Institutionalising quality of care in inpatient facilities for the management of severe acute malnutrition in India
By Meeta Mathur, Naveen Jain, Shivangi Kaushik and Aakanksha Pandey
Meeta Mathur is Head of Programmes for Action Against Hunger India. She has over 13 years of experience in the field of nutrition and health, working with international non-governmental organisations, government and the private sector. Meeta is a qualified nutritionist with a Masters’ degree in food and nutrition.
Naveen Jain is Mission Director of the National Health Mission, Rajasthan and Secretary of the Medical Health and Family Welfare Department. He has pioneered various e-initiatives, including innovative software for use in malnutrition treatment centres in India and has over 20 awards for piloting technical innovations in the field of governance.
Shivangi Kaushik is a public health professional currently working for Action Against Hunger India. She has a masters’ degree in public health and over seven years’ experience leading nutritional surveys for Action Against Hunger and training government and non-government staff on community-based management of acute malnutrition, infant and young child feeding, nutrition in emergencies programming and SMART survey methodology.
Aakanksha Pandey is the State Programme Manager for Action Against Hunger Rajasthan. She has many years of experience working with the government system, providing technical support in the implementation, assessment, planning and monitoring of health and nutrition programmes. She currently supports the government of Rajasthan in the development and implementation of community-based management of acute malnutrition protocols.
The authors would like to thank Naveen Jain and his team at the Medical Health and Family Welfare Department, Government of Rajasthan, Baran District, for their leadership and dedicated collaboration in this programme.
Location: India
What we know: Comprehensive management of children with severe acute malnutrition (SAM), including psychosocial support for the caregiver and child, improves treatment outcomes.
What this article adds: A pilot study by Action Against Hunger (AAH) India was carried out in Baran, a tribal district of Rajasthan, north India, to improve implementation of government SAM guidelines. This involved staff training (n=32) in nine malnutrition treatment centres (MTCs); the appointment and training of counsellors in five MTCs to provide caregiver and SAM children support (one-to-one counselling and group sessions); and improving water, sanitation and hygiene (WASH) and play/education infrastructure facilities in four MTCs. In counsellor-supported MTCs (1,041 children, 2016-18), performance improved in terms of earlier identification by and referral from the community, increase in mean weight gain, reduction in defaulting rates and greater post-discharge attendance at follow-up. The pilot study shows the potential to improve SAM treatment outcomes through staff capacity and infrastructure development to support operationalising government guidelines. Dedicated staff are necessary to deliver adequate psychosocial support and follow-up. Results have been presented to government and discussions are ongoing about the potential for scale-up.
Introduction
In Rajasthan, north India, 20.4% (1,810,670) of children under five years old are wasted and 7.3% (647,936) are severely wasted (National Family Health Survey (NFHS) 3, 2006). Wasting is particularly prevalent in Baran, a largely tribal and one of the poorest districts of Rajasthan. High prevalence of severe acute malnutrition (SAM) led the Government of Rajasthan to develop malnutrition treatment centres (MTCs) in the state, the first of which was set up in Baran in 2006 and now has the highest number of MTCs. In the Integrated Management of Acute Malnutrition (IMAM) programme children with SAM are referred to an MTC for a required inpatient stay of 14 days or more to meet medical and weight-gain discharge criteria (community-based management for uncomplicated cases is not available). However, most caregivers, especially mothers, find it challenging to be away from home for over two weeks; hence they either refuse to be admitted or leave the centre abruptly against medical advice. Action Against Hunger (AAH) has been working in Baran since 2012, focusing on SAM management by early identification and referral of SAM children to MTCs. Despite efforts by AAH and the government, the proportion of children completing the treatment and rate of follow up post-discharge is low (below 50% for the first follow-up and progressively less for each subsequent follow-up). To address this, AAH carried out a qualitative assessment of MTC services in the district, which subsequently informed a series of pilot interventions (training, building counselling capacity and infrastructure development) in target MTCs. Experiences and findings, particularly related to the counselling intervention, are shared in this article.

Quality assessment of MTCs
At the end of 2015 a qualitative survey was undertaken to assess perceptions of and barriers to access of MTC services. In-depth interviews were carried out with caregivers and frontline workers, while knowledge and skills of MTC staff and quality of MTC infrastructures were assessed. Key barriers identified were resistance from husbands and family members to mothers and children staying in the MTC, caregivers feeling intimated by the hospital setting, and caregivers finding it difficult to stay alone at the MTC without their husbands or family members accompanying them. Many caregivers also complained that they feel bored in the MTC as they have nothing to do. These issues were aggravated by inadequate living conditions at the centres and negative behaviour of some MTC staff, which damaged parental trust and perceptions of quality of public health services. Findings were shared with district and state-level officials and possible solutions were discussed.
Quality improvement of MTCs
Based on the assessment findings, a programme of quality improvement was undertaken by AAH, with the full support of the district health administration in Baran, to improve the quality of nine MTCs in the district. A three-pronged programme was devised to improve community demand and the quality of supply services in MTCs. This involved: (1) training of MTC staff in inpatient management of SAM in all nine MTCs; (2) appointing and training of MTC counsellors from local communities in five selected MTCs (those with the highest caseloads and referrals) to provide caregivers with quality care and supportive counselling; and (3) key infrastructure developments in four MTCs where existing infrastructure was particularly poor to improve the living conditions for caregivers and patients and the general environment. Each of these improvements are described in more detail below, particularly the strengthened counselling capacity, where performance was subsequently measured in pilot MTCs.
Technical support to MTCs
Since 2016 AAH Baran has conducted numerous orientation and refresher trainings for staff of all nine MTCs to build their capacity and acquaint them with new developments in SAM management protocols. Trainings are carried out by AAH staff and a highly experienced AAH paediatrician and include an initial three-day classroom training, followed by regular refresher training and ongoing supportive supervision. Information booklets (such as ‘Operational Guidelines of Malnutrition Treatment Centres’), SAM management protocols and job aids are provided to participants as reference guides and monitoring tools.
Appointing MTC counsellors
Improvements in maternal-child bonding and interaction are the major intended child development outcomes during MTC admission; however, this aspect of SAM management was absent from the MTCs prior to 2016. Government guidelines recommend the appointment of a counsellor in each MTC, but funding to support this position was not available. To fill this gap, AAH appointed and financed MTC counsellors in five MTCs with a view to advocating for these positions to be filled and paid for by the government in future. Recruited counsellors had prior experience of working with women and children and received extensive training on facility-based management of acute malnutrition, maternal and child care practices, early stimulation methods, psychosocial support, counselling and communication skills. (See Box 1 for more details on counsellors’ skillsets and how they work.) MTC counsellors also provided technical guidance and on-the-job practical supervisory support and monitoring through qualified and experienced AAH technical managers.
Box 1: Key roles and skills of MTC counsellors
To optimise their stay in the MTC, counsellors work with caregivers to understand their challenges from a psychosocial perspective, provide emotional support and empower them to care for their own and their child’s nutrition and psychosocial needs. Tribal caregivers travelling long distances to an unfamiliar treatment centre are usually overwhelmed and confused on arrival. MTC counsellors are trained to welcome new admissions, assign them a bed and introduce them to MTC staff and facilities. This helps caregivers settle into the surroundings and establishes trust and confidence in the counsellors. Soon after this, counsellors complete a ‘care practices evaluation’ with the caregiver, using an adapted checklist of items to identify areas of weakness in caregiving behaviours. Based on this preliminary evaluation, counsellors prepare a plan for priority interventions with the caregiver to seek their acceptance, consent and active participation.
Important skills and personal attributes of MTC counsellors are:
- Empathy: ability of the counsellor to comprehend the problems, experiences, thoughts and feelings of caregivers and offer supportive space for expression and self-disclosure that further enhances mutual trust and confidence.
- Congruence and warmth: the ability to act in a way that enables caregivers to feel comfortable in the counselling relationship, receive encouragement to interact and attend to child’s health needs.
- Respect: the ability to be impartial and non-judgmental about tribal caregivers, their family challenges and their social situations, so that mothers feel safe, comfortable and confident.
- Unconditional positive regard: acceptance of the caregivers, irrespective of their caste, class and origin; irrespective of caregiver’s weaknesses, negativity and unfavourable conditions.
- Active listening and assistance: a skill that lets caregivers speak for themselves and identify and accept problems and which empowers them to problem-solve on their own, leading to insight, new learning and sustained behaviour change.
Individually tailored, one-to-one psychosocial support sessions are then organised in response to the plan. MTC counsellors also organise daily group education sessions for mothers on specific topics, repeated every 14 days so that each caregiver receives a complete package of knowledge about maternal care and nutrition during pregnancy; post-natal care and infant-feeding practices; immunisation; sanitation and hygiene practices; cooking demonstrations to improve diet diversity; and the benefits of family planning and related services. These sessions are delivered through games, videos and storytelling via flip charts and caregivers are encouraged to share practical challenges they face and ideas on how these can be tackled.
In addition, MTC counsellors teach caregivers simple relaxation exercises, including yoga and breathing exercises, with the aim of improving the caregiver’s mood and helping to reduce mental stress and physical tension and manage their emotions effectively. MTC counsellors also teach mothers to practice daily baby massage to promote a secure mother-child attachment and support the child’s physical and psychological recovery and development. Visiting fathers are also involved in massage sessions to promote paternal affection and attachment with the baby. Daily hour-long play sessions are also organised to stimulate physical and cognitive development in admitted children and strengthen the relationship between caregiver and child further.
On discharge MTC counsellors motivate and inform caregivers to complete four follow-up visits (every 15 days) to track post-discharge recovery of the child from SAM. Counsellors inform the AAH community mobiliser responsible for the village the child is from of their discharge and ensure that the child receives a nutritionally balanced food basket within 24 hours to prevent a gap in the provision of a nutrient-rich diet. During each follow-up visit the counsellor revises key messages on maternal and child nutrition with the caregiver, answers any queries they have, provides information to address any specific caregiving challenges and motivates the caregiver on the basis of progress achieved.
Improvements in facility infrastructure
Adequate infrastructure supports staff to carry out SAM management protocols successfully, improves staff motivation and provides a healthy environment for admitted children and their caregivers, which aids recovery from SAM and reinforces demand for and utilisation of services by target communities. The assessment identified the critical missing infrastructure to be provided as follows:
Water, sanitation and hygiene (WASH) infrastructure
WASH facilities are closely linked with the management of infections and disease. In public health services in India, budgets are largely allocated to treatment rather than preventive services. Shortfalls identified in four MTCs were non-functioning toilets, no wash basins, no access to safe drinking water (in two MTCs), no availability of warm water and no place for washing (and drying) clothes. In these MTCs (and where MTC counsellors were provided), AAH facilitated the development of adequate WASH infrastructure, including repair of toilets, installation of geysers for round-the-clock provision of hot water for medical use and patient care in winter, wash basins with soap dispensers, laundry facilities for caregivers, and repair of water pipes and water purifiers to ensure a regular supply of safe drinking water for parents and children. Sensitisation of MTC staff, beneficiaries and visitors was also undertaken to ensure proper upkeep and maintenance of these services.
Kitchen utilities
Refrigerators used to store therapeutic milk in each of the MTCs were repaired. At Shahabad MTC caregivers were not offered any food from the facility, which created great distress among caregivers. AAH helped to build a kitchen shed and installed traditional mud stoves to give caregivers a place to cook food of their choice.
Play facilities
The quality improvement intervention aimed to ease the anxiety and stress of hospitalisation on admitted children by making the MTC environment as child-friendly and unintimidating as possible. A play area was designed in each MTC and in hospital wards, equipped with a variety of safe toys and games to support physical stimulation and child development. MTC counsellors support mothers in playing with their children and are taught how to make home-made toys from locally available resources and safe waste materials. Televisions were provided to MTCs to show educational videos related to childcare practices and recreation.
Provision of attendant beds
Patient beds are ordinarily shared by their caregiver. However, most children and caregivers are accompanied by the father or another relative. In the absence of residential facilities, the accompanying adult would usually stay for a day, then leave without the child completing treatment, or would also share the patient’s bed, leading to overcrowding. In response AAH provided side beds with storage facilities in the MTCs to enable fathers to stay too.
Results
MTC quality care outcomes and impacts
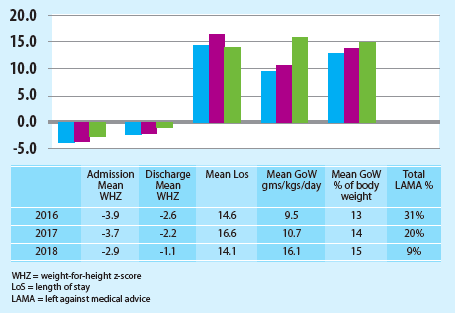
Since their appointment in 2016 MTC counsellors have maintained records of SAM beneficiaries. Training on monitoring was also provided in the four MTCs that did not receive counsellors as part of the general SAM management training, although having a dedicated person to keep records in the MTC counsellors greatly strengthened monitoring activities and the quality of records. Data for five MTCs where counsellors were appointed (Baran, Kishanganj, Relawan, Kelwada and Shahabad) were analysed (see Figure 1). In summary:
- MTC counsellors provided psychosocial support and counselling services to around 33,160 parents and caregivers between 2016 and 2018, including the person accompanying the child for the period of admission and visitors.
- During the project period, 32 MTC personnel, including the MTC in-charge, food demonstrators, cook and auxiliary nurse midwife (ANM)/general nurse midwife (GNM) were trained on protocols on the inpatient management of complicated SAM and nutrition data-monitoring tools. All these staff were continuously provided on-the-job support through AAH-appointed MTC counsellors and the AAH Field Officer.
- Treatment outcomes improved for the 1,041 children treated between 2016 and 2018 in the five counsellor-intervention MTCs. During the two week inpatient treatment of SAM children’s anthropometric growth indicators improved significantly:
- Average mean weight-for-height z-score (WHZ) was higher on admission after the intervention due to earlier identification and referral from the community because of increased confidence in MTC services.
- Average mean difference in WHZ between admission and discharge dropped by 1.5 SD.
- Mean weight gain increased by 6.6 g/kg/day; i.e. by 2% of average body weight gain recorded between admission and discharge.
- Reduction by 22% of cases where caregivers left MTCs against medical advice (LAMA), indicating improvement in caregiver compliance to treatment protocol due to enhanced quality of care. This also ensures the child receives the required treatment, increasing the percentage of recovery and reducing length of recovery.
- Counsellors reported positive outcomes in response to child development support provided to caregivers and children at each facility. This included both caregivers and children engaging and responding positively to baby massage, bathing, play sessions and educational video sessions.
- Improvements in the overall management of MTCs and monitoring were observed.
- Percentage of cases attending all four post-discharge follow-up sessions increased in all MTCs assessed (from 35% to 43% in Baran; 23% to 53% in Kelwada; 19% to 25% in Relawan; 28% to 37% in Shahabad; and 33% to 39% in Kishanghj). This clearly indicates the focus of MTC staff, including the counsellor on post-discharge follow-up. The increase in post-discharge follow-up increases the probability of the child being cured and reduces the recovery period.
Figure 1: MTC outcomes 2016 to 2018
Discussion and conclusions
Non-parametric tests were not performed on the data to test their reliability. However, results seem to suggest that improved performance of the services and treatment outcomes found in this pilot can be attributed to the MTC counsellors and the work of other team members (MTC nurses, feeding demonstrators and cleaning staff), infrastructure improvements leading to improvements in WASH, play and education facilities at each centre, and additional capacity-development activities, such as provision of anthropometry equipment and protocols and training for medical staff. Results indicate the value of investing in both human resource capacity and infrastructure of government MTCs to improve service delivery and SAM treatment outcomes.
A formal assessment of non-counsellor MTCs was not undertaken. However, programming experience is that outcomes for non-counsellor MTCs remain less favourable, including follow-ups happening in under 50% of cases. This reflects a strong need to reinforce post-discharge follow-ups and improve length of stay among the caregivers of SAM children admitted at each facility. While ACF has been building the capacities of MTC staff in captivating caregivers during their stay at MTCs, regular staff are already burdened with record-keeping and day-to-day management of SAM cases, making it difficult to effectively and efficiently deliver all components of a comprehensive service. This experience reinforces the necessity of securing staff who can exclusively deliver on family counselling and related follow-up.
The financial investment per facility is not huge and the potential return on investment high. Findings of the study are being used to advocate with the government for the future appointment of counsellors in all MTCs and the upgrading of MTC infrastructure. As the study was carried out in partnership with the government health department, the results have so far been received well.
The results of this pilot programme show that the addition of dedicated SAM staff at facility level, in addition to existing medical and support staff and structured and thoughtful improvements in infrastructural facilities, can significantly enhance facility performance indicators and improve tribal communities’ confidence, trust and perceptions of treatment services.
For more information please contact Meeta Mathur.


