Nutritional response in north-eastern Nigeria: Approaches to increase service availability in Borno and Yobe States
By Sanjay Kumar Das, Dr Sule Meleh, Dr Umar Chiroma, Bulti Assaye and Maureen L Gallagher
Sanjay Kumar Das is a nutrition manager for UNICEF Maiduguri office for the north-eastern Nigeria response. He is a public health nutritionist with over 15 years’ experience in nutrition programme design, coordination, partnership and resource mobilisation and has worked in Somalia, Kenya, Ethiopia, Sudan, Yemen, Jordan, Pakistan, India and Nepal.
Dr Sule Meleh is Executive Director, Borno State Primary Health Care Development Agency (BSPHCDA), where he oversees the overall management of primary healthcare services in Borno State, north-eastern Nigeria. He previously worked as a senior medical officer in paediatrics for 18 years before taking up a senior leadership position in public health eight years ago.
Dr Umar Chiroma is Deputy Director of Primary Healthcare for Yobe State Primary Health Care Management Board. He is a public health specialist, supervising and managing nutrition response activities in Yobe State. He has eight years’ experience in public health, including nutrition services.
Bulti Assaye is a nutrition officer for UNICEF Abuja office and is responsible for nutrition programme data analysis, information management and reporting.
Maureen L Gallagher is the Chief of Nutrition for UNICEF Afghanistan. She was previously the Nutrition Specialist with UNICEF’s Emergency Response Team based in UNICEF headquarters, when she supported emergencies in Nigeria, Yemen and Democratic Republic of Congo. She is a public health specialist with over 15 years’ experience in nutrition programming in several countries in Africa and Asia.
The authors thank Geoffrey Ijumba, Chief of UNICEF Maiduguri field office, and Dr Simeon Nanama, Nutrition Section Chief of UNICEF Nigeria for reviewing this article and providing strategic guidance and support for the scale-up of the nutrition response in north-eastern Nigeria. The authors would also like to acknowledge the whole nutrition teams of Borno PHCDA, Yobe SPHCMB, UNICEF Maiduguri and Abuja office for their commitment and hard work in the scale-up of the nutrition response in Borno and Yobe states.
The findings, interpretations and conclusions in this article are those of the authors. They do not necessarily represent the views of UNICEF, its executive directors, or the countries that they represent and should not be attributed to them.
Location: Nigeria
What we know: Six years of armed conflict in north-eastern Nigeria have resulted in mass displacement, severe food insecurity and undernutrition, and have destroyed livelihoods and further weakened fragile health systems.
What this article adds: In 2010 UNICEF supported integration of community-based management of acute malnutrition (CMAM) services (SAM treatment) into 75% of fixed health facilities in north-eastern Nigeria. In 2015 infant and young child feeding (IYCF) support and multiple-micronutrient powder (MNP) were added. Government has led scale-up of this integrated package; the number of centres has increased fourfold and the number of children treated has increased fivefold (2013-17). UNICEF has focused on supporting state government to meet immediate needs of severely malnourished children while strengthening the government health system. A minimum nutritional services package was finalised in early 2017. Multiple delivery platforms have been used (fixed health centres, IDP camp nutrition centres, community outreach, mobile services) and community nutrition mobilisers have increased coverage, including in insecure areas. UNICEF has provided financial and technical support, including supervision and monitoring, barrier analysis to poor performing sites, and context-specific supply chain management with roles defined for multiple stakeholders. Financing sources for scale-up have been mixed; some government, some UNICEF-dependent (especially in high humanitarian need states). There has been some success and ongoing advocacy to transition from emergency to development funding sources. Key elements that enabled SAM scale up were strong government leadership with UNICEF support; good communication (especially use of WhatsApp groups); use of existing community platforms for community mobilization; and investment in on-the-job training and supportive supervision.
Background
Before the conflict the situation in Borno and Yobe States was already fragile, with high levels of poverty, underdevelopment, unemployment and inequality. Six years of armed conflict and clashes between government and non-state armed groups (NSAGs) has resulted in millions of people displaced, thousands of lives lost and livelihoods destroyed in north-eastern Nigeria. The prolonged crisis had led to a deterioration in health and other basic services, resulting in increased severe food insecurity and undernutrition. Outbreaks of diseases such as measles, cholera and diarrhoea had also been reported in the area, further aggravating the situation.
More than half of internally displaced persons (IDPs) in north-east Nigeria fled their homes in 2014 and 2015 after NSAGs seized control of a territory covering more than 30,000 square kilometres, committing grave human rights abuses against local populations. A government-led military campaign subsequently saw the government regain control of the area. In 2016 the Nigerian security forces recaptured the main towns and villages of several local government areas (LGAs) and exposed the humanitarian needs of civilians there. Over 250,000 people living in secure ‘satellite’ camps at LGA capitals (including Bama, Dikwa, Monguno and Damboa) were reported in need of emergency assistance. Given the onset of the lean season and rainy season between May and September, the near-term outlook was also grim for the 180,000 food-insecure people in Maiduguri’s outer perimeter and 120,000 Maiduguri camp residents.
Figure 1: Maps of Borno and Yobe state indicating availability of nutrition programme in LGA headquarters and inaccessible area in 2016
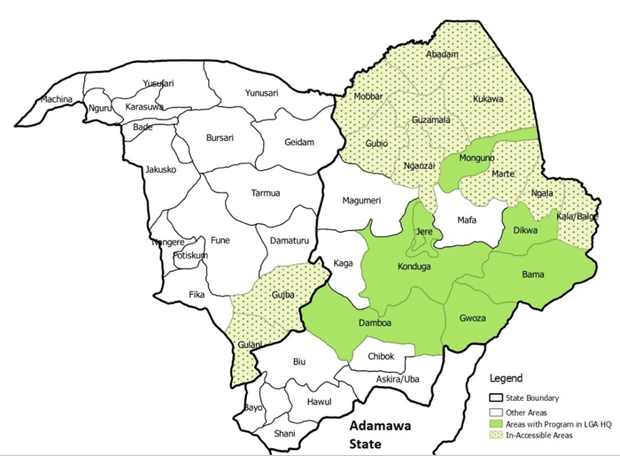
Since 2016 there has been improvement in the access of such communities to life-saving assistance; out of a total 27 LGAs in Borno State, 25 are currently accessible, compared to limited access to 22 LGAs in 2016 (see Figure 1). However, humanitarian access in conflict-affected areas continues to be constrained by restrictions on the movement of aid workers and civilians, especially in Borno State and to some extent Yobe State, as well as ongoing violence and a challenging physical environment (particularly during the rainy season). Borno State clearly remains the epicentre of the humanitarian crisis, with dozens of conflict incidents reported each month. In the crisis affecting north-east Nigeria, nine out of ten displaced persons come from Borno and the State also hosts the majority (78%) of IDPs.
Nutrition situation
The Cadre Harmonisé (CH) analysis1 of March 2018 indicates that an estimated 3.7 million people required emergency assistance between March and May 2018, with 3.9 million being reported as food-insecure. For the projected period of June to August 2018, these figures were expected to increase to about 5.3 million people in the absence of resilience-driven interventions and humanitarian assistance. Only 30% of health facilities are functional in Borno State, where malaria is endemic and cholera and other diseases affect the population regularly and are often life-threatening.
An estimated 943,000 children under five years old across Borno and Yobe States are acutely malnourished; 440,000 with severe acute malnutrition (SAM) and 503,000 with moderate acute malnutrition (MAM). Around 230,000 pregnant and lactating women (PLW) are estimated to be acutely malnourished. The nutrition situation in Borno and Yobe States declined rapidly due to the crisis in 2015, peaked in 2017 and has stabilised in 2018, with some exceptions in hard-to-reach areas (mainly in Damasak, Gubio, Kukawa and northern Yobe). Recent nutrition surveillance (by UNICEF, in collaboration with the National Bureau of Statistics (NBS)) revealed GAM and SAM rates of 6.4% and 1.2% in Borno and 12.0% and 1.3% in Yobe respectively.
Nutrition response scale-up: A combined approach
The nutrition response in north-eastern Nigeria has been driven by the strong political will and leadership of the Ministry of Health (MoH). While public services and institutions have been overstretched, and in some cases destroyed in affected areas, services have continued to function where possible. The emergency nutrition response has been integrated into the existing system, with active participation of key pre-existing stakeholders and therefore provides an example of humanitarian development programming in response to crisis.
UNICEF initiated support to community-based management of acute malnutrition (CMAM) programming in the north-east in 2010 for identification and treatment of children with SAM2. SAM management was integrated in about 75% of fixed health facilities (FHFs) and UNICEF provided training and onsite coaching to enhance the capacity of government health workers and supplied ready-to-use therapeutic food (RUTF) and basic equipment for identification and treatment of SAM children. Infant and young child feeding (IYCF) support and multiple micro-nutrient powder (MNP) supplementation activities were initiated in 2015 after the crisis began. These were integrated into service delivery platforms in health facilities already delivering SAM treatment.
Figure 2 Timeline of major nutrition-related activities in north-eastern Nigeria
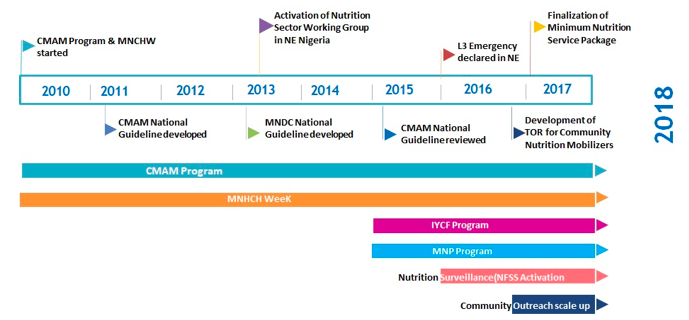
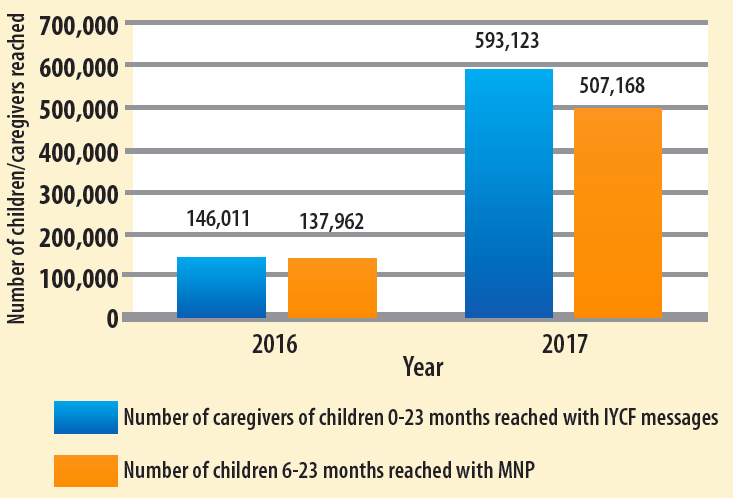
The push to scale up CMAM provision began in 2015 (as described in Figure 2), when the number of fixed health facilities (FHFs) delivering services increased by almost 30%. Scale-up was mainly focused on SAM children (admission based on MUAC <115mm or oedema, discharge MUAC> 125 mm and no oedema), as reflected in the national CMAM guideline that centred on SAM management. Between 2013 and 2017 the number of sites delivering CMAM increased fourfold (from 109 in 2013 to 461 in 2017) and the number of children admitted for SAM treatment increased by over fivefold (from 30,288 in 2013 to 181,170 in 2017) (see Figure 3). At the end of 2017 partners in the Nutrition Sector started to work towards a minimum nutritional services package, which was finalised at the beginning of 2017. This established the premise that all health facilities’ delivery services had to include a minimum package of CMAM, IYCF and MNP services (the latter provided to children aged 6-23 months not affected by SAM or MAM). This significantly increased the coverage of IYCF and MNP services (see Figure 4). The process was led by the Nutrition Sector, with UNICEF participating in the development of an integrated nutrition training package and data tools for health workers and community nutrition mobilisers (CNMs).
The integrated nutrition package approach was placed at the core of the scale-up strategy to increase availability of and access to nutrition services throughout Borno and Yobe States. This was achieved through the use of multiple platforms to deliver the minimum nutrition services package, as summarised in Box 1. Efforts were made by sector partners to strengthen the community-based aspects of the programme through the recruitment and use of CNMs, employed to increase community mobilisation and demand for services (Box 2). In the context of conflict and insecurity, this approach has led to the timely identification and treatment of SAM children, promotion of IYCF practices and appropriate use of MNP at household level. Working with local NGOs to provide CNMs has been beneficial, given their good community network and access at community level with limited security challenges. The new strategy achieved impressive results in terms of increased number of units delivering CMAM services and increased admissions (as illustrated in Figure 2).
Box 1. Approaches implemented by partners to increase availability of nutritional services
Fixed health facilities (FHFs): FHFs are part of the government routine health system in host communities before the crisis. Nutrition services are integrated into FHFs as a component of the primary healthcare package. UNICEF has supported state government to integrate nutrition services (SAM treatment, IYCF support and MNPs) into primary healthcare services in 312 FHFs in Borno and Yobe States.
IDP camp facilities: These are set up temporarily in IDP camps to provide basic health and nutrition services to IDPs after they have arrived in a safe and secure location. IDP camp facilities were first established in 2015 in response to increased numbers of IDPs and the subsequent set-up of the first IDP camp in Borno State. UNICEF has set up 14 nutrition service sites in IDP camps for the provision of integrated nutrition services. UNICEF mobilised health workers displaced to IDP camps to work in the health/nutrition clinics, since they were still paid by government, and offered financial top-ups to motivate them to continue their work.
Community outreach: A community outreach team comprises two skilled people (one CMAM provider and one nutrition screener) for the identification and treatment of SAM children in densely populated areas, mainly in host communities. These teams were launched to reduce overcrowding in FHFs and provide daily nutrition services. Community outreach started in central Borno LGAs (Maiduguri metropolitan city (MMC), Jere, Konduga and Mafa) in 2016 to address the increased IDP influx and increased demand in services. UNICEF, in collaboration with state government, has set up 35 outreach sites from which community outreach teams operate.
Mobile teams: A mobile nutrition team comprises three skilled nutrition personnel (a CMAM provider, a nutrition counsellor and a nutrition screener/recorder). The team moves from one location to another to cover between three and five locations each week for the provision of integrated nutrition services in settlements/communities far away (>3 km) from FHFs. This approach started in August 2017 to increase the availability of nutrition services in remote communities. UNICEF, in collaboration with state government, has so far deployed 49 mobile nutrition teams, often to newly accessible areas where government infrastructures are completely damaged.
Box 2. Community Nutrition Mobilisers (CNM)
CNMs are identified from the local community to strengthen the community mobilisation and sensitisation component of the nutrition programme. Duties include: active house-to-house nutrition screening of all children under five years old (700 to 1,000 children per CNM) and identification and referral of SAM children (ten days per month); follow up SAM children to ensure completion of treatment and appropriate use of RUTF and MNPs (four days per month); formation and facilitation of mother support groups (MSGs) for the protection, promotion and support of IYCF practices (five days per month); and one-to-one support for mothers with breastfeeding problems (three days per month). CMNs refer malnourished children (aged 6-23 months) or MAM children who are not receiving supplementary food for MNP, while SAM children are referred to receive appropriate treatment (RUTF and routine medicine). CNMs are paid and are guided by a terms of reference (TOR) defined and agreed by sector partners.
UNICEF has partnered with three local non-governmental organisations (NGOs) to strengthen community mobilisation activities and ensure timely payment of CNMs. Local partner NGOs provide coaching to and supportive supervision of CNMs through 121 ward-level nutrition supervisors (local NGO staff). Supervisors conduct monthly review meetings between CNMs and FHF nutrition staff to collect monthly reports from CNMs, provide feedback on data quality, discuss challenges and lessons learned, provide monthly incentives to CNMs and plan community mobilisation activities for the subsequent month.
Figure 3: Trends in SAM admissions and scale-up of CMAM service delivery units (SDUs) in Borno and Yobe States 2013-2017
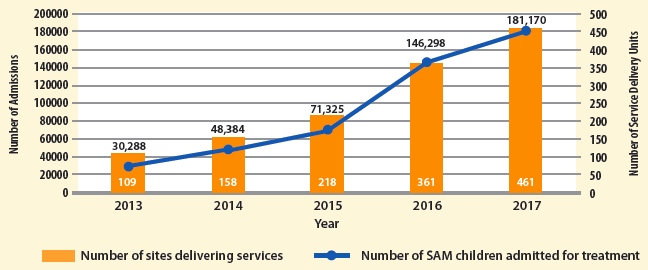
Figure 4: Beneficiaries reached with IYCF support and MNP supplementation in 2016 and 2017
Supervision and monitoring
To address challenges of monitoring in areas of difficult access, UNICEF has a contract with a local institution to deploy skilled personnel to be based at LGA level. Considering the security situation, working through the local institution, personnel can move frequently to and within the LGA. The UNICEF Nutrition section deployed 31 senior nutrition LGA facilitators to provide close monitoring and onsite coaching to nutrition staff at LGA and service delivery site level. They support coordination of nutrition activities at LGA level and provision of onsite coaching to nutrition service providers, as well as collection and compilation of nutrition activity reports together with local government nutrition focal persons. This initiative has been vital to improve quality of services, avoid stock-out issues and strengthen timely reporting.
WhatsApp groups for nutrition were created for communication and regular reporting using mobile coverage from neighbouring countries; coverage of networks within Nigeria was poor. As most of the LGA teams were new to the integrated nutrition response, the platform was also used to discuss technical issues arising in the field and provide remote technical support.
In the beginning of 2017 achievement of nutrition indicators was very low relative to the humanitarian response plan (HRP) target; for example, admission of SAM children reached only 24.4% of target by end of May 2018. The total state target was divided for each LGA and target/achievement ratios were monitored monthly to identify areas with poor achievements and explore the reasons. Those LGAs and FHFs were prioritised to strengthen community mobilisation activities and proper reporting and address related challenges for better programme outcomes. This analysis sensitised the team and encouraged them to take adequate action to ensure all children under five years old are screened on a monthly basis and SAM children are admitted to a nutrition programme.
Supply chain management
Given the multiple stakeholders involved in the nutrition programme, and to overcome access difficulties, a context-specific supply management approach was used to mitigate any stock-outs at SDUs. Responsibilities of the different stakeholders were clearly defined, as follows:
- UNICEF: Responsible for supply provision of outpatient therapeutic programme (OTP) sites of newly liberated areas and south Borno. The UNICEF nutrition staff work with LGA nutrition facilitators to compile RUTF and MNP requirements for the logistics team, who supply to SDUs every two weeks.
- State government central Borno: Responsible for supply provision in FHFs and OTP sites in some LGAs in central Borno (MMC, Jere, Konduga and Mafa) due to state government access in these areas. The State Nutrition Officer (SNO) compiles RUTF and MNP requirements from each LGA, which are reviewed by UNICEF and then supplied by UNICEF Maiduguri logistics team to the government central medical store (CMS), from where they are sent to FHFs bi-weekly and outreach OTP sites weekly. Transport costs are covered by UNICEF.
- International NGOs in Borno: RUTF, R75, F1003, MNP and ReSoMal4 requirements (and quarterly forecasted requirements) are sent monthly to UNICEF Maiduguri office by INGOs with programme cooperation agreements (PCAs) with UNICEF. Once requests are reviewed and released, INGO partners collect supplies from UNICEF Maiduguri warehouse and deliver to the OTP sites they support.
- Yobe: Yobe state primary healthcare management board (YPHCMB) forecasts quarterly supply requirements and UNICEF delivers to CMS. INGOs submit requests for RUTF and MNP with their monthly nutrition programme report to the state nutrition officer, who releases supplies from CMS for delivery by INGOs to SDUs. UNICEF and the SNO visit sites periodically for monitoring. For UNICEF-supported sites, the LAG nutrition focal person collates monthly SDU requirements and shares with the SNO, who arranges delivery in collaboration with UNICEF.
The humanitarian-development nexus
UNICEF’s role in scale-up of services has focused on supporting state government to meet the immediate needs of severely malnourished children while strengthening the government health system. Strong advocacy is carried out with the government to ensure that the provision of nutrition services to the state population continues to be the responsibility of state government. The strong leadership shown by the government and continuous support to governance systems ensures that services are sustainable in the long term.
The support and funding of scale-up of nutritional services is mixed. In some areas it is funded by donors, while in others UNICEF internal funding was used for scale-up where the situation was critical and humanitarian assistance needs very high. In Borno and Yobe, government has not allocated any funds for RUTF as most of their funding is spent on security and safety arrangements; in other states, government has directly procured RUTF supplies. Financing for scale-up has been effected through state government by recruitment of additional staff and capacity building; their payment and operationalisation has been undertaken by state government with guidance and support of UNICEF. There is ongoing advocacy to allocate 1% of the consolidated revenue fund (CRF) for basic healthcare provision fund (BHCPF) as part of Appropriation Act, 2018; nutrition is part of the BHCPF. Some states have already allocated funds, but in Borno and Yobe advocacy has started now through the state committee on food and nutrition (SCFN) in transitioning from an emergency to a development approach.
Community systems are also core to the nexus as the humanitarian response works through CNMs, who are selected from their communities and who are key players in the prevention and treatment of undernutrition. Working through MSGs also strengthens social networks as well as enhancing mothers’ understanding of malnutrition.
Lessons learned and conclusions
The programme demonstrates that it is possible to increase access to treatment of SAM and other nutritional interventions in emergency-affected areas with strong government leadership and UNICEF playing a supportive role in meeting the immediate needs of SAM children whilst strengthening the government health system. Other key elements included the formation and utilisation of existing community platforms (identification of CNMs and MSGs), which was vital for the timely detection and treatment of SAM children and to improve programme coverage. Re-engaging displaced health workers has contributed to the observed achievement in scaling up the response programme and improved quality of SAM treatment services and has provided state governments with a cohort of qualified personnel who can be integrated into the health system to ensure programme sustainability during the transition period.
The effective coordination of partners and detailed gap analysis by the sector helped to identify gap areas for scale-up. This process played a vital role in the rapid expansion of the programme. Subsequent periodic data analysis and feedback helped to identify and address ongoing gaps and issues in a timely way. A context-specific service delivery approach and supply chain management helped to address stock-out issues and create effective programing. The use of WhatsApp allowed for timely reporting and communication, even in areas with poor network coverage.
Investing in strengthening on-the-job training, supportive supervision and feedback has the potential to improve the quality of treatment services. Although the programme overall has met the minimum SPHERE standard (cure rate 87.2%; defaulter rate 9.6%; death rate 0.6%; and non-responder rate 2.6%), maintaining the quality of the programme across all sites while scaling up remains a problem. Disaggregated data reveal variations in quality across the different geographic areas.
For more information, please contact Sanjay Kumar Das.
Endnotes
1The Cadre Harmonisé is the equivalent of the Integrated Phase Classification (IPC) approach used in West Africa.
2UNICEF started to use extended criteria (MUAC<125mm) in August 2017 to admit MAM children in outpatient therapeutic programmes and provided seven sachets of RUTF for one week in some hotspot areas as the nutrition situation was critical, based on nutrition surveillance findings. This has been stopped from 1 April 2018. World Food Programme is doing a blanket supplementary feeding programme (BSFP) for children aged 6-23 months and targeted supplementary feeding program (TSFP) for children aged 24-59 months in some areas.
3F-100 and F-75 (also known as Formula 100 and Formula 75) are therapeutic milk products designed to treat severe malnutrition.
4ReSoMal is used for the preparation of an oral rehydration solution used exclusively to treat severe acute malnutrition. It must be used under medical supervision in therapeutic feeding centres.


