OptiMA study in Burkina Faso: Emerging findings and additional insights
By Kevin PQ Phelan
Kevin PQ Phelan is Nutrition Advisor at ALIMA, the Alliance for International Medical Action based in Paris. Before joining ALIMA he worked for Médecins Sans Frontières (MSF)/Doctors Without Borders for more than a decade in various roles, from crisis communications to Nutrition Working Group Leader.
The OptiMA-Burkina Faso study was funded by European Union humanitarian aid funds, the US Agency for International Development and the Médecins Sans Frontières Foundation.
Location: Burkina Faso
What we know: Different protocols, products and coordination mechanisms are typically used for the care of severe acute malnutrition (SAM) and moderate acute malnutrition (MAM) that limit continuity of care for a continuum condition.
What this article adds: ALIMA’s Optimizing treatment for acute MAlnutrition (OptiMA) is a simplified approach to current case management of acute malnutrition based on existing and emerging evidence. It centres on family MUAC (home screening by mothers/caregivers), single admission criteria (MUAC < 125mm and/or oedema), single treatment product (ready-to-use therapeutic food (RUTF)) and rationalisation of RUTF doses according to the degree of wasting. A pilot study (2016-2018) tested this new protocol against a control (standard care) in 54 health centres in one district of Burkina Faso; 5,000 children were enrolled. Prevalence of concurrent stunting was high (42%) and associated with the degree of wasting. Full results will be published shortly. Further research is planned in Democratic Republic of Congo, Niger and Mali. More randomised control trials are needed to test the effectiveness of RUTF dose reductions, the ‘safety’ of excluding children with MUAC > 125mm but WHZ <-2, and gender-specific MUAC thresholds. Observational studies are also needed in multiple contexts using high-quality programme data.
Background
Current standard practice for community management of acute malnutrition (CMAM) is guided by the 2008 United Nations (UN) Joint Statement and subsequent generic protocols that, in theory, integrate severe acute malnutrition (SAM) and moderate acute malnutrition (MAM) care. However, limitations to the current approach have been evident for years: SAM and MAM care use different protocols and different products, and different UN agencies support country-level efforts for the same continuum condition. Often treatment is only available for SAM children, resulting in lives lost and costly hospitalisation that could be averted if nutritional support was available earlier in the wasting process. Gains in numbers of children treated for both conditions have stalled since 2015.
Participants at a UN agency workshop in Dakar 2017 (ACF et al, 2017) identified several barriers to reaching more children, including high costs and caseloads, weak governance, limited human resources capacity, parallel information systems with poor quality data, and complicated supply chains resulting in stock-outs. In addition, SAM and MAM programmes are chronically underfunded. A 2016 World Bank report estimated it would take an additional USD900 million per year globally to mitigate wasting at the scale required (Shekar et al, 2017). The key costs in CMAM are health workers’ time and ready-to-use therapeutic foods (RUTF) for SAM, and ready-to-use supplementary food (RUSF) for MAM. Thus, programmes that make efficient use of health workers’ time and apply intelligent targeting of one product (RUTF) in a single protocol may overcome many of the identified barriers.
Because of these challenges inherent in the current MAM/SAM approach, many organisations have been looking at alternative, simplified protocols. ALIMA’s Optimizing treatment for acute MAlnutrition (OptiMA) is one such strategy, proposing three main changes to current protocols:
1. Earlier detection by training mothers and caregivers how to use mid-upper arm circumference (MUAC) bands to screen children regularly for malnutrition in the home (i.e., family MUAC.)
2. Simplification and easier management by using only one anthropometric measure (MUAC <125 mm (and/or oedema)) for admissions and one product (RUTF) for treatment.
3. More intelligent use of the costliest input (RUTF) by gradually reducing the dosage based on a child’s MUAC status and weight to increase the number of children with access to treatment at no extra or similar cost.

Justification
There is a growing body of evidence for each of these three elements. ALIMA was the first organisation to show that mothers can screen for malnutrition after being trained to use MUAC bracelets on their own children (Blackwell et al, 2015), and that this can increase early detection and reduce hospitalisations at a lower overall cost when brought to scale (Alé et al, 2016). There have been promising results from programmes that only use MUAC criteria for admissions, management, and discharge (such as Binns et al, 2016). Furthermore, in different contexts, it has been shown that MUAC gain parallels weight gain; both are very rapid in the first weeks of SAM treatment, before reaching a plateau (Goossens et al, 2015). This trend is similar in MAM children (Fabiansen et al, 2015). A reduced RUTF-dosing regimen in Myanmar achieved results exceeding the Sphere standards (Philip et al, 2015).
Under OptiMA, the diagnosis of acute malnutrition is refined to targeting treatment to children with a MUAC < 125 mm or oedema. The simplicity of the MUAC measure allows families to screen children and check for oedema at home and identify malnourished children on a regular basis (Alé et al, 2016). The diagnosis is quickly confirmed by clinicians at the health centre. MUAC progression is also used to monitor recovery and determine discharge, thus eliminating the discrepancies that occur when both MUAC and WHZ are used to diagnose acute malnutrition. One of the characteristics of MUAC is that it selects stunted children, and recent research shows how concurrently wasted and stunted children are at a very high risk of death (Myatt et al, 2018); therefore devising strategies that broaden inclusion criteria to encompass these children is important for reducing malnutrition-related mortality. Arguably, a single protocol may be the most practical way to reach these children. Second, RUTF dosage is rationalised and calibrated to the child’s degree of wasting. The WHZ tables and dosing tables are replaced by a single table that determines the child’s RUTF ration based on MUAC category and weight. Larger rations, on a per kilo basis, are given to the most severely malnourished and the ration is reduced as the child progresses to recovery. Third, supply chain is simplified to a single RUTF and data management from two programmes are merged into one. This streamlined programme should result in better coverage, a high proportion of children detected before MUAC <115 mm, lower RUTF consumption per child, and fewer acute malnutrition-related hospitalisations.
Furthermore, data from recent randomised nutrition trials in Niger (Isanaka et al, 2015) and Burkina Faso (Cichon et al, 2016) demonstrate significant morbidity in children with MUAC ≥115mm. In Niger there was no difference in the prevalence of clinical complications among children with MUAC <115 mm and those with MUAC ≥115 and WHZ <-3. In the TreatFOOD trial in children with MAM (MUAC 115-124 mm or -3 < WHZ <-2), 70% of children had a clinical condition identified on admission to the supplementary feeding study. This suggests that a large proportion of children with MUAC 115-124 mm and often classified as moderately malnourished may benefit from the more thorough medical evaluation provided in current SAM programmes.
One published study demonstrates the promise of a MUAC-based simplified protocol. Maust et al (2015) in Sierra Leone achieved >80% recovery in children managed with a MUAC-based, reduced dose RUTF-regimen integrated protocol, compared to 79% recovery in standard treatment. The ComPAS study is a randomised control trial (RCT) comparing a similar protocol to current standard practice (Bailey et al, 2018) (summarised in this issue of Field Exchange and due for peer review publication in 2019).
OptiMA is one of several recent trials seeking to simplify and streamline nutrition protocols and directly address research gaps. In Minding the Undernutrition Evidence Gap, experts identified “the need for further simplifying protocols” and treatment of MAM as two priorities (ECF, 2018). The Humanitarian Health Evidence Review by the London School of Hygiene and Tropical Medicine concluded that early detection of SAM should be prioritised (Blanchet et al, 2015). The Research Agenda for Acute Malnutrition launched by the Council of Research and Technical Advice (CORTASAM) and convened by the No Wasted Lives Initiative identified “the appropriate entry and discharge criteria for treatment of acute malnutrition” and “investigating the safety, effectiveness and cost-effectiveness of reduced dosage ready-to-use therapeutic food dosages” as key research priorities (No Wasted Lives, 2018).
OptiMA-Burkina Faso
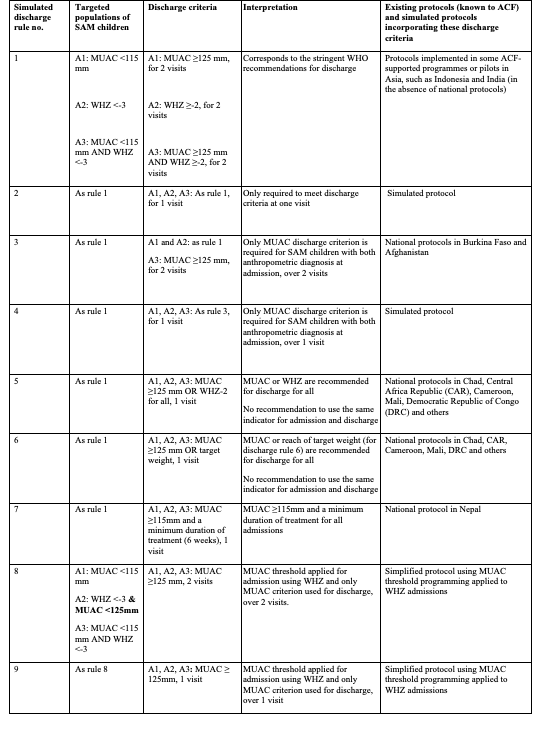
In 2016 ALIMA and its Burkinabe partners Keoogo and SOS Médecins, in partnership with the Ministry of Health (MoH), designed the protocol for OptiMA-Burkina Faso as a pilot trial against external control (i.e., national Burkinabe and international Sphere standards). Figure 1 shows the differences between the current Burkina Faso protocol and OptiMA. Figure 2 shows the reduced-dosage table, which addresses the current dosing paradox in which children receive more RUTF at the end of treatment, even after their weight has plateaued.
Figure 1. Differences between OptiMA-Burkina Faso and the current Burkina Faso protocols for management of acute malnutrition.

Figure 2: OptiMA-Burkina Faso RUTF dosage table compared to the current Burkina Faso PCIMA dosage
The study was conducted in all 54 health centres in Burkina Faso’s Yako district, in the north region, from January 2017 to March 2018 and was implemented by MoH clinical staff. Research staff supervised and monitored data collection, from which an individual database was created. A separate study was conducted to determine rates of relapse at three months post-recovery.
Nearly 5,000 children were admitted under OptiMA and will be included for analysis. A small number of children presented with MUAC >=125 mm and a WHZ <-3; they were treated under the current Burkina Faso SAM protocol. As anticipated in a MUAC-based strategy, prevalence of concurrent stunting was high overall at 42% of children treated under OptiMA, with a positive correlation between levels of stunting and wasting: i.e., 56% for those with MUAC <115 mm at admission; 46% for those with MUAC 115-119 mm; and 37% for those with MUAC 120-124 mm.
Discussion and next steps
Full results of the OptiMA-Burkina Faso pilot will be available in the next few months in a peer-reviewed publication and will be summarised in Field Exchange. ALIMA also hopes to share programme lessons in a future issue of Field Exchange. Regardless of the positive results from Maust et al (2015) and similar forthcoming results from OptiMA- Burkina Faso, it is important to clearly understand the questions that must still be addressed. We need RCTs to determine whether modest RUTF dose reductions (i.e., 150 kcal/kg/d) are non-inferior to current dosage regimens (175-200 kcal/kg/d) for children who present with MUAC < 115 mm or oedema. Second, we need RCTs to learn whether it is ‘safe’ to exclude children with MUAC > 125 mm but WHZ <-2 (children who are currently CMAM eligible but would not be eligible in a MUAC < 125 mm threshold programme). Third, MUAC consistently selects more girls than boys, although there is no reason to believe that girls in sub-Saharan Africa are more affected by acute malnutrition than boys; thus, RCTs are also needed to investigate gender-specific MUAC thresholds to see if gender balance in MUAC-based programming can be improved. Most importantly, given the highly context-dependent aspects of nutrition programming, more observational studies are needed in more places. This means investing in high-quality programme data collection that allows for creation of individualised, monitored databases for thousands of children in multiple countries in east, central and west Africa and in places with high HIV prevalence or significant burden of kwashiorkor.
ALIMA and its national partners have two RCTs and two operational pilots already in the works. The OptiMA-DRC trial, an individual RCT that will begin in 2019, will determine how well this strategy works in a region with a high prevalence of oedematous malnutrition. OptiMA-Niger, first as a small-scale operational pilot and then as an individually randomised control trial, will provide crucial evidence on simplified programming in an area of very high incidence of both wasting and stunting. And OptiMA-Bamako in Mali will test the approach in an urban setting.
With the results from OptiMA-Burkina Faso and these upcoming OptiMA trials, ALIMA hopes to help fill in several research gaps in the coming years and contribute to improved management of acute malnutrition, so that more children have access to life-saving treatment.
For more information, please contact Kevin Phelan.
References
ACF et al (2017). Innovations in CMAM Treatment Protocols. A Workshop Report: Dakar, October 19th 2017. No Wasted Lives Coalition.
Alé F, Phelan KP, Issa H et al. Mothers screening for malnutrition by mid-upper arm circumference is non-inferior to community health workers: results from a large-scale pragmatic trial in rural Niger. Archives of Public Health. 2016 (74:38).
Bailey J, Lelijveld N, et al. Combined Protocol for Acute Malnutrition Study (ComPAS) in rural South Sudan and urban Kenya: study protocol for a randomized controlled triel. Trials. 2018 Apr 24;19(1):251.
Binns PJ, Dale NM, Banda T, Banda C, Shaba B, Myatt M. Safety and practicability of using mid-upper arm circumference as a discharge criterion in community based management of severe acute malnutrition in children aged 6 to 59 months programmes. Arch Public Health 2016 Jun 15;74;24. doi: 10.1186/s13690-0136-x. eCollection 2016.
Blackwell N, Myatt M, Allafort-Duverger T, Balogoun A, Ibrahim A, Briend A. Mothers Understand And Can do it (MUAC): a comparison of mothers and community health workers determining mid-upper arm circumference in 103 children aged from 6 months to 5 years. Archives of Public Health. 2015;73(1):26.
Blanchet K, Sistenich V, et al. An evidence review of research on health interventions in humanitarian crises. London School of Hygiene and Tropical Medicine, October 2015.
Cichon B, et al. Children with moderate acute malnutrition have inflammation not explained by maternal reports of illness and clinical symptoms: a cross-sectional study in Burkina Faso. BMC Nutrition. 2016; 2:57
ECF, Minding the Undernutrition Evidence Gap: Findings of the Key Expert Consultation. 2018. Eleanor Crook Foundation, found at: www.eleanorcrookfoundation.org
Fabiansen C, Yaméogo CW, Iuel-Brockdorf A-S, Cichon B, Rytter MJH, Kurpad A, Shepherd S, et al. (2017) Effectiveness of food supplements in increasing fat-free tissue accretion in children with moderate acute malnutrition: A randomised 2 × 2 × 3 factorial trial in Burkina Faso. PLoS Med 14(9): e1002387.
Goossens S, Bekele Y, et al. (2012) Mid-Upper Arm Circumference Based Nutrition Programming: Evidence for a New Approach in Regions with High Burden of Acute Malnutrition. PLoS ONE 7(11): e49320
Isanaka S, et al. Comparison of Clinical Characteristics and Treatment Outcomes of Children Selected for Treatment of Severe Acute Malnutrition Using Mid Upper Arm Circumference and/or Weight-for-Height Z-Score. PLoS One. 2015; 10(9): e0137606.
Maust A, Koroma AS, Abla C, et al. Severe and Moderate Acute Malnutrition Can Be Successfully Managed with an Integrated Protocol in Sierra Leone. J Nutr 2015 Nov;145(11):2604–9.
Myatt M, Khara T, Schoenbuchner S, et al. Children who are both wasted and stunted are also underweight and have a high risk of death: a descriptive epidemiology of multiple anthropometric deficits using data from 51 countries. Arch Public Health 2018; 76: 28.
Philip T, et al. Low-dose RUTF protocol and improved service delivery lead to good programme outcomes in the treatment of uncomplicated SAM: a programme report from Myanmar. Maternal and Child Nutrition (2015),11, pp. 859–869.
No Wasted Lives, 2018. A statement from the Council of Research & Technical Advice on Acute Malnutrition (CORTASAM). A research agenda for acute malnutrition. No Wasted Lives, 2018.
Shekar M et al. Investing in Nutrition: The Foundation for Development: an Investment Framework to Reach the Global Nutrition Targets. World Bank 2016.


 English
English Français
Français Deutsch
Deutsch Italiano
Italiano Español
Español