SAM and MAM programming in East and West Africa: An insight into continuum of service provision for acute malnutrition treatment
By Rebecca Brown, Kate Sadler, Tanya Khara, Marie McGrath and Jeremy Shoham
Rebecca Brown is an experienced public health nutritionist engaged as an ENN consultant to lead on this review.
Kate Sadler is an experienced public health nutritionist engaged as an ENN consultant to support this review.
Tanya Khara, Marie McGrath and Jeremy Shoham are ENN Technical Directors.
ENN extends thanks to UNICEF, WFP, WHO and UNHCR headquarters, regional and country staff and ministry of health staff for their help in planning the scope of this exercise, contributing data, contextual insights and valuable review. We would also like to extend our thanks to all individual and country stakeholders included in the review who provided data, participated in the online survey and reviewed final reports. Finally, ENN gratefully acknowledges the support of the Eleanor Crook Foundation for funding this work.
The findings, interpretations and conclusions in this article are those of the authors. They do not necessarily represent the views of the contributing individuals and organisations.
Location: East and West Africa
What we know: Combined data on location and links between SAM and MAM treatment services is not globally available.
What this article adds: Between January and June 2019, ENN undertook a basic mapping of United Nations (UN) -supported severe acute malnutrition (SAM) and moderate acute malnutrition (MAM) treatment in selected countries in East and West Africa. ENN collated and analysed available UN data on SAM and MAM admissions at national and sub-national levels and on geographical/treatment coverage. An online survey contextualised the data provided. Conclusions on service alignment were limited by significant gaps in availability and consistency of data within the timeframe available and at the level of data collection. While good examples exist, in general there are gaps in how outpatient therapeutic programmes (OTPs) and targeted supplementary feeding programmes (TSFPs) are operationally aligned. At sub-national level a degree of geographical convergence of SAM and MAM services was observed but could not be mapped at facility level. Referral tracking between services, successful referral and complicated case service availability/linkage to other services could not be determined. Variable discharge criteria and supply pipeline breaks for supplies were commonly reported. Lower MAM geographical coverage compared to SAM likely reflects different targeting strategies and coverage ambitions for these services, variable integration within national systems, consideration of TSFPs only, and possible resource shortfalls. No single UN agency is responsible for data management and oversight of continuum of care for acute malnutrition. Findings warrant more in-depth reviews of service availability and alignment in multiple contexts, product supply chain, referral systems and practices, and protocol adaptations.
Background
As part of ENN’s initiative to collate and appraise experience and evidence around the delivery of programmes in relation to continuum of care for acute malnutrition treatment1, we undertook a basic mapping exercise and review of current practice in severe acute malnutrition (SAM) and moderate acute malnutrition (MAM) treatment in selected countries in East and West Africa between January and June 2019. The exercise aimed to determine the extent to which services for the treatment of children with MAM and SAM are aligned with each other in these regions, which were selected due to their high burden of acute malnutrition and widespread treatment services. For this exercise, we examined SAM treatment as those services supported by UNICEF and WHO, and MAM treatment in the form of targeted supplementary feeding programmes (TSFPs) delivered by World Food Programme (WFP)2. The mapping was carried out against the backdrop of policy and guidance whereby SAM services are in general being scaled up with UNICEF support as a systematic service in health systems, albeit in an incremental way; whereas MAM treatment implementation is led by WFP guided by contextual factors (global acute malnutrition (GAM) prevalence, food insecurity, etc.) as reflected in the Global Nutrition Cluster (GNC) MAM decision tool3.
Based on data availability, the mapping specifically aimed to collect and compare SAM and MAM treatment admissions data at national and sub-national level in selected countries in the region and identify geographical crossover of services and the extent to which protocols are aligned. This initiative was necessary as data on SAM and MAM treatment is not currently collated globally. The scope of work was determined by available funding and timeframe and considered a first step to bringing some visibility to reports of unaligned services from programmers.
For the purpose of the mapping, ENN defined continuum of acute malnutrition care as the extent to which treatment programmes for children with MAM and those with SAM, both complicated and uncomplicated, are aligned on a number of levels, including how successful referrals between services are operating. We recognise this is just one part of a broader continuum of care for malnourished children that encompasses prevention.
The mapping was undertaken with input from UNICEF and WFP East Africa and West Africa regional offices, who in turn engaged with country offices as necessary to secure available data and with UNHCR East Horn and Great Lakes (EHAGL) regional office. The GNC was also engaged and country cluster representatives contacted as potential additional sources of data. No data was provided by regional WHO offices.
This article summarises key findings and recommendations.
Methodology
The mapping began with initial discussions with representatives from UNICEF, WFP, WHO, GNC and UNHCR headquarters and regional offices to define parameters and data sources mapping. It was agreed that countries of focus for the review would be those classified in the same regional zones by both UNICEF and WFP, as follows:
West Africa: Burkina Faso, Cameroon, Central African Republic, Chad, Mali, Mauritania, Niger, Nigeria and Senegal.
East Africa: Burundi, Ethiopia, Kenya, Rwanda, Somalia, South Sudan and Uganda.
Existing programme data was collected from regional nutrition data managers at WFP (MAM data) and UNICEF (SAM data) separately and collated by ENN. Exceptions were South Sudan, where MAM and SAM treatment data for 2017 and 2018 was provided in combined form by the National Nutrition Cluster, and Kenya, where combined data on referral between MAM and SAM services was provided by government. Data on SAM and MAM admissions at national and sub-national levels and on geographical/treatment coverage where available in the selected countries was collected. In addition, UNHCR EHAGL regional office shared its own mapping of alignment of available services for SAM and MAM for refugee populations in the selected countries. Data was also sought on treatment admissions and referrals, but was not available in time from the CMAM Report (individual agency/country permissions needed), Action Against Hunger (data not collated) and World Vision International (insufficient detail).
An online survey (in English and French), proposed by the East Africa regional team, was also targeted to representatives from government, UN and non-governmental organisations (NGOs) in all selected countries. The survey (completed by 116 respondents in East Africa4 and 46 in West Africa5) collected broader information on the country approach to treatment of acute malnutrition (both SAM and MAM), the structure of the services, protocols (including products used), admission and discharge criteria, level of integration, mechanisms and monitoring for referrals, reported barriers to ensuring continuum of care for acute malnutrition, examples of good models of continuum of care, and ideas on how continuum of care for acute malnutrition could be improved.
Limitations
The data collected was secondary and from multiple sources, with consequently varying definitions, and was incomplete, particularly in relation to coverage. Data collection and the online survey were limited to selected countries in two regions of Africa, to a limited range of government, UN and NGO respondents (particularly for West Africa) and to humanitarian contexts, and therefore must be interpreted with caution. The online survey represents personal opinions and representation across countries is not comparable. The review would have benefited from a context analysis covering national strategies, national nutrition profile and sub-national-specific analysis, including prevalence of GAM, but this was not feasible within the timeframes. Specific limitations regarding data available and/or the degree of analysis possible within the scope of work are further reflected in the results and conclusions.
Results
Coverage and geographical alignment
Comparable data on geographical coverage (proportion of health facilities offering the service) was available only for countries in West Africa6 (see Box 1 for limitations). This data illustrates the more widespread coverage of SAM services compared to MAM in 2017 and 2018, reflecting the common strategy of SAM service scale-up at national levels in the health system (see Figures 1, 2 and 3). Notable exceptions are Chad and Mauritania, where there were similar levels of geographical coverage for both services; i.e. proportion of facilities offering the service. Although it cannot be assumed that there is 100% overlap in the facilities offering both services throughout the year (MAM treatment in Mauritania only operates for five months per year), the higher the geographical coverage reported for both services, the greater is the degree of likely overlap.
Box 1: Variations in definitions of coverage
The mapping highlighted limitations in the comparability of coverage data for MAM and SAM programming and ongoing difficulties with relying on estimates of treatment coverage. Both SAM treatment coverage and MAM treatment coverage figures for West Africa obtained are calculated as the number of children treated as a proportion of the estimated overall burden. Burden is calculated from estimates of prevalence, population and incidence. There are well publicised issues with such estimates and the errors involved in their calculation may have a different magnitude of implications when applied to SAM or to MAM, limiting the utility of comparisons. SAM geographical coverage is calculated as the number of health facilities treating SAM out of the total number of health facilities in a country. In some cases, MAM coverage is calculated in the same way; however, in many cases this data was not provided.
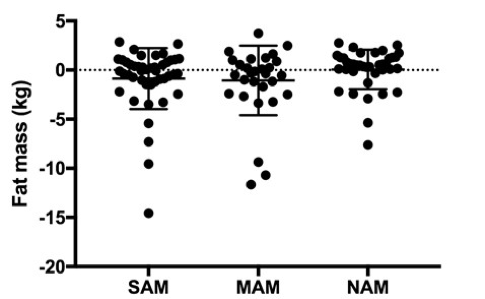
Availability of data on treatment coverage (proportion of affected children who are accessing the services) was limited to rough estimations (projected burden compared to actual admissions), rather than on assessment and was made available for SAM in all countries and for five countries for MAM (see Figures 4 and 5)7. It has therefore not been possible to make any robust comparisons between what is being achieved for MAM and SAM, beyond the need for improvement in practical methods to routinely calculate and report on treatment coverage, a critical indicator of programme impact for both SAM and MAM treatment.
Figure 1: Geographical coverage of SAM and MAM treatment in selected countries in West Africa in 2017

Figure 2: Geographical coverage of SAM and MAM treatment in selected countries in West Africa in 2018

*Very limited TSFP has been operating in Senegal for two years due to absence of resources.
**A BSFP that includes MAM children is being implemented in Cameroon (data provided) and in Northeast Nigeria (data not shown here).
** No data on geographical coverage of MAM treatment provided by Central Africa Republic (CAR).
Figure 3: Geographical coverage of SAM treatment in selected countries in East Africa, 2017 and 2018

Figure 4: SAM and MAM admissions data from selected countries in East Africa, 2017 and 2018

Figure 5: SAM and MAM admissions data from selected countries in West Africa, 2017 and 2018

Geographical and treatment coverage data as currently collected cannot in general tell us if MAM and SAM services are geographically aligned at a facility level. In nearly all cases, data or mapping on the geographical overlap at facility level in the location of services for SAM and MAM treatment was not available in the timeframe of the mapping. Notable exceptions to this and good examples of what is possible are Somalia, where a detailed map of services is being maintained (see Figure 6); Kenya, where referrals between TSFP and OTP are documented and reported by county and then national level; and UNHCR for refugee settings in East Africa.
Figure 6: UNICEF mapping of stabilisation centre (SC), OTP and TSFP sites in Somalia, September 2018
At a sub-national level, the degree to which both services are in place and admitting children can be discerned to some extent from the data collected on admissions by district for the selected countries8. Although we cannot assume that the service reaches the whole district, that it is available for the whole year, or that beneficiaries have equal and opportune access to all services, 2018 sub-national data on admissions indicates that in Kenya, South Sudan, Ethiopia and Niger both SAM treatment and MAM treatment services were present in all the districts providing data. Burundi, Uganda, Burkina Faso, Chad, Mali and Mauritania all have significant proportions of districts/regions where SAM treatment was implemented without MAM treatment. In Rwanda, Nigeria and Cameroon, data indicated there was no MAM treatment in the form of targeted SFP in any districts in 20189. In both Nigeria and Cameroon10 an ‘expanded’ prevention programme (i.e. expanded to manage MAM cases) is being implemented as an alternative strategy for reaching children with MAM. Whether this was the case in other contexts was not captured and is a limitation of the mapping. In Rwanda WFP reported MAM programming only in camp settings. Only in Mali did the sub-national data for 2018 suggest that MAM treatment was being implemented without SAM treatment, and then only in two districts. Together these findings indicate there is a range of different combinations of SAM and MAM treatment on the ground, but that it is common for SAM treatment to be implemented without MAM treatment in the form of TSFPs. Further mapping is required to comprehensively understand how continuum of care is being provided in the absence of TSFPs in those cases (e.g. counselling, social protection, blanket feeding approaches).
Alignment of the services where they do coincide
The majority of survey respondents in both West and East Africa reported that SAM and MAM services in their country or region are provided in combination. This suggests there is an ambition that SAM and MAM treatment should be parts of a whole in terms of national and/or agency protocols and criteria, monitoring and reporting, and successful movements of children between them where they are provided in the same place. The level of integration in the health system reported by survey respondents was also in general positive for both MAM and SAM. This mapping exercise was not able to back these findings up with quantitative data.
The survey indicated that there is a wide range of standard and non-standard discharge criteria in place for SAM treatment, which may have implications for continuum of care. A number of respondents in West Africa, and particularly in East Africa, noted that SAM discharge criteria were adapted; i.e. lowered (e.g. from MUAC >=125 to MUAC>115), so that children were discharged sooner from OTPs when MAM treatment (SFPs) was present. In East Africa the majority of respondents in Burundi, Ethiopia, Rwanda and Uganda reported that children with SAM are discharged once cured (no acute malnutrition); while one third of respondents in Kenya, 40% in Somalia and half in South Sudan reported discharging SAM children to TSFP one they reach MAM criteria. However, a larger number of respondents indicated that the presence or absence of MAM treatment did not lead to SAM discharge protocol change. Whether such practice is detrimental to continuum of care requires further investigation.
Referral between SC and OTP components
Most respondents in both East (73%) and West Africa (80%) reported that outpatient services can successfully refer complicated cases of SAM to an inpatient facility. More (over 90% in both regions) reported that referral was successful the other way; from a facility after stabilisation to an outpatient programme. Geographical distance between the outpatient and inpatient facilities was the major barrier identified to achieving successful referral. Most respondents reported that, at local level, monitoring systems are in place to assess whether referrals are being made successfully; however, it is not possible to conclude from the data on the quality and completeness of these systems to sufficiently ensure individual children are not lost between these components of therapeutic care.
Referral between MAM and SAM services
Data relating to referral between SAM and MAM services is generally not collected/collated in standard SAM and MAM national reporting formats, although it may be available at lower level. It was not possible, given the timeframe, to examine records kept at district/facility level or by individual agencies at country level to report on different mechanisms in place; thus we cannot discern the degree of convergence in referrals between services. Data on numbers of referrals made from SAM treatment to MAM treatment and vice versa are available for Kenya; however, the utility of this information is limited for exploring continuum of care as it does not tell us whether referrals were successful, i.e. whether children actually arrived.
The survey responses suggest in general that there are challenges with referral between MAM and SAM services in most countries. Respondents in both East and West Africa reported that many SAM treatment centres could not successfully refer children to MAM treatment centres consistently, even when the service is in place. Respondents were in general more positive about the availability of SAM services for those children identified with SAM in SFPs and requiring referral.
Respondents in both regions described considerable variation in management of acutely malnourished infants under six months old. In terms of access, 17% of respondents in West Africa and 25% in East Africa reported that the service did not admit acutely malnourished infants for treatment. Among those who reported infants being admitted, 50% and 40% of respondents in West and East Africa respectively reported the use of non-standardised admission criteria coupled with variable discharge criteria.
Expressed challenges to continuum of care
The six main barriers to continuum of care for children with acute malnutrition reported in East Africa are, in order of priority: lack of financial resources, insecurity/issues with access, limited geographic coverage of services implemented at health-facility level, product pipeline issues, lack of capacity at health centres, and limited infrastructure (see Table 1). The type of barrier experienced obviously differs by country: Somalia and South Sudan rated access and security issues as the primary barrier; for Kenya pipeline issues and access/security issues were a major barrier; and for Burundi, Rwanda and Uganda main barriers were limited geographical coverage and lack of capacity, while limited financial resources was a major barrier common to all. Cross-cutting all these factors was a reported lack of coordination among agencies and between levels of the health system operating the different services, which leads to children being lost to follow-up. High caseloads paired with low human resources are also reflected as barriers to the extent to which treatment programmes for children with MAM and SAM are aligned and successfully making referrals between the two services. Similar barriers were reported in West Africa (see also Table 1).
Table 1: Main reported barriers to continuum of care for children with acute malnutrition in East and West Africa (descending order)

Availability and alignment of data
Collection of data for this exercise highlighted that, in most instances, no single agency at country or regional level (or at global level) has overall responsibility for data continuity and monitoring of treatment for acute malnutrition. Although several survey respondents suggested a key role for government health information systems and country clusters in the collection and collation of relevant SAM and MAM service data, this exercise did not succeed in accessing these sources, perhaps due to timeframe constraints and the level at which data was being sought. Given the need for national systems for sustainable reporting on services for nutrition, the question remains how progress in achieving a continuum of care can be tracked at regional or global level. A clearer picture of service coherence can be presented in those exceptions when one agency at national level has oversight of the range of services available for acute malnutrition in different areas (but not necessarily responsibility for the delivery of all of them), as was the case in Kenya (led by government), South Sudan (Nutrition Cluster) and UNHCR programmes (East Africa).
This exercise identified a lack of alignment in the data being collected for SAM and MAM by individual agencies, through national ministry of health systems, and in some instances within agencies in a number of areas. As noted above, treatment and geographical coverage data available to us was limited in its robustness, comparability and completeness in many cases, particularly for East Africa. Differences in methods of calculating geographical coverage and treatment coverage for SAM and MAM further limited comparability.
Several specific data gaps when collecting data at this level were also highlighted. We have not been able to present data on the crossover between MAM and SAM treatment at facility level. Although this has been possible to some extent at district level using admissions figures, it is important to note that yearly admissions figures may not represent the service, particularly for MAM treatment, being available throughout the district or even for the full year.
At this level of data collection it was also not possible to comprehensively determine the extent to which SAM and MAM treatment services are linked where they are being implemented in the same geographical area; e.g. existence of systems for referral between them, distances between them and the degree to which protocols are aligned. The extent to which this information exists at national level and the extent to which it is harmonised within or across agencies requires further investigation. Equally, data on the extent to which referrals are being made successfully for complicated cases between inpatient and outpatient care was not possible to discern at this level as data on complicated SAM is mainly integrated within collated SAM figures at national level. Although some data on numbers of complicated admissions is available, with no denominator of complicated cases it is not possible to draw helpful conclusions. Finally, data on level of service or any systems in place for identifying and referring complicated MAM for appropriate treatment was not available.
Discussion
Considerable data is currently collected and collated on SAM and MAM treatment and involves huge effort and investment by government, agencies and individuals at regional, national and sub-national levels. While fully appreciating this commitment, and the short timeframe that was available for this exercise, the data obtained points to gaps in the nature, availability and consistency of data at regional and global level for understanding the extent to which a continuum of care for children with acute malnutrition is being achieved. Further information may be available at national and sub-national level and further investigation is therefore required in order to be able to draw conclusions on continuum of care. Clarity on what constitutes continuity of care across different contexts, including where there is no intention to implement a TSFP and which UN agency is responsible for liaising with government on such oversight, provision or support, is also needed. Based on this, further investigation of the level and extent of gaps in information and potential ways to fill them will be needed in order to provide a more secure basis for discussions on the extent to which the international community and governments can better ensure a continuity of care for acute malnutrition and track progress.
Although there are crossovers in implementation areas (and, to a limited extent, in protocols), the data available and experiences shared indicate that even where they are both being implemented, SAM and MAM services are often not practically aligned in a way that is conducive to a continuum of care; i.e. to ensure that children can move through the different components appropriately and successfully. Important aspects of this include the limitations identified in the tracking of referrals, the need for clarity on how admission and discharge criteria for the services coherently fit together, and gaps in support for at-risk infants under six months of age. Critically, supply breaks for ready-to-use therapeutic foods (RUTF) and ready-to-use supplementary foods (RUSF) were reported in both regions as compromising continuity of care for children.
Despite its limitations, this mapping exercise provides important clues to and highlights significant gaps in our collective capacity to deliver a continuum of care to children who are acutely malnourished. Both the data and reported experiences indicate that SAM treatment without MAM treatment (in the form of TSFPs) is commonplace. This pattern reflects differences in global strategies for the implementation of these two services; TSFPs are configured for delivery in emergency contexts that prioritises areas/populations of highest vulnerability according to several criteria, including GAM rate of greater than 10%11, and may be seasonal. SAM treatment scale-up and 100% coverage targets are potentially realisable through an established system (health service) with widespread reach and governed by global WHO SAM guidance. The substantially larger MAM caseload, limited evidence on feasible implementation within the health system, absence of normative guidance for MAM treatment and prevention, and no UN ambition for 100% coverage are all factors contributing to the lack of equivalent MAM programme scalability.
It is important to emphasise that, while this exercise focused on mapping availability of TSFPs as a treatment option for MAM (reflecting WFP’s operational experience and primary approach), TSFPs are not the only intervention options for MAM. Approaches to care for MAM children reported in the regions included nutrition counselling, referral to health centres, referral to ‘preventive’ services, and management in blanket supplementary feeding programmes (BSFPs). These interventions were not mapped in this exercise. It is also not possible to determine from this mapping the extent to which TSFPs are not present in settings where they should be according to criteria set out in the MAM decision tree or due to resource shortfalls.
Conclusions and recommendations
As a priority, we need to improve transparency on the degree to which a continuum of care is being provided to children with acute malnutrition to learn from contexts where it is being achieved, and identify where and how we need to act where it is not. We recommend the following actions:
- A more in-depth and comprehensive global review of MAM and SAM treatment services at national and sub-national level. This should include different models and care options (e.g. prevention programmes that are being implemented with a treatment aim); a mix of settings, including Asia and non-emergencies; cluster-activated countries; and context-specific analysis (e.g. GAM prevalence, emergencies/non-emergencies, donor vs no donor support). A review would benefit from scrutinising methods for estimating coverage for SAM and MAM services and more in-depth investigation of data and services for complicated acute malnutrition.
- A detailed global review of bottlenecks to predictable and sustained supply of RUTF and RUSF to further identify the extent and the patterns of pipeline breaks and major bottlenecks to resolution, given how fundamental supply-chain security is to continuum of care.
- A review of implementation protocols for admission, discharge and referral between SAM and MAM treatment programmes (including early discharge of recovering SAM children to TSFPs) to examine outcomes and clarify best practice. Examples of referral mechanisms that are functioning and being reported at local levels could be used to identify good scalable models, help more clearly determine how to measure successful referral, and inform guidance on child movement through levels of service to sustained recovery.
- The potential to include MAM data in national and international databases that capture SAM data (e.g. UNICEF global Nutridash platform) should be explored, building on learning from contexts where this has been achieved.
We hope that the findings of this mapping inform wider conversations and initiatives that are drawing on emerging evidence to examine what needs to change – including ways of working between UN agencies, governments and partners, and options available for care – to ensure that children suffering from malnutrition receive the most appropriate care across the continuum of their experience, including but not limited to acute malnutrition.
For more information, contact Tanya Khara.
Endnotes
1Collated in a special edition of Field Exchange (issue 60); www.ennonline.net/fex
2As outlined in 2011, UNICEF is responsible for SAM treatment and WFP is responsible for MAM treatment; hence UNICEF and WFP-sourced data on services supported or delivered was sought.
3GNC, 2017. Moderate Acute Malnutrition. A Decision Tool for Emergencies. GNC MAM Task Force. March 2017.
4Burundi (n=14), Ethiopia (n=14), Kenya (n=20), Rwanda (n=6), Somalia (n=31), South Sudan (n=27) and Uganda (n=4); across government (n=6); NGOs (n=79); and United Nations (n=31).
5Burkina Faso (n=6), Cameroon (n=3), Central African Republic (n=2), Chad (n=3), Mali (n=4), Mauritania (n=1), Niger (n=7), Nigeria (n=17), and Senegal (n=4); across government (n=4); NGOs (n=15); United Nations (n=26); and a research centre (n=1).
6Comparable estimates of geographical coverage (proportion of health facilities/health catchment areas where the service is provided) for MAM was available for a limited number of countries in West Africa only (Burkina Faso, Chad, Mali, Mauritania, Niger).
7Comparable estimates of treatment coverage for MAM were available for Burkina Faso, Chad, Mali, Mauritania and Niger. Data for MAM treatment in Cameroon as part of an expanded blanket supplementary feeding programme (BSFP) was provided but not included here due to difficulty of comparison. Data from the pilot BSFP in Northeast Nigeria was not available in the timeframe of this review.
8Detailed data is available in the full regional reports; see contact at end of article.
9Comparable data for Senegal and Somalia was not available.
10Eveline Ngwenyi, Mica Jenkins, Nicolas Joannic and Cécile Patricia (2019). Addressing acute malnutrition in Cameroon during an emergency: Results and benefits of an integrated prevention programme. Field Exchange issue 60, June 2019. www.ennonline.net/fex/60/acutemalnutritioncameroon
11Moderate acute malnutrition: a decision tool for emergencies. MAM Task Force. Global Nutrition Cluster. Updated March 2017.


