Screening for maternal and child malnutrition using sentinel-based national nutrition surveillance in Afghanistan
By Admire Chinjekure, Dr Mohammad Qasem Shams, Dr Abdul Baseer Qureshi, Dr Shafiqullah Safi and Dr Noor Rahman Noor
Admire Chinjekure is the Technical Officer and Team Leader Nutrition for the World Health Organization (WHO) Afghanistan. He is a nutritionist with an MSc in Public Health from the London School of Hygiene and Tropical Medicine (LSHTM) and has over 12 years’ experience in nutrition, health and monitoring and evaluation in Afghanistan and Zimbabwe.
Dr Mohammed Qasem Shams is the National Professional Officer Nutrition for WHO Afghanistan. He is a medical doctor with a post-graduate diploma in Public Health Nutrition and has over 15 years’ experience in nutrition programming, including setting up routine nutrition surveillance systems in Afghanistan.
Dr Abdul Baseer Qureshi is the Technical Officer Nutrition for WHO Afghanistan. He is a medical doctor with over five years’ experience in nutrition coordination and setting up routine nutrition surveillance systems in Afghanistan, having previously been the National Coordinator for the Afghanistan National Nutrition Surveillance Department.
Dr Shafiqullah Safi is the Focal Point for the Integrated Management of Acute Malnutrition (IMAM) supply and emergency in the Public Nutrition Directorate of the Ministry of Public Health (MoPH) Afghanistan. He is a medical doctor with a post-graduate diploma in nutrition and has over nine years’ experience in public health and nutrition in Afghanistan.
Dr Noor Rahman Noor is National Coordinator for the Afghanistan National Nutrition Surveillance Department in the Public Nutrition Directorate of the MoPH Afghanistan. He is a medical doctor with a post-graduate diploma in nutrition and over five years’ experience in nutrition surveillance and IMAM.
The authors would like to acknowledge WHO and UNICEF as the technical partners for the National Nutrition Surveillance Programme in Afghanistan, funded by Global Affairs Canada. They would also like to acknowledge Dr Homayoun Ludin, the Acting Director of the Public Nutrition Directorate of the MoPH Afghanistan, who provided strategic leadership for the Nutrition Surveillance Programme.
Location: Afghanistan
What we know: Nutrition surveillance is an important strategy for measuring trends in undernutrition to determine nutrition response and to act as an early warning system (EWS).
What this article adds: A health facility-based nutrition surveillance system (sentinel) was developed in Afghanistan by the Ministry of Public Health (MoPH), supported by the World Health Organization and UNICEF to monitor nutrition trends and serve as an EWS. Data are collected from 175 health facility sites and 868 community sentinel sites, selected by convenience from all 34 provinces. Anthropometric, birth outcomes, infant and young child feeding (IYCF) practices and maternal haemoglobin (Hb) data are collected from a random sample of children under two years of age/mothers as they visit health facilities at different levels. Facilities are provided with training, equipment, reporting forms and supportive supervision. Results show an increase in the number of children screened from 2015 to 2017. Acute malnutrition is prevalent among children under two years old, as is maternal malnutrition (30% with low Hb levels). Although largely similar, there was a decreasing trend of GAM and SAM at community compared to health facility sites (2016 to 2017). Lessons learned include the following: it takes time to develop a fully functional nutrition information system (five years in this case); fewer indicators are better to preserve data quality; several IYCF indicators are not feasible to collect in routine services; health facilities should be well connected with community sites to facilitate monitoring; exhaustive monitoring may be preferable to a sample to avoid bias. Steps are being taken to now integrate feasible nutrition indicators into the HMIS system, complemented by the sentinel system for detailed indicator collection.
Background
The national nutrition surveillance system (NNSS) of Afghanistan consists of surveys (national nutrition surveys (NNS); demographic and health surveys (DHS); Afghanistan household surveys (AHS); SMART surveys; and localised surveys) and the Health Management Information System (HMIS). Since 2013, the World Health Organization (WHO) and UNICEF, funded by Global Affairs Canada (GAC), have jointly supported the Ministry of Public Health (MoPH) Public Nutrition Directorate (PND) in establishing a health facility-based nutrition surveillance (sentinel) system, complemented by community-based surveillance data, to address the lack of a nutrition early warning system (EWS) and limited collection of nutrition data by the HMIS. This article shares lessons learned in the development of a nutrition surveillance system in an emergency context where data needs are high due to the dynamic nature of the humanitarian situation and the requirement of near-to-real-time modelling of vulnerability to target interventions to those in most need.
Objectives
The primary objective of the intervention was to monitor nutrition trends in the country to serve as an EWS. Specifically, the system was established to collect information on child anthropometry, infant and young child feeding (IYCF) and maternal nutrition status through the existing health system, to understand the nutrition trends in the country and to provide early warning on any potential malnutrition problems requiring action. Ultimately, the intervention intends to contribute towards mothers and children receiving essential nutrition services that contribute to improvement of nutrition status.

Methods
Coverage of the sentinel nutrition surveillance system
The sentinel site system consists of two levels: (i) health facility sites (n = 175); and (ii) community sentinel sites (n = 868). Sites were selected by convenience in all 34 provinces through participatory involvement of key stakeholders. Accessibility was a key consideration due to insecurity risks, although whenever possible hard-to-reach areas were considered for inclusion. Health facilities in Afghanistan consist (in ascending order) of: health posts (community level), sub-health centres, basic health centres, comprehensive health centers, district hospitals and provincial hospitals. The total number of health facilities in the country is approximately 2,865. There are 15,855 active health posts. Maternity services are provided in all health facilities except health posts; currently 1,454 facilities provide maternity services.
Under the sentinel system, anthropometric data are collected from a random sample of children under two years old as they visit health facilities (basic healthcare, comprehensive, district and provincial facilities). Every third child is selected until a target sample (minimum 150 per quarter per heath facility) is reached, and then assessed against anthropometric indices. For maternal indicators, a random sample of pregnant women visiting the particular health facility for the first time (first ANC contact) in the current pregnancy have blood samples taken and Hb measured; four to five mothers are selected randomly per day. Table 1 describes the nutrition indicators collected in the sample population. Emergency nutrition assessment (ENA) software is used to analyse anthropometric indicators against indices. Data are collected daily until targets are reached, after which they are sent for data entry on a monthly basis. Reporting is conducted quarterly.
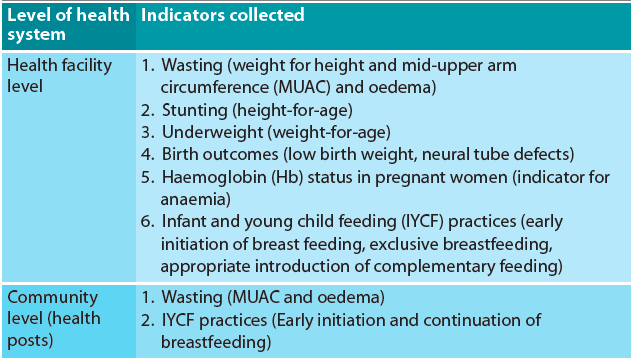
Table 1. Indicators collected through the sentinel nutrition surveillance system
Investment at sentinel sites
Before starting data collection, training on surveillance principles and techniques is conducted for facility personnel. A two-day training detailing the principles of growth assessment, surveillance and reporting is conducted for health workers from each site. Training is more detailed for workers from health facilities as they conduct more in-depth assessments, while community health workers (CHWs) develop more basic skills in measuring mid-upper arm circumference (MUAC) and interpreting results. Health facilities are provided with equipment for conducting the assessments (scales, height boards and hemoCues for Hb measurement) as well as reporting forms while community sites receive MUAC tapes and registers. The reporting forms were developed from existing mother and child health registers, modified to collect additional nutrition surveillance data. Regular support visits and on-the-job mentoring is provided by WHO-recruited field officers and government-recruited nutrition officers. Replenishing of surveillance equipment and registers is initially done through project funds and then gradually taken up by the respective implementers of the health services across the sentinel sites.
Results
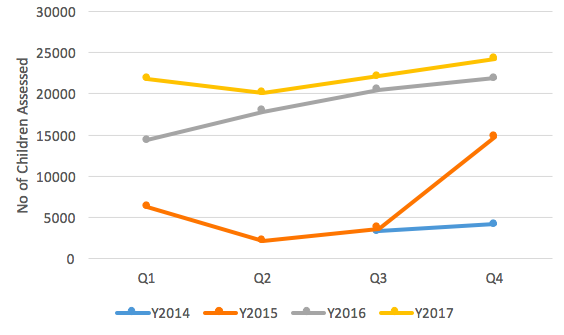
Although there is a need to continually improve the quality of data, the nutrition surveillance intervention has served as an entry point to strengthen growth monitoring and promotion as one of the main preventive strategies, as well as enable early case identification of severe acute malnutrition cases. As shown in Figures 1 and 2, the number of children screened has gradually increased and it is at this screening contact that growth monitoring and promotion services are likely to be provided by the health worker. The growth monitoring and promotion in the health facility sentinel sites are comparatively better than other health facilities not selected as sentinel sites. This is explained by the increased in-service trainings at sentinel sites, as well as more refresher trainings, on-the-job trainings, supervision and monitoring, which in turn increased screening both at health facility and community levels. This improves the quality of data collection, allowing better detection of malnourished children.
Figure 1: Total number of children screened using MUAC at community sites 2015-2017
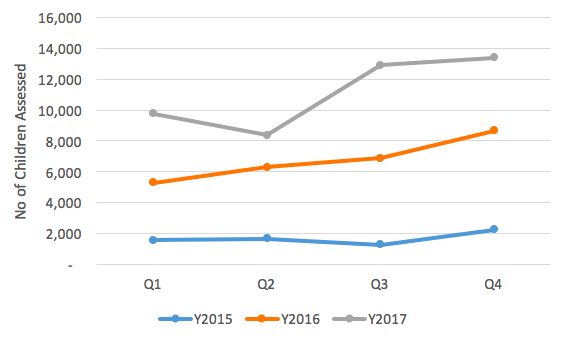
Figure 2: Total number of children assessed at health facility sentinel sites 2014-2017
Community and facility-level screening
In 2017 an average of 11,095 children per quarter from 868 community health posts were screened, an increase from 6,789 (Y2016) and 1,710 (Y2015). There was a lower number of reporting community sites (540) in the initial phase of implementation (2015-16); uptake was a little slower in the community compared to the health facility sites.
Numbers screened at health facility sites average 22,050 children per quarter from 175 health facilities in 2017, up from 18,649 in 2016, 6,718 in 2015 and 3,784 in 2014. Higher numbers of children screened at health facilities is expected, given this comprises children visiting the health facility directly as well as referrals from community, sometimes from beyond the geographical catchment of the health facility. The increasing numbers observed also reflects the phased approach in the scale-up process; ten provinces in 2014, 22 in 2015 and by 2016 all 34 provinces were on board. An analysis of SAM inpatient data (complicated cases) from the HMIS System (HMIS-DHIS2) shows a general increase in the number of admissions across the years (Figure 3). However, a mixed picture was observed whereby in 2015 the highest admissions were reported in Q2; for 2016 it was in Q3, whereas in 2017 the highest admissions were reported in Q1.
General high levels of acute malnutrition are being observed in children under two years old in the community as reported by the community sentinel sites, consistent with the protracted emergency situation in Afghanistan (Figure 4). A significant proportion of acute malnutrition cases are identified at community surveillance sites using MUAC; complicated cases are referred to the health facilities for further assessment and management as per IMAM protocol. At community level, CHWs are equipped with basic skills to provide nutrition promotional messages, including messages on optimal infant feeding.
Similar to the trends observed at community level, general high levels of acute malnutrition were observed in children under two years old at facility-level sentinel sites (Figure 5). Cyclical trends are emerging in which high levels of acute malnutrition are observed during Q3 and lowest levels in Q1. 2017 had slightly lower levels of malnutrition. The reasons that caregivers and children visit facilities (and are then screened) are varied, including visits for treatment of sickness, vaccinations, growth monitoring and promotion, antenatal care and contraception. Children screened are therefore random, with a possibility of unmeasured bias towards sick baby visits.
SAM prevalence at community level was generally lower in 2017 compared to 2016 (Figure 6). The peak of SAM in 2017 was reported in Q3, while the peak for 2016 was reported in Q2. With increased training and monitoring, CHWs are identifying acute malnutrition cases for management before they deteriorate into serious conditions.
SAM cases were somewhat higher at health facilities in 2017 compared to 2016. In both years the peak was reported in Q3, while lowest levels were reported in Q1. Assessments and interventions at health facilities are much more detailed; hence more at-risk and malnourished children are identified here and provided with the intervention or referred for further management whenever the health facility does not provide services such as inpatient management. There is an expected bias of likelihood of sicker children presenting at the hospitals and hence elevated proportions of acute malnutrition.
Figure 3: HMIS SAM inpatient admissions data 2015-17
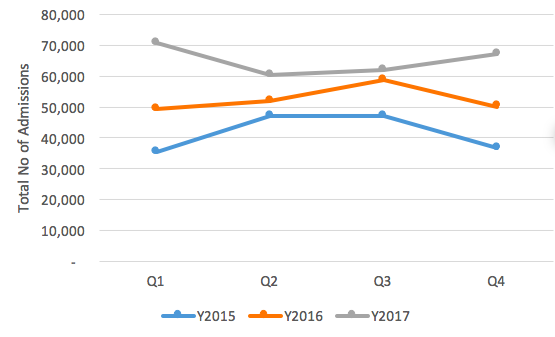
Figure 4: National community global acute malnutrition (GAM) trends 2016-2017
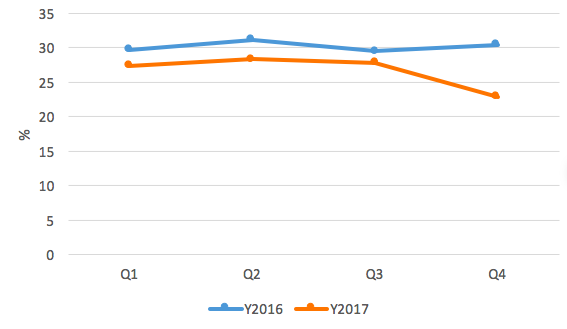
Figure 5: National health facility global acute malnutrition (GAM) trends 2016-2017
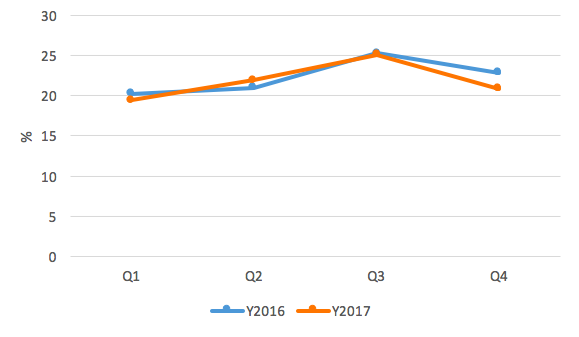
Figure 6: National community severe acute malnutrition (SAM) trends 2016-2017
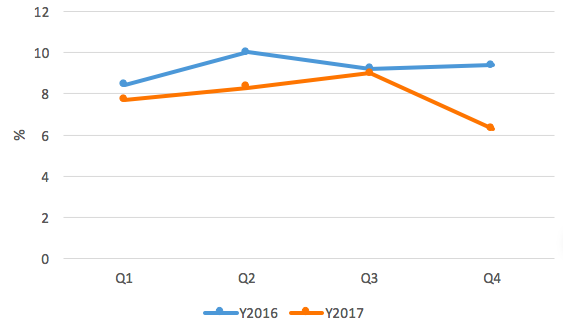
Figure 7 National health facility severe acute malnutrition (SAM) trends 2016-2017
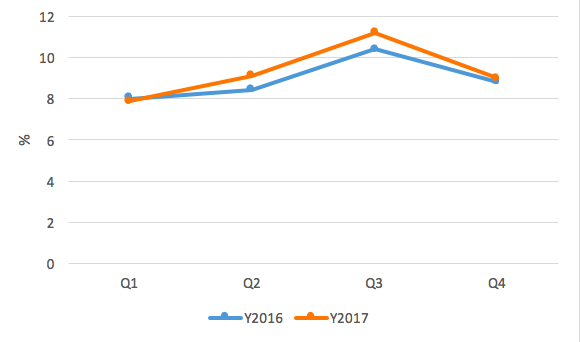 Figure 8: Infant feeding practices 2014-2017
Figure 8: Infant feeding practices 2014-2017
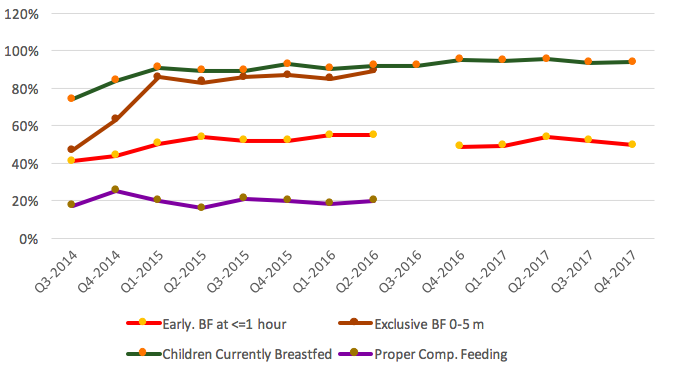
Infant and young child feeding (IYCF) practices
Comprehensive IYCF data was collected from 2014 until revisions were made in Q3-2016, when a decision was made to reduce the number of IYCF indicators. Justification for removing two main indicators, exclusive breastfeeding and appropriate complementary feeding, was based on lack of reliable data due to the considerable amount of time required to collect the information at a routine health facility. Initially reported rates of exclusive breastfeeding were low (Q1-Q2-2014), rising to above 80% between Q1-2015 and Q2-2016, when data collection stopped. The proportion of appropriate complementary feeding was consistently around 20%. Fairly consistent trends were observed across the reporting period, with most women reporting initiating breastfeeding within the first 24 hours. Marginal fluctuations were observed where, for example in Q4-2017, 49.7% infants were breastfed within one hour of delivery, compared to 52.1% in Q3-2017; otherwise the proportion was consistent from 2016 to 2017. The proportion of infants breastfed in the first hour was low between Q3-2014 and Q1-2015, when a steady rise in the proportion was reported. A total of 93.7% of infants aged under two years were currently breastfed (assessed using the standard WHO definition of continued breastfeeding rate at 20-23 months of age). This has been consistent across the reporting period Q1-2016 to Q4-2017. No data were collected in Q2 and Q3-2016 on early initiation of breastfeeding due to a revision of assessment tools, with resumption in Q4-2016 after consensus was achieved to retain the indicator.
Maternal health
Hb status was assessed for all pregnant women visiting the respective sentinel sites that provided maternity services. It has been observed that later-stage pregnancies (>= 24 weeks) have higher proportion of Hb deficiency (Hb) level < 11 g/dl) compared to earlier stage (<24 weeks). The proportion of all pregnant women with Hb level < 11 g/dl has been consistent across the reporting period, reaching a peak of 31.1% in Q4-2017 and a minimum of 26% for Q1 and Q2-2016. Further patterns by pregnancy stage are reflected in Figure 9.
Figure 9: Proportion of pregnant women with HB<11g/dL
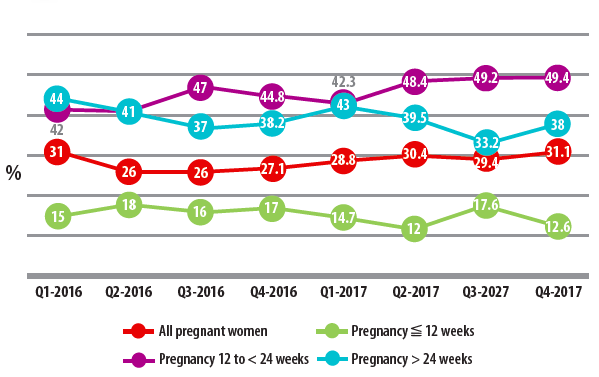
Figure 10: Birth outcomes 2016-2017 by quarter
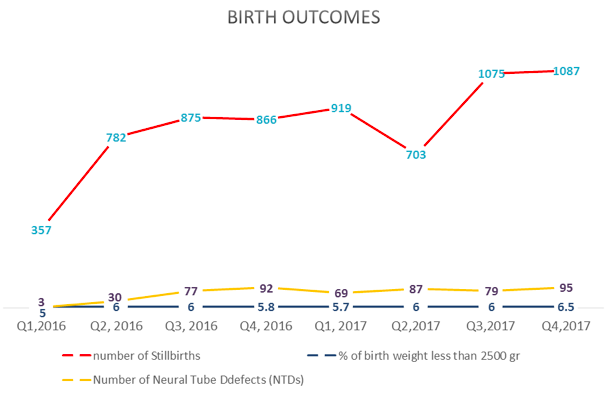
Birth outcomes
Birth outcomes were reported for all deliveries conducted at the sentinel sites that offer maternity services. The proportion of babies born with low birth weight was fairly consistent across the reporting period, hovering around 6% except for Q4-2017, where it slightly increased to 6.5%. Neural tube defects (NTDs) were prevalent, with increasing trends across the reporting period; a peak of 95 cases was reported in Q4-2017 (an increase from 79 in Q3-2017) out of a total of 33,239 births reported from maternity sites enrolled for the surveillance intervention. The lowest number of three cases in Q1-2016 is associated with under-reporting during the initial phases of the intervention due to non-standardised case definitions, which subsequently improved over the reporting period. NTDs (anencephaly, spina bifida and encephalopathy) have a strong association with folic acid deficiency.
Use of data
Data collected are of primary use by the health facilities and community posts. Beyond the health facility, central government uses the data to forecast trends in malnutrition and initiate in-depth assessments to establish the extent of the problem. Non-governmental organisations (NGOs) may use the data to support in-depth assessments in areas identified, on the basis of which subsequent assistance may be provided. In 2016 Action Contre la Faim (ACF) received funding to conduct SMART assessments to determine current nutrition status of children, based on triangulation of trends observed in the western region as well as HMIS and routine admissions data. Sub-national level data enables location-specific analysis, planning and intervention, which is particularly useful for health facilities compared to data produced at provincial level using statistical methods. Currently the database reports the data at provincial aggregate level, and follow-ups are made to health facilities for specific issues or unusual trends observed.
At national level NNSS data is used as one of the data sources when developing the Humanitarian Needs Overview (HNO) – the early warning function. The nutrition trends data was used in the prioritisation matrix in developing the 2017 Humanitarian Response Plan (HRP). In 2016 NNSS child nutrition trend data was used to inform in-depth population assessments. One of the provinces, Herat province, was prioritised for assessment through triangulation of NNS, HMIS and nutrition routine data. Observing the high levels of NTDs as well as anaemia levels among pregnant women resulted in the nutrition department reviewing the iron and folic acid supplementation intervention, after which it was noted that improvements in coverage as well as adherence to national protocols were needed.
Discussion
The trends are showing generally high levels of acute malnutrition amongst children < 2 years old. Similarly, general high levels of maternal malnutrition have been observed (30% with low Hb levels). Cyclical trends in the 2016-2017 period have emerged, with peak levels of acute malnutrition being observed for Q4 and the lowest levels in Q1. The main planting season in the country is between October and February, which coincides with the winter season. In recent years the winter agricultural season has been affected by low snow precipitation, river flows and dam levels compounded by inadequate moisture levels. There is likelihood of an association between the peak GAM levels and the poor agricultural season, although further analysis of the other existing EWSs may be needed to substantiate the extent to which the trends are related.
The GAM trends are largely similar for health facility and community sites, but GAM and SAM trends show a decreasing trend at community compared to health facility sites (2016 compared to 2017). It should be noted that, with increased mentoring, CHWs are better able to identify malnutrition cases and therefore community surveillance is identifying a significant proportion of acute malnutrition cases. However, it should be noted that community sites only carry out MUAC screening, while health facilities carry out more detailed assessments; therefore the community is an initial point for further referral. A bias is expected of the likelihood of sicker children presenting at the hospitals and hence elevated proportions of acute malnutrition is. These trends, as evidenced by the similar GAM trends observed at health facilities, point towards early detection; therefore strengthening of community referral systems is essential.
Lessons learned
It takes time to develop a fully functional nutrition information system. It has taken five years of continuous investments for Afghanistan to start realising the usefulness of the routine trend data. A phased approach in implementing the surveillance intervention ensured that critical lessons in the early phases were applied in the subsequent phases. Programme development at multiple levels and inter-departmental involvement enhances acceptability and likelihood of sustaining the intervention beyond project life. Maternal and child health outcomes are spread across the Nutrition, Reproductive and Maternal Child Health Departments, hence any efforts in improving data collection, reporting and analysis systems require active involvement of these key departments. Any exclusions will greatly stall the intervention and harmonisation may be far-fetched.
Too many indicators may affect data quality; therefore ‘less is more’. Some indicators, such as detailed IYCF assessment, may require surveys as they are more prone to measurement error and require considerable time, which may be impractical at a health facility providing routine services. Extensive indicator collection is beyond the capacity and time of a typical CHW. CHWs are an integral part of the health system and their role in screening, counselling and referrals needs to be strengthened. Options to improve performance (such as performance-based incentives in cash or kind) could be explored in different contexts.
In selecting sentinel sites, health facilities must be connected to community sites to facilitate monitoring as well as to link services. This approach follows the continuum of care logic whereby mothers and children receive referrals to and from health facilities, hence referrals can be tracked and easily followed up. The quality of routine data is always an issue, particularly in fragile environments like Afghanistan where insecurity may affect staff retention as well as monitoring of sites. It is therefore essential to factor in accessibility as one of the key criteria when selecting sentinel sites. Options to include children from inaccessible and insecure areas have been challenging, but the availability and use of mobile health teams is being considered nationally to capture the hard-to-reach children as much as is feasibly possible.
Selection of subjects to be entered into the surveillance registers may need to be exhaustive rather than a sample so as to minimise potential bias encountered during the assessments. This will ensure that entry into the registers is ongoing and will help keep track of actual caseloads, as well as help identify at-risk mothers and children visiting the health facilities.
Sustainable integration steps
Data are currently collected by health workers at health facilities at no additional cost. Timely and early feedback to health facilities on data is a simple way to help ensure data quality. The health workers’ capacity on nutrition surveillance processes has been continuously enhanced throughout the life of the intervention. Integration into the HMIS of key indicators will be the major milestone for ensuring continuity of the system. Having a sentinel system has been a strategy to avoid overloading the HMIS system; collecting too many indicators compromises the quality of data. The current nutrition indicators being collected through the HMIS at community level are number of children screened and referred using MUAC. At health-facility level, data is gathered on number of children weighed, number of children with acute malnutrition, low birth weight, and acute malnutrition management (admissions, cured, referrals, deaths and defaulters). The strategy of integration will apply lessons learnt from implementing the sentinel-based system.
The integration process has begun and includes steps for reviewing and updating the current nutrition indicators in the HMIS, modifying and adding more key indicators and maintaining a sentinel system which collects detailed indicators. In view of quality and reliability, a few IYCF indicators have been proposed to be collected at health facility level; early initiation as well as continued breastfeeding. The other detailed IYCF indicators will be collected in the periodic surveys. NTDs and anaemia in pregnancy have also been proposed for the HMIS, with the possibility of running a sub-database to maintain the other detailed indicators that cannot be integrated into the HMIS. This means the reviewed HMIS will run alongside the sentinel sites until full integration is achieved with the migration to the DHIS2 platform, an MoPH data warehouse (an online health information management system) that is being developed for the country. The DHIS2 is an improvement from the previous static HMIS system and the new system is expected to have greater capacity to manage health information.
The value of the routine data will rest in its capability to establish trend analyses, as has been observed. For added value of investment, efforts need to be focused on improving the quality of routine health-facility data through regular supervision visits, standardising equipment in use, and motivation of health workers for routine data to serve as early warning for potential nutrition and health problems in the population. The CHWs’ role in screening, counseling and referrals needs to be strengthened, as this facilitates early case detection, greater coverage and better treatment outcomes for children with acute malnutrition.
For more information, please contact Admire Chinjekure.


