Scale up of high-impact nutrition interventions in the informal settlements of Nairobi, Kenya
By Kassim Lupao and Esther Mogusu
Kassim Lupao is a senior manager for the Nairobi urban health and nutrition programme at Concern Worldwide. He has many years of experience in the implementation of high-impact nutrition interventions in urban contexts, is a trainer of trainers in nutrition programming, and has helped develop Nairobi county nutrition assessments, strategies and action plans.
Esther Mogusu is the county nutrition coordinator for Nairobi City County. She has over 15 years of experience in implementing nutrition programmes in Kenya at health facility, sub-county and county levels. She is a mentor and trainer of trainers in nutrition programming.
The funding to support scale up of high-impact nutrition interventions in Nairobi was funded by UNICEF.
Location: Kenya
What we know: Scale-up of high-impact nutrition interventions (HINI) is necessary to comprehensively address malnutrition.
What this article adds: In Nairobi county wasting prevalence in urban informal settlements is normal but caseload is high; stunting, micronutrient deficiencies and obesity are also prevalent. Concern Worldwide implemented a five-year programme of support to government to scale up HINI through the health system in Nairobi. Activities included strategic policy development, nutrition assessment and analysis, health worker nutrition capacity development and development of an urban early warning system and emergency nutrition response mechanism. This has contributed to improved coverage of HINIs and acute malnutrition programming and reduced prevalence in stunting, wasting and underweight. Challenges to HINI scale-up include limited and short-term funding, shortfalls in community nutrition capacity, insufficient government budgetary allocation and predominance of private health care. This successful partnership will continue to 2022, prioritising stunting impact. More broadly, new thresholds and ways of working are needed for urban emergency response programming.
Background
Nairobi informal settlements
Over 60% of the urban population in Nairobi live in informal settlements on 5% of the land (Nairobi Urban Sector Profile, 2006). The poorest urban-dwellers spend up to three quarters of their income on staple foods alone (Oxfam, 2009) and regularly engage in negative coping strategies, such as reducing the number of meals consumed, decreasing food variety and quality, and food scavenging. Residents living in informal settlements are vulnerable to rising prices as they are highly dependent on the market for their food and non-food needs. Informal settlements in Nairobi are characterised by inadequate access to potable water and sanitation facilities, leading to increased risk of waterborne, food-borne and vector-borne diseases such as diarrhoea, cholera, typhoid and malaria. Children under five years old attending informal daycare centres are particularly vulnerable, due to lack of regulation and staff training and inadequate food and play activities.
Research shows that only 39% of children between six months and two years living in urban slums of Nairobi receive an adequate diet, in terms of both quantity and diversity (Concern Worldwide and Welthungerhilfe, 2009). Deficiencies are common in iron, zinc, vitamin A, vitamin C and protein, and most caregivers do not feed their children appropriately during and after illness (Concern Worldwide, 2014). Although the prevalence of acute malnutrition is relatively low in Nairobi County, at 54,438 cases the burden of acute malnutrition is the second highest in Kenya due to population density (Kenya Food and Nutrition Security Seasonal Assessment, 2018). One in every three children is stunted (SMART survey, 2017) and, in terms of absolute numbers, Nairobi County has the highest caseload of stunted children in the country at 104,074 children (Kenya Food Security Steering Group, 2018). Substantial levels of overweight/obesity have also been observed, demonstrating the double burden of malnutrition; in Nairobi 43% of women are obese, compared to 25% of women of reproductive age nationally (KNBS, 2009). Childhood obesity is also on the rise, although the problem is much more prevalent among adults at present.
Concern urban nutrition programme
Concern Worldwide has partnered with the government to support scale-up of HINI in Nairobi since 2012. This support has focused on strengthening county government health systems to support the delivery of quality health and nutrition services to children under five years old and pregnant and lactating women (PLW) and improving community-based services through participatory approaches to behaviour change and innovations in emergency nutrition programming, including preparedness. Funded by UNICEF, Concern Worldwide supported implementation of HINI in Nairobi’s informal settlements between 2012 and 2017 (US$2.5 million).
Package of support to scale up HINI
Policy development
Concern Worldwide has played a critical role in supporting Nairobi City County to develop key strategic documents, including the Urban Nutrition Strategy (UNS), the first County Nutrition Action Plan (CNAP) (2013-2017), the County maternal infant and young child nutrition (MIYCN) Social Behaviour Change and Communication Strategy (SBCC), and the County Nutrition Capacity Development Framework. Development of the UNS has been critical in highlighting the unique nutrition challenges in an urban context. As a result, other donors are now showing interest in funding urban nutrition projects, such as the Korea International Cooperation Agency (KOICA), which is supporting implementation of a nutrition innovations project called ‘Lishe Poa’ that aims to develop a highly nutritious, affordable and ready-to-eat product that will be promoted in the informal settlements as a replacement for popular but unhealthy street foods. The CNAP guides and costs nutrition interventions in the County and is used as a tool to advocate for government to increase allocation of resources for nutrition services. Such advocacy efforts have been successful; for 2018/2019 the City County of Nairobi has allocated 10 million KES (Kenyan Shillings) to the County Nutrition programme, compared to 2012 when nutrition services were 100% supported by development partners. The Nairobi County MIYCN SBCC strategy was developed to operationalise the MIYCN policy to protect, promote and support optimal maternal, infant and young child feeding practices and improve child survival, and to provide strategic guidance for implementation of focused interventions as outlined in the Advocacy, Communication and Social Mobilization (ACSM) strategy (an advocacy strategy for nutrition interventions in Kenya).
Nutrition assessments and capacity-building
Concern Worldwide has supported the City County of Nairobi by conducting a series of nutrition-related surveys and assessments to provide evidence for decision-making and policy direction. Baseline and endline nutrition programme coverage surveys (2012 and 2018) and SMART surveys (2014 and 2017) were conducted. A nutrition bottleneck analysis and nutrition causal analysis for Nairobi County were carried out in 2017. Health management team members at both county and sub-county levels were trained to conduct coverage and SMART surveys and bottleneck and causal analyses, and were involved in the whole survey process (training of enumerators, supervision of data collection, supervision of data entry and analysis, report writing and dissemination of results).
Concern Worldwide also provided technical and financial resources to carry out a nutrition capacity-gap analysis in 2016 for Nairobi County. Health management team members at county and sub-county levels were trained and supported to conduct analysis around the pillars of the health system. Results (summarised in Box 1) were used as a basis for a county nutrition capacity development framework, which prioritised key capacity-building activities (classroom trainings, on the job training and mentoring) for the nutrition workforce, including all health cadres involved in providing nutrition services through to community health volunteers and community health assistants involved in delivering nutrition services at community level. Concern Worldwide supported training of the health management team as trainers in IMAM, MIYCN and the Baby Friendly Community Initiative (BFCI), and in how to provide on-the-job training and mentorship to healthcare workers. The training was then cascaded by the health management team. It is expected that such training will be carried out with government support in future as part of the increased budget allocation to nutrition services. Concern Worldwide also facilitated the development of Nutrition Technical Forums (NTF) at county and sub-county levels that bring together stakeholders implementing both nutrition-specific and nutrition-sensitive interventions in the county. These complement the work of existing multi-sector platforms, which exist to support a range of outcomes, not just nutrition.
Box 1: Nutrition capacity in the Nairobi County health system: Key findings (2016)
Nutrition service needs in Nairobi county are covered by the County Integrated Development Plan (CIDP) and the County Health Sector Strategic and Investment Plan (CHSIP). Nairobi City County also has a County Nutrition Action Plan (CNAP) that specifies the capacity of the health system to deliver on nutrition. Coordination of nutrition services occurs through a county and sub-county Nutrition Technical Forum (NTF), which brings together nutrition stakeholders across the county to discuss how the nutrition agenda can be taken forward. A multi-sector platform also exists at county-level that brings together nutrition; water, sanitation and hygiene (WASH); agriculture; social services and education sectors. Challenges described include difficulties in the dissemination and application of key nutrition policy documents, such as the Breast Milk Substitutes (BMS) Act (2012), to health facility and community levels, resulting in poor implementation and enforcement. This highlights the need to strengthen the multi-sector platform.
Private, faith-based and non-governmental organisation (NGO) owned hospitals constitute 78% of Nairobi County’s health facilities and provide the bulk of nutrition services in the informal settlements (this is much higher than in rural areas in Kenya, where health services are predominantly government-owned). Most HINIs are offered at health facility level, but very few are offered at community level due to low coverage of community health units and limitations of the nutrition workforce in the community. Many health workers (nutritionists and other cadres) have been trained in national guidelines on the IMAM, MIYCN and the Kenya Medical Supplies Agencies (KEMSA) Logistics Management and Information System (LMIS); however, new skills are not always practiced and training available to the community-level workforce is more limited.
Ten per cent of the county’s health budget is allocated to the reproductive, maternal, newborn, child and adolescent health (RMNCH) sub-programme, within which nutrition is a delivery unit. Around 75% of the RMNCH budget allocation pays for health worker salaries, with little resources allocated to service development.
HINIs described within the CNAP are not adequately financed; therefore the county is heavily reliant on partners for HINI implementation. Equipment to assess nutrition status is available at health-facility level, although not always in adequate supply. Nutrition supplies for managing acute malnutrition and routine medications are available at health facilities, although occasional stockouts are experienced due to debts owed to KEMSA; an overreliance on partners to procure nutrition supplies and commodities persists.
All nutrition-related data collection tools are available at health-facility level, with the exception of the Maternal and Child Health (MCH) handbook.
Emergency preparedness
Concern Worldwide supported the City County of Nairobi to mitigate and respond quickly to the impacts of slow-onset emergencies by establishing an Urban Early Warning and Early Action (UEWEA) system. The UEWEA system was born out of the Indicator Development and Surveillance for Urban Emergencies (IDSUE) project that Concern Worldwide successfully piloted for five years in informal settlements of Nairobi. The system is based on five key indicators: percentage of households experiencing shocks; equivalised monthly income; number of food baskets; percentage of households with at least one stable income-earner; and percentage of households with at least one child reporting diarrhoea. The county is being supported by the Kenya Red Cross Society to collect monthly surveillance data from the informal settlements to feed into the UEWEA system, after which results are summarised as ‘normal’, ‘alert’, ‘alarm’ or ‘emergency’. Thresholds for each category were set based on data from the five-year pilot phase (see Table 1). Once the normal threshold is surpassed, the county government mobilises resources to respond to the situation; emergency response actions are mounted when UEWEA indicators indicate an emergency situation, an example of which is provided in Box 2.
Table 1: Thresholds for the UEWEA system
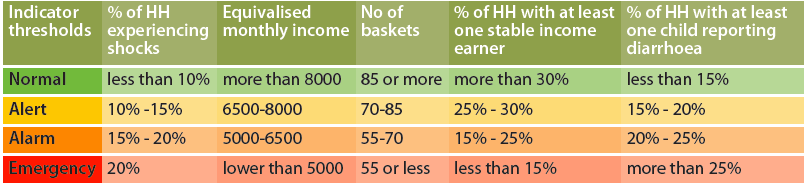
HH = households
Box 2: Case study of county-level response to the Urban Early warning and Early Action (UEWEA) system
A drop in the number of food baskets and a surge in diarrhoea cases were reported to emergency thresholds in three of the sentinel surveillance sites (Korogocho, Mukuru and Kibera) in February 2017, May to June 2017, and November 2017. In response Concern Worldwide liaised with health management team members at both county and sub-county levels to plan and mount the following response activities: mass screening and referral of children with acute malnutrition; distribution of water purification products for treatment of water at both household level and at designated water points; treatment of active diarrhoea cases with zinc and oral rehydration solution (ORS), including referral of severe cases for further management at the nearby health facilities.
A total of 32,244 children under the age of five was screened; of these 131 were diagnosed with severe acute malnutrition (SAM) and 849 were diagnosed with moderate acute malnutrition (MAM). All were referred for management. Without the UEWEA surveillance system, such children would not have been identified and referred for treatment.
Concern Worldwide also supported the county to rollout IMAM surge using a phased approach. IMAM surge aims to build the resilience of the health system to better deliver services for treatment of acute malnutrition over time, particularly during periods of high demand, without undermining the capacity and accountability of government health actors. During the first phase of implementation, 18 health facilities (at county and sub-county levels) were targeted through the training of two county trainer of trainers (TOTs) and 24 sub-county TOTs, who then cascaded training to healthcare workers in the 18 identified health facilities. During implementation of IMAM surge, seven health facilities were able to surpass their normal IMAM surge thresholds and no health facilities hit emergency thresholds, indicating that the health system managed to handle the situation. During surge periods, health facilities notified the health management team members and, depending on the IMAM surge phase, scale-up surge actions were undertaken, such as mass screening of children under the age of five in the health facility catchment areas, prepositioning of medical and nutrition supplies. and cancelling healthcare workers’ leave. At the county and sub-county levels, health management team members monitored implementation of IMAM surge activities using dashboards that were updated monthly, indicating which health facilities had passed normal thresholds and needed IMAM surge actions.
Nutrition programme coverage and nutrition outcomes
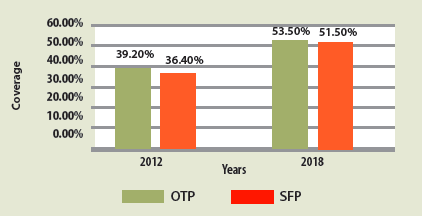
Findings of nutrition SMART surveys conducted in 2014 and 2017 indicate marked improvements in the coverage of all HINI indicators over this period, including deworming of children aged 12-59 months (59.0% to 65.1% versus target of 50%); zinc supplementation for management of diarrhoea among children under five years old (29.0% to 73.0% versus target of 80%); vitamin A supplementation for children aged 6-11 months (81.7% to 87.2%) and children aged 12-59 months (36.4% to 80.2%) (versus target for age 6-59 months of 80%) and iron and folic acid supplementation (IFAS) (23.9% to 56.7% versus target of 80%) (Figure 1). While targets were met for two HINI indicators (deworming and vitamin A supplementation), zinc supplementation for management of diarrhoea among children under five years old fell slightly short of target coverage. Achievement of IFAS for pregnant women improved but fell far below the set target. This was mainly due to supply challenges as IFAS was not included in the essential drug list; however, it is now and going forward all pregnant women will be supplemented as per the schedule.
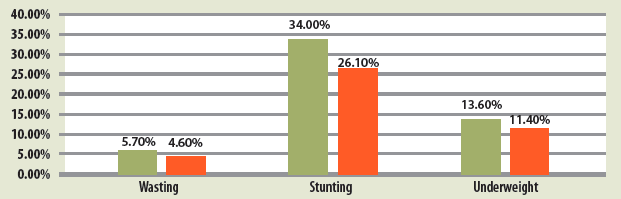
Coverage of the county’s outpatient therapeutic programme (OTP) improved from 39.2% in 2012 to 53.5% in 2018, while the county’s supplementary feeding programme (SFP) coverage improved from 36.4% in 2012 to 51.5% in 2018 (Figure 2). Results of SMART surveys show that stunting prevalence declined from 36.0% in 2014 to 26.0% in 2017; wasting prevalence reduced from 5.7% in 2014 to 4.6% in 2017; and prevalence of underweight reduced from 13.6% in 2014 to 11.4% in 2017 (see Figure 3).
Aside from some small-scale interventions, such as that of Afya Jijini, which conducted nutrition-related trainings, Concern Worldwide’s programme of health systems strengthening was the only large-scale, systematic programme over this period to work with the government to identify gaps in the health system and develop a clear plan of response. Improved coverage of nutrition programmes and nutrition outcomes over this period can therefore reasonably be attributed to the government’s commitment and dedicated actions to develop health system capacity and scale up key actions and the technical and financial support provided by Concern Worldwide.
Figure 1: Coverage of HINI indicators Nairobi County 2014 and 2017
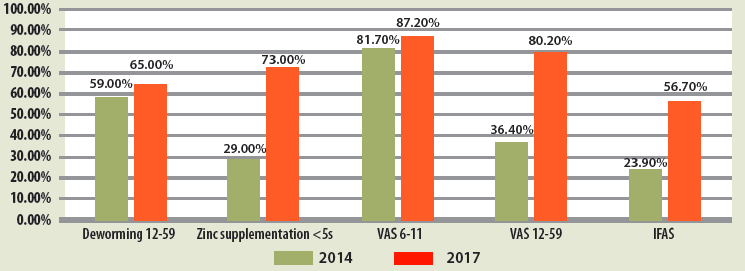
Figure 2: IMAM coverage Nairobi County 2012 and 2018
Figure 3: Nutrition status of children under five years old, Nairobi County 2014 and 2017
Challenges
Limited and short-term funding: Not many donors are familiar with urban contexts and interest in funding urban programmes is low. Donor resources are traditionally channelled to areas with high prevalence of malnutrition, rather than considering caseload. Over the years, Concern Worldwide has received short-team (yearly to two-yearly) funding to support implementation of HINIs in Nairobi County, which hampers scale-up across all health facilities. Inconsistent funding has also led to interruption of HINI services. A case in point is the period between January to July 2016, when the Nairobi urban nutrition programme did not have funding and services were temporarily suspended.
Inadequate budgetary allocation for nutrition by the county government: The nutrition programme in Nairobi has a costed nutrition action plan. However, a large proportion of resources received by the County Department of Health from the national treasury goes towards taking care of recurrent expenditures, with few resources left for development purposes. In addition, due to government bureaucracy, it is difficult for the County Department of Health to access the few resources for development that are available; hence the government relies heavily on partners to implement HINI.
Insufficient nutrition workforce: The County has a total of 130 health facilities implementing HINIs but only 52 nutritionists, out of which 12 are serving in managerial positions at county and sub-county levels. The remaining nutritionists are distributed between county referral hospitals (level-four health facilities) and a few health centres (level-three health facilities). There are no nutritionists working in any of the dispensaries (level-two health facilities) and at the community (level one). This situation has meant other cadres of health workers, especially nurses and clinical officers, have had to take up nutrition roles while they are already overwhelmed with existing responsibilities.
Low coverage of community health units (CHU): Based on the population in the county, Nairobi should have at least 868 Community Health Units (CHU); however, only 217 exist, of which only 121 are functional (the rest are completely non-functioning), which hampers efforts to create demand for nutrition services at community level. In addition, low coverage of CHUs limits capacity to follow up clients at the community level, which may hamper recovery rates.
Private health care: The majority of health facilities in the urban informal settlements are privately owned, which makes health services expensive for residents when they would otherwise be free for children under five years old and PLW. There is therefore need for public private partnerships (PPP) to ensure access to quality nutrition services, especially in the informal settlements.
Conclusions and recommendations
Scale up of HINI services in the informal settlements of Nairobi through existing government health structures and with technical support from Concern Worldwide resulted in improvement in the nutrition status of children under five years old. There was also a notable improvement in the coverage of OTP and SFP services. This provides evidence that scale-up of HINIs through the strengthening of existing health systems is a viable approach that could be applied to other urban areas. While wasting prevalence is acceptable, absolute numbers are usually very high. This requires a new way of thinking; for example, coming up with urban-specific thresholds (as per the UEWEA) to determine when to mount emergency nutrition interventions.
Heavy dependence on development partners to fund HINI scale-up persists. A review of the key strategic documents, including the UNS and the Kenya Nutrition Action Plan (KNAP), is needed to ensure that they capture the challenges faced by the urban nutrition programme and to direct budgetary allocations towards development to address these.
Scale-up of HINIs in Nairobi continues to face the challenges of limited and short-term funding that is secured based on prevalence rather than caseloads. Continued advocacy is needed with donors to inform and change practice.
Increased advocacy is needed to the government and other key stakeholders to allocate resources for strengthening community-level health and nutrition services, including recruitment of more nutritionists.
Advocacy is also needed to the government to embrace PPPs, whereby the government provides drugs and additional healthcare workers in private healthcare facilities to enable poor residents in the informal settlements to access healthcare services at an affordable rate.
Scale up of HINI services in Nairobi County has continued beyond this first phase, funded by a county government allocation of KES 10 million and by UNICEF (to Concern Worldwide) to support this process up to 2022. Looking ahead, tackling childhood stunting is a high priority for the Nairobi urban nutrition programme, since stunting is the predominant form of malnutrition in the County. Investment in the government’s BFCI and promotion of MIYCN practices are priorities to this end.
For more information, please contact Kassim Lupao.
References
Nairobi Urban Sector Profile, 2006. https://unhabitat.org/books/kenya-nairobi-urban-profile/
OXFAM, 2009, Urban Poverty and Vulnerability in Kenya. https://urbanhealthupdates.files.wordpress.com/2009/09/urban_poverty_and_vulnerability_in_kenya1.pdf
The Global Hunger Index report 2009, Concern Worldwide and Welthungerhilfe. The link between gender inequality and hunger.
Process for Improving Child Feeding (ProPAN) (2014), Preliminary Report, Concern Worldwide. Social determinants of child under-nutrition in urban informal settlements in Kenya.
Kenya Food and Nutrition Security Seasonal Assessment, 2018 available at http://www.nutritionhealth.or.ke/reports/seasonal-assessment-reports/situation-reports/
Nutrition Survey Conducted in The Slums of Nairobi County, May 2017 (SMART survey) available at http://www.nutritionhealth.or.ke/reports/smart-survey-reports/
Kenya Demographic and Health Survey 2008-09. Kenya National Bureau of Statistics (KNBS), ICF Macro (2009). Calverton, Maryland: KNBS and ICF Macro. Available at http://dhsprogram.com/pubs/pdf/fr229/fr229.pdf.
Food and Agriculture Organization (FAO) of the United Nations (2006). The double burden of malnutrition. Case studies from six developing countries. FAO food and nutrition paper 84. Rome: FAO. Available at www.fao.org/docrep/009/a0442e/a0442e03.htm