Micronutrient powder distribution strategies to increase coverage and adherence among children aged six to 23 months as part of an IYCF strategy in Cambodia
By Sarah Gibson, Hou Kroeun and Gary Mundy
Sarah Gibson is a public health nutritionist and currently works as an analyst at the Children’s Investment Fund Foundation (CIFF). She holds an MSc in nutrition for global health from the London School of Hygiene and Tropical Medicine.
Hou Kroeun is the Deputy Country Director for Programmes at Helen Keller International Cambodia and the Chairman of the Scaling Up Nutrition Civil Society Alliance (SUN CSA) in Cambodia. He holds a master’s degree in public health and has 20 years of experience in the design and management of integrated household food production and nutrition-related programmes in Cambodia.
Gary Mundy is currently Senior Regional Evaluation Adviser for the British Council in East Asia. He has spent the last 15 years supporting the evaluation and research work of a number of non-governmental organisations in Asia and Africa.
The project described in this article was implemented by Helen Keller International and funded by Irish Aid. The authors would like to thank the Cambodian Ministry of Health for their collaboration and support of this project.
Location: Cambodia
What we know: Micronutrient powder (MNP) distribution improves micronutrient status and reduces anaemia and iron deficiency in children aged six to 23 months.
What this article adds: Helen Keller International (HKI) and the Ministry of Health (MoH) in Cambodia implemented an integrated infant and young child feeding (IYCF)/MNP pilot programme for children aged 6-23 months between 2012 and 2014. Three strategies were used to distribute MNPs and provide MNP and IYCF counselling: community-based volunteers direct to households; collection from health centres (fixed); and a combination of the two (mixed). Results of an endline cross-sectional survey and coverage data (final 11 months) showed significantly higher average coverage for community sites compared to mixed and fixed, and for mixed compared to fixed. Programme adherence and differences in caregiver knowledge were significantly higher for community compared to fixed sites; no significant differences were found between community and mixed. Community-based distribution has the potential to improve coverage of MNP programmes among children age 6 to 23 months in Cambodia: combining community and facility-based distribution may be more feasible and cost-effective.
Background
Micronutrient deficiencies are a major public health challenge in Cambodia. Over half (56%) of children six to 59 months are anaemic, with notably higher prevalence among infants aged nine to 11 months (83%) (National Institute of Statistics, 2014). There are multiple causes of anaemia, including deficiencies in iron and zinc, infection and genetic haemoglobin disorders and, for infants and young children, inadequate dietary intake and poor infant and young child feeding (IYCF) practices (Balarajan et al, 2011). Only 30% of Cambodian children aged six to 23 months receive a minimum acceptable diet and, particularly in rural households, complementary foods tend to lack in quantity, diversity and animal-source foods (National Institute of Statistics, 2014).
Micronutrient powders (MNPs) are a proven home-fortification strategy recommended by the World Health Organization (WHO) to improve micronutrient status and reduce anaemia and iron deficiency in children aged 6 to 23 months (WHO, 2016). The efficacy of large-scale MNP programmes in reducing anaemia in this age group has been clearly demonstrated in various low- and middle-income countries, including Cambodia (WHO, 2016). Despite this, there is a lack of implementation research exploring which distribution strategies are most effective in supporting sustained coverage and adherence to MNPs at scale.
Current global MNP programmes typically use more than one channel of distribution; either facility-based, community-based or market-based (Jefferds et al, 2011). Community-based distribution has been identified as one of the best ways to reach rural populations in resource-limited settings where existing coverage may be chronically low (Micronutrient Forum, 2008). Integrating MNPs into well-established community-based services may provide an increased opportunity for long-term sustainability, a critical component for successful programme scale-up. A recent review of nine global MNP interventions that delivered MNPs at no charge through the national health sector, found that coverage was generally higher when distribution took place at the community level (Reerink et al, 2017).
Helen Keller International (HKI) worked with the Ministry of Health (MoH) in Cambodia to implement an integrated IYCF/MNP pilot programme among children aged 6-23 months of age between 2012 and 2014, with the goal of reducing anaemia in this age group. This post hoc analysis looks at the different distribution strategies employed and their association with coverage, adherence and knowledge to help identify the most effective methods to improve delivery, coverage and use of MNPs in Cambodia.
Methods
Prior to the programme MNPs were available at health centres (HCs), but household usage was low. In response the programme employed three strategies for distributing MNPs to eligible households: (1) Community-based delivery: village health volunteers distributed MNPs directly to households (five operational districts (ODs)); (2) Fixed-site strategy: households within 10 km of an HC collect MNPs from HC (1 OD); (3) Mixed strategy: Households within 5 km of an HC collect MNP from HC staff and households further than 5 km received MNPs from village health volunteers (VHVs) (1 OD).
Data were used from two sources: an endline cross-sectional survey (n=800), conducted after 20 months of MNP distribution (no data were collected on coverage or adherence at baseline as very few households (3%) had previously used MNP before) and monthly coverage data collected over the final 11 months of MNP distribution. The latter reported on monthly coverage estimates across the seven ODs, each covering approximately 50,000-100,000 people with five to 10 HCs (MoH, 2016).
A box containing 15 sachets of MNPs was provided each month to caregivers, along with preparation and feeding instructions. Both VHVs and HC staff were trained to provide standardised messages to participating families. A total of 1,770 VHVs and 404 HC staff were trained to distribute and counsel on MNP use and improved IYCF practices. Mass media spots and counselling sessions provided educational messages with an emphasis on WHO-endorsed complementary feeding practices and continued breastfeeding until two years of age and beyond.
The Cambodian National Nutrition Programme (NNP) recommended that all children aged six to 23 months be allocated 15 sachets of MNPs for consumption on a flexible schedule every month. Coverage was defined as the percentage of children aged six to 23 months who received 15 MNP sachets in the last month. Adherence was defined as the percentage of children aged six to 23 months who consumed all 15 sachets during that time period. In January 2015, after the programme ended, the MoH began to recommend a revised dosage of 10 sachets per month per child, so partial adherence was included in this analysis.
Results
Coverage
Table 1 summarises monthly coverage across each of the three distribution strategies over the final 11 months of distribution. Results showed significantly higher average coverage among the VHV distribution ODs, compared with the mixed distribution OD (73%, 64%; p=<.001), and compared with the OD using fixed-site distribution (73%, 30%; p=<.001). There was also significantly higher average coverage among the mixed distribution OD compared with the fixed-site distribution OD (64%, 30%, p=<.001).
Between January and July 2014 the fixed-site strategy achieved 16% coverage (range: 12-23%; p=.03 for difference in coverage between January and July). After observing higher coverage in the VHV and mixed distribution model, the fixed-site strategy changed to a mixed strategy and coverage increased to 55% over the last four months of the programme (range: 37-66%; p=<.001 for difference in coverage between July and November).
Table 1: MNP coverage (received 15 MNP sachets in the last month) from monitoring data during the final 11 months of programme implementation
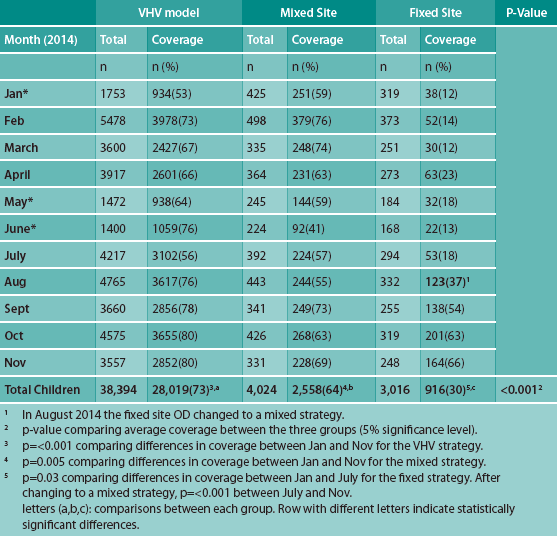
* In January, May and June 2014 MNPs were unavailable in three ODs (using the VHV distribution strategy) because of a disrupted supply, so there are no coverage data from those ODs, resulting in smaller sample sizes during those months. For other months, the total number of children that fell within the 6-23 months age range differed, which also resulted in variations in the number of households monitored each month.
Adherence
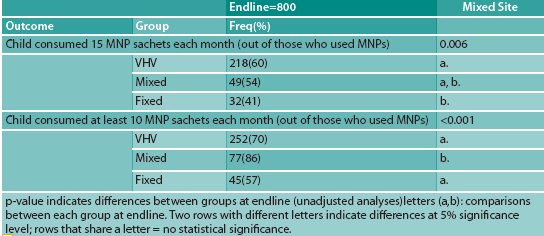
Table 2 summarises adherence estimates collected at endline. There was no significant difference in adherence, as measured by consumption of 15 sachets in the past one month, between VHV-distribution ODs and the mixed-site OD (60%, 54%). There were positive differences in adherence between VHV-distribution ODs and the fixed-site OD (60%, 41%; p=.001), but no significant differences in adherence between the mixed-site and fixed-site ODs (54%, 41%).
When measuring the consumption of 10 sachets in the past month, significantly more respondents in the mixed-site OD reported partial adherence, compared with the VHV-site ODs (86%, 70%; p=.002) and the fixed-site OD (86%, 57%; p=<.001). Differences between the VHV site and the fixed site were not significant. After disaggregating the adherence data in the mixed-site OD, it was found that 90% of those who received MNPs from VHVs consumed at least 10 sachets per month, compared to 79% among households who collected MNPs from HCs. However, this finding was not statistically significant because of the small sample size of the mixed-site OD (n=100).
Table 2: Adherence to MNP across the three distribution strategies at endline
Caregiver Knowledge
Table 3 summarises caregiver knowledge of four promoted benefits of MNP for young children at endline across the three distribution approaches. There were significant and positive differences in knowledge of three out of the four promoted benefits between the VHV and fixed sites: promoting optimal growth (76%, 54%; p=<.001), increasing immunity (35%, 19%; p=.004), and preventing iron deficiency (19%, 7%; p=.01). However, there was no significant difference in knowledge across respondents receiving either VHV distributed MNPs or the mixed model. The fixed-site group was significantly more likely not to know of any benefits of MNPs compared to the VHV (p=<.001) and mixed groups (p=.02).
Table 3: Knowledge of benefits of MNPs among caregivers who had previously used MNPs across the three distribution strategies at endline
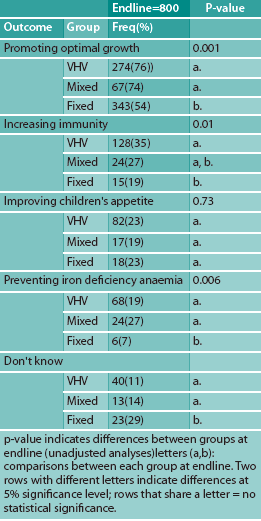
(As only one OD employed a fixed-site strategy and only one OD employed the mixed strategy, sample sizes for these two strategies were much lower than in the VHV strategy at endline (fixed n=100; mixed n=100; VHV n=600).
Discussion
MNP coverage was considerably higher in target ODs where VHVs were responsible for full or partial distribution, compared to the OD using a fixed-site strategy. Full community-based distribution of MNPs by VHVs showed the highest level of coverage. After the fixed-site strategy changed to a mixed model for the final four months of the programme, coverage rates increased rapidly and significantly. These findings suggest that community-based distribution of MNPs using VHVs is more effective than an absolute fixed-site distribution strategy at increasing coverage.
Many different factors can influence intake adherence to MNPs, such as guidance to caregivers, perceived benefits of the product, side effects, administration frequency and distribution model (de Barros et al, 2016). In target ODs where VHVs were responsible for total or partial distribution, children were significantly more likely to consume 15 or at least 10 sachets of MNP each month compared to those in the fixed-site strategy. Similarly, when examining maternal/caregiver knowledge on the benefits of MNPs, it was found that where VHVs were responsible for total or partial MNP distribution, caregivers demonstrated better knowledge than caregivers who collected MNPs from HCs. Lower rates of adherence and knowledge in the fixed-site OD suggest that VHVs may play a unique role in the community as an effective channel of communication linking households to MNPs.
Conclusions
This analysis found that community-based distribution using VHVs is more effective at maximising coverage and promoting adherence to MNPs than fixed-site distribution from health centres. Although VHVs are trusted community members who have been used for decades by non-governmental organisations (NGOs) and government to implement health interventions, they are not formally recognised as part of the healthcare system of the MoH of Cambodia, nor are they permitted to deliver essential drugs. HKI has observed that VHVs operating in areas where NGOs are working tend to be well trained, financially supported, motivated and active. However, when NGOs phase out their support, VHV involvement and engagement often declines. VHVs need consistent and cohesive centralised support from government to ensure the sustainability of a large-scale MNP programme.
Large-scale MNP distribution depends on the ability of governments to plan and budget effectively and their capacity to distribute product and monitor interventions. With time, countries will shift from external, donor-funded to government-financed programmes, so long-term financing is an important consideration, particularly if MNPs are to be distributed free of charge to the end-user. Although an absolute fixed-site distribution strategy is less burdensome on resources, it can only be expected to reach a portion of the target population (approximately one quarter, based on this analysis). Community-based distribution using VHVs will be critical to reach children aged 6 to 23 months in the most vulnerable villages across Cambodia. A mixed strategy of MNP distribution that includes both community-based and facility-based distribution may be a more cost-effective and comprehensive model that can capitalise on existing infrastructure and minimise the risk of overburdening VHVs.
For more information, please contact Sarah Gibson.
References
Balarajan Y, Ramakrishnan U, Ozaltin E, Shankar A, Subramanian S. Anaemia in low-income and middle-income countries. Lancet. 2011;378(9809):2123–35.
de Barros SF, Augusto Cardoso M, Cardoso MA. Adherence to and acceptability of home fortification with vitamins and minerals in children aged 6 to 23 months: a systematic review. BMC Public Health [Internet]. 2016;16(1):1–11. Available from: http://10.0.4.162/s12889-016-2978-0%0Ahttp://search.ebscohost.com/login.aspx?direct=true&db=a9h&AN=114454153&site=ehost-live&scope=site
Jefferds ME, Irizarry L, Timmer A, Tripp K. Unicef-cdc global assessment of home fortification interventions 2011: Current status, new directions, and implications for policy and programmatic guidance. Food Nutr Bull. 2013;34(4):434–43.
Micronutrient Forum Project UM and CB. Scaling Up Micronutrient Programs: What works and what needs more work? The 2008 Innocenti Process. Micronutr Forum. 2008.
Ministry of Health. Kingdom of Cambodia: Health Strategic Plan 2016-2020 [Internet]. Phnom Penh, Cambodia; 2016. Available from: www.nationalplanningcycles.org/sites/default/files/planning_cycle_repository/cambodia/cambodia_nhpsp_2016-2020.pdf
National Institute of Statistics, Directorate General for Health, ICF International. Cambodia Demographic and Health Survey 2014. Phnom Penh, Cambodia and Rockville, Maryland, USA; 2015.
Reerink I, Namaste SM, Poonawala A, Nyhus Dhillon C, Aburto N, Chaudhery D, et al. Experiences and lessons learned for delivery of micronutrient powders interventions. Matern Child Nutr [Internet]. 2017;13(June):e12495. Available from: http://doi.wiley.com/10.1111/mcn.12495
WHO. WHO guideline: Use of multiple micronutrient powders for point-of-use fortification of foods consumed by infants and young children aged 6–23 months and children aged 2–12 years. World Health Organization. 2016. Licence: CC BY-NC-SA 3.0 IGO.


