Implementation of the Expanded Admission Criteria (EAC) for acute malnutrition in Somalia: interim lessons learned
By John Ntambi, Pramila Ghimire, Ciara Hogan, Madina Ali Abdirahman, Dorothy Nabiwemba, Abdiwali Mohamed Mohamud, Abdirizak Osman Hussien, Kheyriya Mohamed Mohamud, Samson Desie, Grainne Moloney, Ezatullah Majeed.
John Ntambi is the Nutrition Manager for UNICEF Somalia. He is a medical doctor with a Master’s in Public Health and Nutrition and over 15 years’ experience working in health and nutrition programmes in Uganda, Rwanda, Eswatini, Chad, Burkina Faso, Côte d’Ivoire, Ethiopia, Burundi and (currently) Somalia.
Pramila is the Head of Nutrition and School Meals for World Food Progamme (WFP) Somalia. Pramila holds Master’s degrees in Public Health Nutrition, Sociology, and Business Administration and has over 18 years’ experience working in food security and nutrition both in development and emergency settings.
Ciara Hogan is a registered dietitian working in the UNICEF Somalia Nutrition Section. Prior to joining UNICEF, she worked with Concern Worldwide in Niger. Ciara holds a Master’s in Nutrition for Global Health from the London School of Hygiene and Tropical Medicine.
Madina Ali Abdirahman is a Nutrition Officer with UNICEF Somalia with over 15 years’ experience in nutrition with UNICEF and non-governmental organisations (NGOs) in Somalia.
Dorothy Nabiwemba is a Nutrition Officer with UNICEF Somalia. She previously worked with the United Nations World Food Programme (WFP) in South Sudan as a nutrition analyst and nutrition scale-up coordinator. Dorothy is a nutritionist and holds a Master’s in Public Health.
Abdiwali Mohamed Mohamud is UNICEF’s Integrated Management Of Acute Malnutrition/Resilience Officer, based in Dollow, Somali, providing technical and operational support to government counterparts and NGO partners.
Abdirizak Osman Hussein has worked with UNICEF Somalia for 16 years and is currently a Nutrition Programme Officer in Baidoa office. He has more than 28 years of experience in nutrition and public health with UN agencies and NGOs.
Kheyriya Mohamed Mohamud is Head of the Nutrition Unit in the Department of Public Health in the Federal Ministry of Health in Somalia. She is a public health professional with a Master’s in Public Health and a post-graduate Diploma in Human Nutrition and Dietetics.
Samson Desie is a nutrition specialist currently working as Nutrition Cluster Coordinator in Somalia with UNICEF. He has over 10 years’ experience in managing large-scale and complex programmes, including in South Sudan and Sudan.
Grainne Moloney has worked for the last 18 years in the development sector, 15 of those with the UN. She currently works as Regional Nutrition Specialist for Emergencies and Severe Acute Malnutrition Scale-up with UNICEF Eastern and Southern Africa Regional Office.
Sayed Ezatullah Majeed is Chief of Field Office for UNICEF Somalia with previous experience working for UNICEF in Afghanistan, Democratic People’s Republic of Korea, Sudan, Eritrea, Sri Lanka and for the Ministry of Health in Afghanistan. Majeed is a medical doctor with a Master’s in Strategic Planning and a post-graduate Diploma in Nutrition.
The authors thank the donors of this programme, including European Civil Protection and Humanitarian Aid Operations (ECHO), Office of United States Foreign Disaster Assistance (OFDA), China, USAID Food for Peace and the UK Department for International Development (DFID).
The findings, interpretations and conclusions in this article are those of the authors. They do not necessarily represent the views of UNICEF, its executive directors or the countries they represent and should not be attributed to them.
Location: Somalia
What we know: Somalia is characterised by persistently high wasting prevalence and insecurity that often constrains access to treatment.
What this article adds: In drought-affected, insecure districts of Somalia, gap analysis by the Nutrition Cluster in 2017 showed seven drought-affected areas had treatment services for severe acute malnutrition (SAM), but none for moderate acute malnutrition (MAM). As an exceptional measure, UNICEF implemented an expanded admission criteria (EAC), combining SAM and MAM treatment (using a ready-to-use therapeutic food (RUTF) product for all), implemented in seven districts by 11 partners. Operational challenges included low local partner capacity (reflected in inconsistent delivery of the protocol and limited monitoring data), challenges in RUTF supply delivery, and poor population access to primary healthcare. Coverage of global acute malnutrition caseload increased to 53%. Performance met Sphere standards for six partners with adequate data. Key ongoing actions include capacity strengthening of partners, increased quality assurance and monitoring, and cost analysis for this fragile, operationally challenging context.
Context
The nutrition situation in Somalia is characterised by a persistently high prevalence of wasting, with global acute malnutrition (GAM) >10% and pockets of GAM above the World Health Organization (WHO) emergency threshold (>15%). Over the past 12 years, GAM prevalence has never been below 10% (Figure 1).
Figure 1: GAM and SAM trends in Somalia 2007-2018
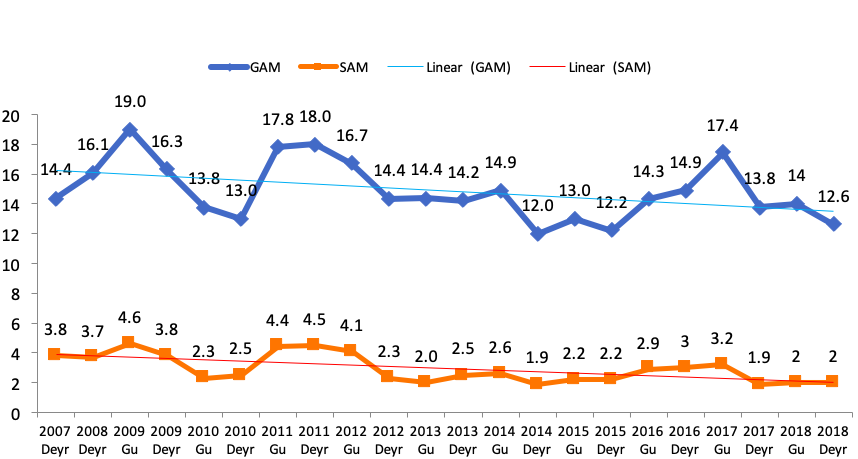
Key drivers of wasting in Somalia include: food insecurity; high morbidity (partly due to limited access to basic social services such as healthcare and adequate water, sanitation and hygiene (WASH)); conflict; climatic shocks; and underlying factors such as weak governance, marginalisation and inequality. Humanitarian access to deliver services to communities living in hard-to-reach areas, often controlled by non-state actors, is constrained. At the peak of the 2017 drought response, cluster mapping reported districts with partial or total absence of lifesaving nutrition services, largely due to security constraints in areas partially controlled by non-state actors. Seven districts in the central south regions of Somalia had operational outpatient therapeutic programmes (OTPs) for the management of severe acute malnutrition (SAM), but no targeted supplementary feeding programmes (TSFPs) for the management of moderate acute malnutrition (MAM). This is in part explained by a policy that requires operational TSFPs to be accessible either to World Food Programme (WFP) staff or to WFP-assigned third-party monitors (TPMs) to conduct monthly programme monitoring and supervision. Expanded admission criteria (EAC) districts are not accessible to UNICEF staff in the same way; however, as a provider of last resort, UNICEF can contract TPMs to visit implementing sites quarterly to assess service quality and provide a degree of programme oversight. This system mitigates staff risk while enabling UNICEF to deliver on the humanitarian imperative.
Rationale for adopting the EAC
In late 2017 UNICEF and WFP agreed to apply a practice outlined in a 2011 memorandum of understanding (MoU)1 to treat MAM with ready-to-use therapeutic food (RUTF) in the absence of TSFPs in districts where UNICEF has operational presence. EAC practice is consistent with the lifesaving agenda of the Humanitarian Response Plan (HRP) and is outlined in the Global Nutrition Cluster (GNC) interim operational guidance on MAM2 and interim operational guidance for community-based management of acute malnutrition (CMAM) programming in exceptional circumstances.3 Guided by these documents, country-level consensus was developed and joint UNICEF and WFP guidance formulated to aid the operationalisation of the EAC into OTPs in Somalia by non-governmental organisation (NGO) partners.

EAC implementation process
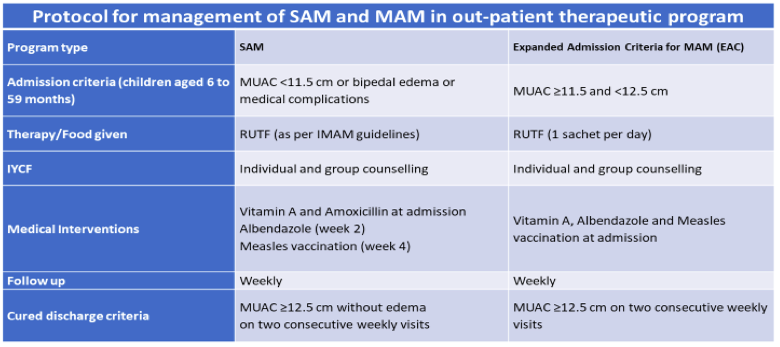
The Somali Cluster Rationalization Plan III, currently under development by the Ministry of Health (MoH), will advise that OTPs and TSFPs operate ‘under the same roof’, using the same implementing partner. This approach, and that of the EAC, intends that SAM and MAM cases are treated in the same facility, ensuring access to treatment services for acute malnutrition while drawing on the same resources, to minimise overheads and operational costs, simplify organisational structures and enable a better flow of patients from one service to the other. Under this protocol (described in Table 1), both SAM and MAM children receive all minimum elements of the basic nutrition services package, including immunisation, deworming, vitamin A supplementation and infant and young child feeding (IYCF) counselling. MAM children receive a weekly ration of one sachet of RUTF/day until discharge at MUAC ≥12.5cm, while uncomplicated SAM care and treatment continues to follow existing Somali national integrated management of acute malnutrition (IMAM) guidelines. Given the absence of stabilisation centres in these hardest-to-reach areas, children with SAM with complications are referred to stabilisation centres in accessible districts.
Exit strategy
The implementation of the EAC is a temporary strategy to save lives in specified areas as agreed by the Nutrition Cluster, WFP, UNICEF and the MoH. When the security situation improves and the specified locations become accessible for programme implementation and monitoring, EAC implementation will cease and the management of MAM will be transferred to WFP. Additionally, EAC may only continue for as long as implementing partners have access to the specified areas and the risk of loss of UNICEF resources can be mitigated.
Table 1: Protocol for the management of SAM and MAM under the EAC
EAC timeline for rollout
The timeline of activities in the adoption of the EAC approach are outlined in figure 2 below.
Figure 2: EAC timeline for rollout
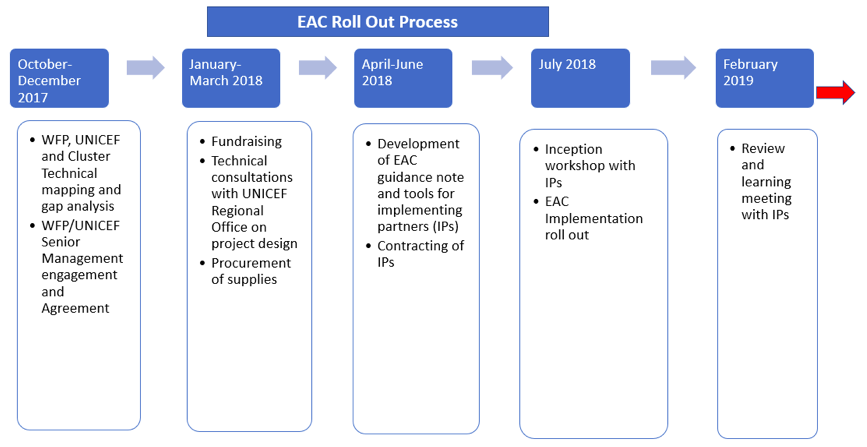
The process began organically with a gap analysis during the last quarter of 2017 which mapped the distribution of existing services across the country. Following learnings from this analysis, WFP and UNICEF came together to reach agreement on adopting the EAC approach in districts without MAM treatment but in the presence of OTPs. MoH, UNICEF and WFP agreed the following district selection criteria: malnutrition rate above emergency threshold; WFP unable to support programme implementation due to their internal policy on access. Fundraising was sought in the first quarter of 2018 and the UNICEF Regional Office was consulted on the technical design of the project. Guidance was developed in the second quarter of 2018 with input from WFP, the Nutrition Cluster and MoH. Following a positive donor response, 10 implementing partners from across the seven EAC districts were subsequently selected to deliver the EAC, based on their existing presence and technical capacity to offer MAM and SAM services. Caseload estimations were derived from the food security and nutrition assessment unit (FSNAU4) seasonal prevalence estimates.
In July 2018, all 10 partners were brought together in an inception workshop where the technical approach was outlined by UNICEF and programme expectations agreed. Programme documents were then signed and, from August onwards, on receipt of supplies, partners began programme rollout. Another district, where accessibility had deteriorated due to security concerns, was identified by WFP for the EAC in December 2018. An international NGO was contracted to take up the caseload in this district; implementation began from March 2019. Eleven partners are therefore now implementing EAC across eight districts in the central south regions of Somalia, including Hiran, Bay, Galgaduug, Lower Juba and Bakool regions.
Implementation experiences
Although it is still too early to fully understand the operational implications of the EAC approach and factors affecting its effectiveness and sustainability, an initial review and learning workshop took place in early February 2019 to analyse emerging data and discuss strengths and challenges of the approach so far. Nine partners participated in the workshop, including eight local and one international NGO, with participation and support from UNICEF, WFP, the Nutrition Cluster and MoH. This was the first time the partners came together to share their experiences of implementation and the first opportunity UNICEF had to understand the practical realities of rollout on the ground. The following sections outline learnings from the different perspectives, informed by the February workshop.
UNICEF’s experience
Somalia is a particularly complex and difficult context in which to operationalise the EAC. Districts selected for the EAC were chosen due to their elevated levels of malnutrition, limited accessibility and security risks relative to other parts of the country. It follows that the global capacity of implementing partners is limited and the ability to attract highly skilled staff to these areas is greatly reduced. TPMs, like partners, often lack the technical expertise to oversee and assess the quality of services of this innovative approach.
Overall, implementing partners appear to face challenges of adherence to the EAC protocol, as evidenced by varying treatment outcomes across partners such as length of stay and amount of RUTF required to cure one case of MAM. Thus, resources are required to build partner capacity, hold training workshops and ensure adherence to the treatment protocol.
Despite challenges, children who were previously inaccessible are now able to receive lifesaving treatment. Furthermore, the EAC has the potential to provide a platform for the expansion of a package of integrated services in some districts. However, there are questions which could not be answered in the February 2019 review workshop that will remain a focus for future review meetings. Such questions include the level of human resources changes or adaptations required to implement EAC, the actual cost per MAM case treated, and the supply-chain management capacity of partners to prevent leakage of RUTF in these hard-to-access areas.
Partner’s experience
A key barrier to EAC implementation was maintenance of the RUTF supply pipeline, which was often disrupted by precarious road transport. As a result, some partners reported a mismatch between the estimated caseloads in their catchment areas and allocated supplies. Other partners discussed challenges in meeting the overall primary healthcare needs of the local community, such as the fact that services for routine vitamin A supplementation, malaria treatment, and treatment for diarrhoea and deworming were not currently available. Follow-up of cases also posed problems due to population movement in some districts in search of pasture and water for livestock. Finally, community health workers were described by some partners as lacking key skills to complement service delivery, while the increased caseload reported by some partners increases the burden on health facility staff.
Key achievements identified by partners included the ability to reach children who previously had no access to lifesaving services, the positive response of the community to the service, and consistent MAM cases in excess of SAM cases, which is thought to reflect good community awareness of service availability and uptake.

Data analysis and outcomes
During the workshop, data from the initiation of implementation (ranging from August to October 2018) to January 2019 was extracted from various sources, including OTP registers and monthly OTP reports (with data disaggregated for OTP and MAM admissions); RUTF stock cards; individual OTP follow-up cards; and copies of quarterly reports submitted to UNICEF.
Key data were summarised in Excel tables in small working groups, guided by UNICEF and WFP staff, including details of SAM and MAM admissions and outcomes, RUTF use and estimated length of stay.
Following the workshop, data from all partners were compiled and analysed. Results revealed significant differences in completeness of data, with only two of the nine partners having comprehensive data across all domains, reflecting the significant constraints of the context. Taking into account these limitations, key findings from the data analysis include:
- As of January 2019, almost 11,000 children were treated for acute malnutrition from a projected caseload of 20,615 children (53% coverage) over six months. Of these, 30% (2,398) were SAM cases (70% coverage) and 70% (8,559) were MAM cases (50% coverage) who previously had no access to services.
- Discharge information for six partners revealed that outcomes consistently met SPHERE standards for MAM programmes of deaths <3%, defaulters <15% and cured cases >75% (Figure 4).
- Data from four partners showed that one carton of RUTF was required to treat 2.9 (range 1.0- 5.37) children with MAM and 0.97 (range 0.22 - 2.0) children with SAM. For SAM, the average is in line with the national guideline, whereas for MAM this is almost double the projected 1.67 children served per carton. Performance data appeared not to be affected by considerable variation in RUTF quantities used by partners, but this requires closer monitoring and examination.
- Data from three partners revealed an average length of stay for children discharged as cured of 7.6 weeks for MAM (minimum 4 weeks, maximum 9 weeks) and 7.3 weeks for SAM (minimum 5 weeks, maximum 13 weeks).
Figure 3: Total MAM and SAM cases treated, August 2018-January 2019
Figure 4: Discharge outcomes of the EAC programme, August 2018-January 2019

Discussion and next steps
There is growing global interest in the continuum of care and the development of a combined/simplified protocol for MAM and SAM treatment, with research ongoing in several countries in Africa. Modalities employed in this approach vary from context to context. In our experience, there is no ‘one-size-fits-all’ solution or model. Somalia is embarking on a learning process and we hope, in time, to increase our understanding of the viability and effectiveness of the EAC approach in this emergency setting.
Interim lessons show that the capacity of partners needs to be strengthened in order to deliver the EAC consistent with the protocol. To do this, regular performance-review meetings and information sharing must take place. Quarterly reviews and regular analysis and interpretation of data will enable timely identification of challenges and continual improvement of the quality of care for patients, as well as the drawing of hypotheses on the effectiveness of the approach. Increased support to TPMs through closer oversight of implementation and quality control through site visits is also warranted. Operating in a fragile context like Somalia bears a higher cost than in more stable settings. This effect is compounded in hardest-to-reach areas and may have an impact on the longevity of this approach. Protection issues should also be considered; mothers come long distances to seek services that may expose them to risks in areas that have limited service provision of any kind. In the future, we hope to undertake an analysis of costs, comparing the EAC model versus ‘business as usual’ to help inform the development of an appropriate model adapted to the Somalia context.
The key next steps include:
- UNICEF to provide further support to implementing partners to improve capacity through quarterly performance-review meetings.
- UNICEF to build capacity of TPMs to monitor and report EAC activities.
- Partners and UNICEF to continue implementation and participate in monthly reporting for quality assurance and analysis.
- UNICEF to further build the capacity of partners in key areas, including preparation of activity reports, caseload estimation, RUTF supply planning and compliance with the protocol.
- UNICEF to advocate in the Health Cluster for the incorporation of certain primary healthcare elements, such as immunisation and the treatment of diarrhea, into the approach.
- UNICEF and WFP to advocate for funding to include support for malnourished pregnant and lactating women in the expanded criteria.
- UNICEF, WFP, MoH and partners to develop a single EAC protocol adapted to the Somali context to be triggered during emergencies or periods of limited accessibility
For more information, please contact John Ntambi.
Endnotes
1MOU WFP-UNICEF: Areas of Technical Cooperation – March 2011. http://nutritioncluster.net/resources/mou-wfp-unicef-march-2011/ last accessed 30 November 2018.
2Global Nutrition Cluster (2017) Moderate acute malnutrition: a decision-tool for emergencies. Global Nutrition cluster MAM Task Force, updated March 2017.
3Interim operational guidance for CMAM programming in exceptional circumstances; http://nutritioncluster.net/interim-operational-guidance-cmam-programming-exceptional-circumstances/
4Food Security and Nutrition Assessment Unit of the United Nations Food and Agriculture Organization: www.fsnau.org/



