages 31–72. Retrieved from http://onlinelibrary.wiley.com/doi/10.1111/j.1467-6419.2007.00527.x/epdf
Chaparro C, Oot L & Sethuraman K. (2014). Vietnam Nutrition Profile. Washington, DC: FHI 360/FANTA. Retrieved from www.fantaproject.org/sites/default/files/download/Vietnam-Nutrition-Profile-Apr2014.pdf (Accessed 9 July 2018).
Rana M, Nguyen Van H & Nguyen Ngoc T. (2017). Effectiveness of community-based infant and young child (IYCF) support group model in reducing child undernutrition among ethnic minorities in Vietnam. Hanoi, Vietnam: Save the Children.


