Development of a maternal service package for mothers of children with severe acute malnutrition admitted to nutrition rehabilitation centres in India
By Vani Sethi, Praveen Kumar and Arjan De Wagt
Vani Sethi PhD is a public health nutritionist in the Nutrition Division, UNICEF India, presently leading a girl’s and women’s nutrition programme linking nutri-based livelihoods and empowerment and supporting the Ministry of Health in maternal malnutrition and anaemia programmes. She has 17 years’ experience in several Indian programming contexts, including rural, tribal and urban slums.
Dr Praveen Kumar is a paediatrician and Professor of Pediatrics at Lady Hardinge Medical College and Kalawati Saran Children’s Hospital in New Delhi. He runs India’s national centre of excellence on severe acute malnutrition and supports the Ministry of Health in the development of protocols for management of children with severe acute malnutrition and HIV and capacity-building.
Arjan de Wagt is Chief of the Nutrition Section, UNICEF India country office, New Delhi. He has over 25 years’ international experience in several countries, including Nigeria, Zambia, New York and Netherlands and has specialised in the management of severe acute malnutrition, emergency nutrition and nutrition in HIV.
The authors are grateful to Kalawati Saran Children’s Hospital, Hindu Rao Hospital, Bhagwan Mahavir Hospital and Jawaharlal Nehru Medical College for user of their premises in data collection. The authors recognise and thank all partners, consultants (Shikha Sayal, Swati Dogra and Dr Neha Sareen) and advisors (Dr HPS Sachdev, Dr Manju Puri and Dr Neena Bhatia) who have supported the work highlighted in this article at various stages, including the Maternal Health Division, Ministry of Health and Family Welfare, Government of India, New Delhi. This work was funded by UNCEF India.
Location: India
What we know: Maternal factors, such as poor nutrition in utero, anaemia and short birth spacing, contribute to undernutrition in children.
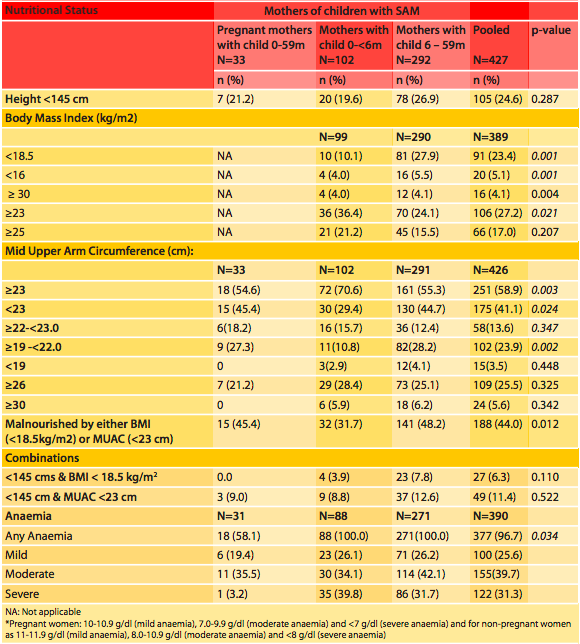
What this article adds: The socio-economic, anthropometric, morbidity and biochemical profile of 427 mothers of inpatient children with severe acute malnutrition (SAM) admitted to four nutrition rehabilitation centres (NRCs) in India was assessed. Twenty-five per cent of mothers were low in stature (height <145 cm); 23% were underweight (body mass index (BMI) <18.5 kg/m2); 5% were severely underweight (BMI <16); more than a quarter (27%) were overweight/obese (BMI ≥23 kg/m2); and 71% had moderate or severe anaemia. Of 33 mothers who were also pregnant, 41% had low mid-upper arm circumference (<23 cm). Diarrhoea, urinary tract infection and genital infection were common and use of family planning methods was low (23%). Findings informed the development of a maternal service package integrated within existing government services and according to nutrition/medical risk of mothers. Further research is needed to test the effect of the protocol on maternal nutrition outcomes and its operational feasibility at scale.
Background
In India 8% of children under five years old suffer from severe acute malnutrition (SAM) (NFHS 4, 2015-2016). Underlying causes of SAM in children are directly and indirectly related to maternal factors such as poor nutrition in utero, short birth spacing and household food insecurity. Currently 1,151 functional nutrition rehabilitation centres (NRCs) are set up by the Government of India (GoI) under the Ministry of Health and Family Welfare (MoHFW) to provide inpatient care for children under five years old with SAM with medical complications (~10% of burden of SAM) (MoHFW, 2011). A typical NRC has 10 to 20 beds where mothers/caregivers stay with admitted children for the duration of treatment (7-14 days) and attend daily group and individual counselling sessions to prepare them for discharge.
Limited information exists on the nutritional profile of mothers of children with SAM in India. Facility and community-based studies with small sample sizes show that mothers of children with SAM are often underweight (33%-50% of mothers had a body mass index (BMI) <18.5 kg/m2 in a study by Bhandari et al, 2016), and anaemic (70%-88% in studies by Rai et al, 2015 and Nagabhushan et al, 2017); however, more research and national protocols are needed to support the effective screening and management of maternal malnutrition (including undernutrition, overweight and obesity) at facility and community levels.
The aim of this study was to bridge this knowledge gap by assessing the nutritional status of mothers of children with SAM admitted to four NRCs in Delhi and Aligarh, Uttar Pradesh, and, based on the results, develop a maternal service package of interventions for mothers to be integrated in routine NRC services.
Methods
The study was conducted in two phases: in phase one the nutritional status of mothers was profiled and in phase two a maternal service package was developed. The first phase was conducted between September 2016 and November 2017 in four NRCs. Three NRCs were located in Delhi (Kalawati Saran Children’s Hospital, Hindu Rao Hospital and Bhagwan Mahavir Hospital) and one in Aligarh (Jawaharlal Nehru Medical College and Hospital of Aligarh Muslim University). In each NRC, once the SAM child had been stabilised, all mothers were invited to enrol in the study and informed consent was obtained. No mothers declined to take part.
Socio-demographic profile was recorded on a pretested proforma. Maternal weight was measured using UNICEF SECA weighing scales (model 874) with at least 100 grams gradation. Height was recorded using UNICEF SECA microtoise (model 216) with 0.1 cm gradation and mid-upper arm circumference (MUAC) using MUAC tape (procured from UNICEF supply department) with a gradation of 0.1 cm. World Health Organization (WHO) classifications were used to classify short stature and thinness based on BMI and anaemia (WHO, 1995, WHO, 2003, 2011). South Asian classifications of overweight (≥23 kg/m2) and obesity (≥26 kg/m2) (WHO, 2003) were also used. MUAC <23 cm and MUAC <19 cm were used as alternative cut-offs to define malnutrition and SAM respectively (MoHFW, 2017). MUAC ≥30 cm was used to define overweight or obesity (Khadivzadeh, 2002). Venous blood sample was collected from consenting mothers for haemoglobin estimation using Erba Sysmex KX-21 auto-analyser. Descriptive statistics were generated using SPSS version 12.0.
Results are presented for all mothers, in three stratified categories: those who were pregnant and had a SAM child aged 0-59 months (n=33); non-pregnant mothers with a SAM child aged less than six months (n=102); and non-pregnant mothers with a SAM child aged 6-59 months (n=292). Chi-square test was used to compare the nutritional status of mothers between the three groups.
Phase two entailed the development of a maternal service package. A nodal pre-testing centre was identified (Kalawati Saran Children’s Hospital, paediatric ward NRC), a technical expert group formed and GoI/WHO nutrition guidelines reviewed. The findings of phase one were presented to technical experts and GoI officials and a protocol and counselling aids were developed and refined. The final protocol was implemented as part of routine service provision in the NRC by a nutrition counsellor post-graduate nutrition researcher on a sample of 100 mothers over a period of six months (December 2017 to May 2018). During this time changes were continuously made to the algorithm and counselling aids for further contextualisation. The maternal service package was then presented to the GoI.

Results
Phase 1: Profiling the nutritional status of mothers
General characteristics
A total of 427 mothers with a child admitted to an NRC participated in the study: 203 (47.5%) from Kalawati Saran Children’s Hospital, 144 (33.7%) Hindu Rao Hospital, 64 (15%) Jawaharlal Nehru Medical College and 16 (3.8%) Bhagwan Mahavir Hospital. Of the 427 mothers, 102 (24%) had an infant aged 0 to less than 6 months of age; 292 (68%) had a child aged 6 to 59 months; and 33 (8%) were pregnant (as well as having an admitted child of 0-59 months of age). The mean age of mothers was 18.9 years (range: 16-32 years). The majority of mothers were Hindus (65%), unemployed (89%) and had more than four family members (89%). Forty per cent of mothers had never attended school and 23% had studied until higher secondary school. Adoption of family planning methods was low (23%).
Anthropometry
Of the 427 mothers assessed, 25% were low in stature (stunted, height <145 cm) and 44% of mothers were malnourished either by BMI or MUAC. By BMI, 23% were underweight (BMI <18.5kg/m2), which is comparable to the national average of 22.9% (NFHS 4 2015-2016), and 5% were severely underweight (BMI <16 kg/m2). By MUAC, 41% were malnourished (MUAC <23cm) and 3.5% were severely malnourished (MUAC <19cm) (no national data to compare).
Overweight or obesity was documented in 27% (by Asian cut-off, BMI ≥ 23 kg/m2) and 17% (by WHO cut off of ≥25kg/m2), which is slightly lower than the national female average of 20.6% by WHO cut-off (NFHS 4 2015-2016)). Obesity was documented in 13% by Asian cut-off of BMI ≥ 26 kg/m2 and 4% by WHO cut-off of ≥30kg/m2. According to MUAC ≥30 cm obesity was observed in 6% of mothers.
Anaemia
Haemoglobin concentration was measured in 390 consenting mothers, of whom 377 (97%) were anaemic and 71% were moderately or severely anaemic. Morbidities such as diarrhoea (15%), urinary tract infection (UTI) and genital infection (20%), chronic cough (12%), Bitot’s spot (4%) and fluorosis (1.3%) were common among mothers who were stunted, underweight or overweight/obese. Cases of diarrhoea were higher in mothers who were underweight compared to mothers who were overweight (5% vs 1%) (Table 1).
Table 1: Nutritional status of mothers of children with severe acute malnutrition (N=427)
Phase 2: Development of a maternal service package
The GoI offers a service package to mothers through various antenatal and postnatal care platforms, targeted at pregnant mothers and those with infants aged 0 to 6 months. These include: i) physical examination (height and weight); ii) laboratory investigation (haemoglobin estimation and oral glucose tolerance test); iii) iron and folic acid (IFA) and calcium supplementation; iv) deworming; and v) counselling (on healthy eating and diet diversity, family planning, micronutrient supplementation, personal hygiene, and food and recipe demonstration). Additionally, there are protocols in place for screening and management of adult severe thinness and severe anaemia which are used in tuberculosis wards and haematology departments.
The protocol developed for this study examined these guidelines in the context of routine services provided in an NRC setting with a view to expanding the appropriate support to all mothers with a SAM child admitted to an NRC. Building on what exists, a protocol was developed whereby mothers are screened using the criteria outlined in Table 2 and classified as: i) not at nutritional risk; ii) at some nutritional risk; or iii) at severe nutritional risk/medical risk. Nutrition interventions for each group were developed as follows:
1. Universal interventions for all mothers not at nutritional risk
i. Hospital diet
As per the Operational Guidelines on Facility Based Management of Children with SAM (MoHFW, 2011) and Janani Shishu Suraksha Karyakaram (JSSK) diet guidelines (MoHFW 2018), the mother or the caregiver staying with the child is provided with food by the NRC, funded by the State Program Implementation Plans (PIPs) approved by the MoHFW.
ii. Micronutrient supplementation and deworming
As per GoI guidelines, IFA and calcium supplements are provided to pregnant mothers from the second trimester onwards to six months post-partum if not already provided elsewhere (one IFA tablet daily (60 mg iron and 500 mcg folic acid) and two calcium tablets (500mg)). As per GoI guidelines, mothers in the second trimester of pregnancy are provided with a single oral dose deworming tablet (400 mg of albendazole) if not already provided elsewhere.
iii. Group-based nutrition education and counselling
Child-focused group counselling is provided in most NRCs daily for one hour. In the proposed NRC protocol, daily group counselling is extended by 30 minutes to focus on the mother as well. Group counselling takes place five days per week, covering one of five thematic areas per day (micronutrients and anaemia; diet diversity; personal hygiene and sanitation; breastfeeding, family planning; and non-communicable and communicable diseases, including TB, HIV, malaria, obesity, hypertension and diabetes). During Phase 2, group counselling aids were developed to help staff deliver the counselling (pictorial flip book, game, food plate model, recipe book for underweight and obese and pocket cards for testing their knowledge).1 Pretesting showed that the counselling aids are easy to carry around the wards and simple to use and understand, with emphasis on important points. They were also found to increase the interest and involvement of the mothers.
Table 2 Maternal services package for Nutrition Rehabilitation Centres
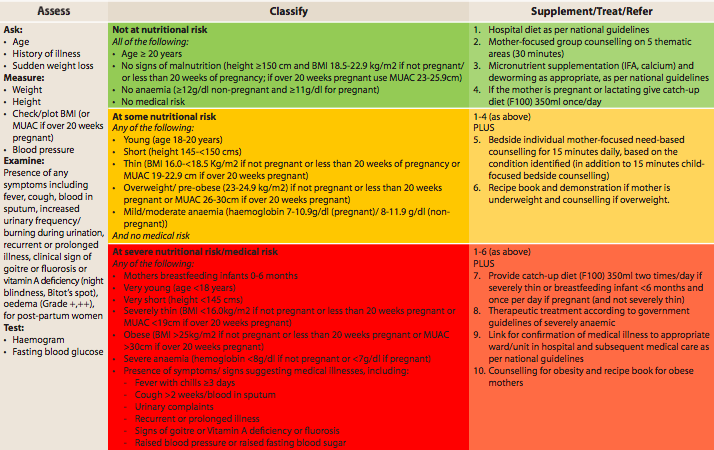
2. Additional interventions for mothers at some nutritional risk
In addition to the universal interventions, 15 minutes of individual, mother-focused, bedside counselling is provided for mothers deemed to be at some nutritional risk in addition to the routine 15 minutes of child-focused bedside counselling. Counselling is tailored to the mother’s specific nutritional risk. In addition, those mothers identified as having mild or moderate anaemia are provided with a therapeutic dose of oral IFA, as per GoI guidelines.
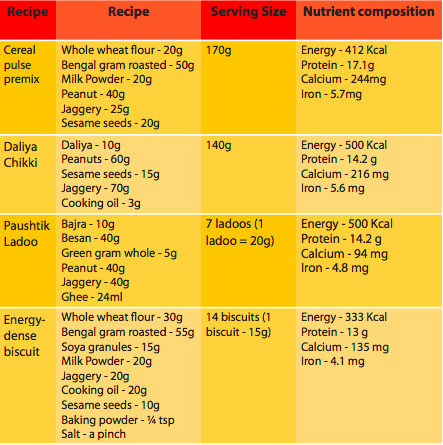
A recipe book was developed for underweight mothers, which was explained through live demonstration sessions based on four local recipes (see Table 3). Pretesting showed that mothers took a keen interest in these sessions, which were successful in increasing their involvement and practical knowledge.
Table 3: Composition and nutrient content of the recipes developed for food demonstration using local ingredients
3. Additional interventions for mothers at severe nutritional risk/medical risk
In addition to universal interventions and those targeted to mothers at some nutritional risk, extra support is provided to mothers deemed to be at severe nutritional or medical risk (see Table 2 for criteria). Several options for an enhanced energy-dense supplement were developed but, after pre-testing with mothers, F-1002 was found to be the most feasible as it is already provided to the SAM child after stabilisation (for ‘catch-up’ growth) and therefore no extra cooking and ingredients were required. F-100 (350ml) is provided once per day to pregnant mothers and twice per day (700ml) to mothers breastfeeding infants under six months of age and severely thin mothers to cover estimated additional energy requirements. Therapeutic treatment is provided to women with severe anaemia as per government guidelines. Many of these mothers also have other signs of underlying illness (such as TB) and are referred to respective wards for treatment.
Obese mothers were provided with counselling on physical exercise and given a recipe book tailored to obesity. Very young mothers were given additional counselling on family planning and very short mothers were counselled on diet and family planning.
Limitations of the study
The present opportunistic study on a reasonable sample size was restricted to anthropometric measurements and anaemia, which precluded use of robust biomarkers of nutritional profile as well as co-morbidities not routinely gathered in NRCs. Furthermore, mothers of children without SAM were not assessed to determine if the maternal anthropometric profile was simply a reflection of all mothers visiting these facilities. This study helped inform the development of a maternal package, using a common-sense approach based on available evidence and feasibility and practicality in the given context. It was not possible to test the effectiveness of the package on nutrition outcomes of mothers.
Discussion
Prevalence of malnutrition was high among mothers of children admitted with complicated SAM; one third of the mothers were malnourished, similar to that found in a multi-centre trial in India (Bhandari et al, 2016). The present study also found a double burden of malnutrition in around one quarter of households, where the child was acutely undernourished and the mother was overweight or obese. Eight per cent of mothers were pregnant and almost half were malnourished, highlighting the need for intervention involving counselling and dietary supplementation as per GoI norms and, looking ahead, to address family planning. This is an important preventive action as a mother being stunted, wasted or underweight preconception or during pregnancy predisposes the unborn child to undernutrition (Bhutta, 2013). The pregnant mother’s stay in the NRC with their admitted child (and non-pregnant mothers) presents an important opportunity to improve the mother’s own nutritional status and that of her future children.
The capacity required to roll out the maternal services package is minimal, given that the programme is operated through existing NRCs, which already have kitchen facilities and adequate human resources for cooking and nutrition counselling. The IFA, calcium supplementation and deworming can be procured from the hospital supply, already funded by the GoI. Additional costs will be incurred in the provision of MUAC tapes and in the extension of the time input by existing nutrition counsellors for group and bedside counselling, which we estimate is possible within current capacity.
Conclusion
In conclusion, facility-based centres for treatment of SAM in children present an opportunity to capture the attention of mothers and target support to them for a duration of at least one to two weeks, to address the maternal double burden of malnutrition, anaemia and family planning practices. Co-morbidities are common among mothers who may be stunted and/or underweight or overweight. More research is needed in similar settings to corroborate this evidence and urgent pilot testing is needed of the proposed service package in NRCs to determine operational feasibility and effectiveness on nutrition outcomes.
Read the maternal malnutrition guideline here.
For more information, please email Vani Sethi.
Endnotes
1Counselling aids are available on request from the authors.
2The composition of F-100 is cow’s milk/toned dairy milk (treated buffalo milk) 315 ml, sugar 26.2g and vegetable oil 7g, which has 350 Kcal, 10.1 g of protein and 14.7 g of lactose.
References
Bhandari N, Mohan SB, Bose A, Iyengar SD, Taneja S, Mazumder S, Pricilla RA, Iyengar K, Sachdev HPS, Mohan VR, Suhalka V, Yoshida S, Martines J, Bahl R. Efficacy of three feeding regimens for home-based management of children with uncomplicated severe acute malnutrition: a randomised trial in India. BMJ Global Health 2016; 1: e000144.
Bhutta ZA. Early nutrition and adult outcomes: pieces of the puzzle. Lancet 2013; 13: 60716-3.
Khadivzadeh T. Mid upper arm and calf circumferences as indicators of nutritional status in women of reproductive age. Eastern Mediterranean Health Journal 2002; 8: 612-618.
Ministry of Health and Family Welfare (MoHFW). Guidelines for Antenatal care and skilled attendance at Birth by ANMs, LHVs/SNs. Government of India. 2010. http://nhm.gov.in/images/pdf/programmes/maternalhealth/guidelines/sba_guidelines_for_skilled_attendance_at_birth.pdf, accessed 28 March 2018.
Ministry of Health and Family Welfare (MoHFW). Guidance document: Nutritional care and support for patients with Tuberculosis In India. Government of India, New Delhi, India. 2017. https://tbcindia.gov.in/WriteReadData/Guidance%20Document%20-%20Nutritional%20Care%20%26%20Support%20for%20TB%20patients%20in%20India.pdf, accessed 22 April 2018.
Ministry of Health and Family Welfare, Government of India. (2011). Operational Guidelines on Facility Based Management of Children with Severe Acute Malnutrition. Accessible from: http://nhm.gov.in/images/pdf/programmes/child-health/guidelines/operational_guidelines_on_fbmc_with_sam.pdf, accessed 18 March 2018.
Nagabhushan BM, Poornima J, Premalatha R. Study of maternal profile in children admitted to nutritional rehabilitation centre at a tertiary hospital. International Journal of Contemporary paediatrics 2017; 4: 1911-1913.
National Family Health Survey (NFHS 4) 2015-16. International Institute of Population Sciences, Mumbai, India. 2016. www.rchiips.org/nfhs/nfhs4.shtml, accessed 14 March 2018.
R, Singh DK. Maternal Profile of Children with Severe Acute Malnutrition. Indian Pediatrics 2015; 52: 344.
World Health Organization (WHO). Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series 854. Geneva: World Health Organization. 1995.
World Health Organization (WHO). Adolescent nutrition: a review of the situation in selected South-East Asian countries. New Delhi: Regional Office of South-East Asia, World Health Organization, World Health Organization 2003; 3–29.
World Health Organization (WHO). Hemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Vitamin and Mineral Nutrition Information System. Geneva, (WHO/NMH/NHD/MNM/11.1). 2011. Available from: www.who.int/vmnis/indicators/Hemoglobin. pdf, accessed 28 September 2017.


