Testing an adapted severe acute malnutrition treatment protocol in Somalia
Summary of research1
By Naoko Kozuki, Jama Mohamud Ahmed, Mukhtar Sirat and Muna Abdirizak Jama
Naoko Kozuki is the Health Research Adviser for the International Rescue Committee (IRC), overseeing its health research portfolio. Her research focuses on maternal, neonatal and child health and nutrition, and community health systems.
Jama Mohamud Ahmed is the Nutrition Research Officer for IRC Somalia, responsible for coordinating, supporting and supervising research programmes.
Mukhtar Sirat is the Nutrition Manager for IRC Somalia. His role is to plan, coordinate and implement nutrition programmes, focusing on both curative and preventive interventions.
Muna Abdirizak Jama is the Health Manager for IRC Somalia. She is a medical doctor by training and oversees health, nutrition and community development programmes.
This project is funded by Elrha’s Research for Health in Humanitarian Crises (R2HC) programme, which aims to improve health outcomes by strengthening the evidence base for public health interventions in humanitarian crises. The R2HC programme is funded equally by the Wellcome Trust and the UK Department for International Development (DFID). Visit www.elrha.org/r2hc for more information.
Location: Somalia
What we know: Some severe acute malnutrition (SAM) treatment approaches have potential inefficiencies, such as poor continuity of care from SAM to MAM phases of treatment, higher than necessary dosage of Ready-to-Use Therapeutic Food (RUTF), and management of dual supply chains for RUTF and Ready-to-Use Supplementary Foods.
What this article adds: The International Rescue Committee (IRC) conducted a prospective cohort study to test an adapted protocol for the treatment of SAM in Mogadishu, Somalia using a reduced RUTF dosage (two sachets per day, weekly for SAM phase; one sachet per day, every two weeks, in MAM phase). There was no control group. In total 727 SAM children without complications were enrolled. Median number of weeks to recovery was 14; recovery rate was 98% (1% defaulted and 1% were referred); non-response and death rates were 0%. Good treatment adherence in the study was likely helped by close proximity of services to beneficiaries. Further research is needed on how to enable beneficiaries to see through treatment to full recovery and the potential impact of direct admission of MAM cases.
Context
The International Rescue Committee (IRC) conducted a prospective cohort study to test an adapted protocol for treating severe acute malnutrition (SAM) as outpatients in the outpatient therapeutic programme (OTP) of Karaan Clinic, Mogadishu, Benadir district, Somalia, with the aim of improving continuity of care for severe acute malnutrition (SAM) children. The adapted protocol treated SAM children until full recovery with a simplified dosage protocol. Treatment was based on the provision of ready-to-use therapeutic food (RUTF) for children in both severe and moderate malnutrition ‘zones’, with children in the severe zone receiving weekly treatment at two RUTF sachets per day and, once in the moderate zone, two-weekly treatment at one RUTF sachet per day, based on MUAC or WHZ benchmarks (both mid-upper arm circumference (MUAC) and weight-for-height z-score (WHZ) were used as admission criteria). There was no control group.
Headline findings and some implementation experiences are shared in this article; full results will be submitted for peer review publication in 2019.

Methods
Between January and March 2018 the study enrolled SAM children aged 6-59 months presenting to Karaan Clinic OTP with no medical complications and with MUAC 90 - <115mm or WHZ <-3. Children were treated weekly at the same clinic, with a total of 14 RUTF sachets (two per day) sent home with the caregiver, until the children had achieved two consecutive visits with MUAC ≥115mm (for MUAC enrollees) or WHZ ≥-3 (for WHZ enrollees, based on height taken monthly). On reaching that anthropometric benchmark, children were treated once every two weeks, with a total of 14 RUTF sachets (one per day) sent home with the caregiver. Children were considered recovered when after two consecutive visits, they achieved MUAC ≥125mm (for MUAC enrollees) or WHZ ≥-2 (for WHZ enrollees). The children were retained at the OTP throughout the course of their treatment. Qualitative data were collected from clinic staff and caregivers.
Results
The study enrolled 727 SAM children without complications. A total of 700 (96%) had eligible results, of whom 640 (analytic sample) were treated with strict adherence to protocol. In the analytic sample, the median age of enrolment was eight months (range 6-42 months), with 41% male and 59% female. The caregivers reported a median time of 21 minutes to reach the facility, with 72% walking there. Anthropometry at enrolment is described in Table 1; treatment outcomes are described in Table 2. Median number of weeks to recovery was 14 weeks (IQR: 12-16, range 7-27 weeks). Full data will be published elsewhere.
Table 1: Anthropometry at enrolment
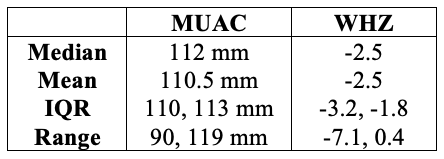
IQR: inter-quartile range
Table 2: Treatment outcomes and weeks to outcome
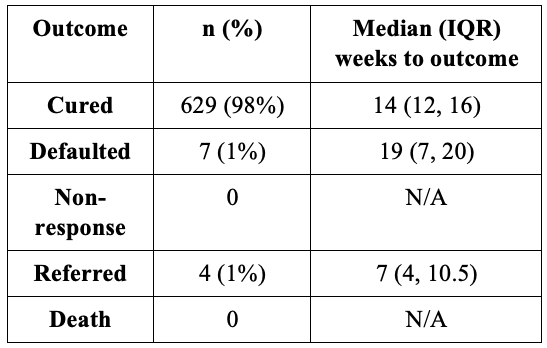
Default: Three consecutive missed visit. Non-response: non-recovery after 28 weeks (derived from 12 weeks allowed in OTP programmes, 16 weeks in TSFP programmes).
Discussion
This study did not include a control group; thus definitive comparisons could not be made against a standard CMAM programme. However, we have made several observations, as follows:
Continuity of care
The Somalia Integrated Management of Acute Malnutrition (IMAM) national protocol recommends treatment of uncomplicated cases of SAM until full recovery (MUAC ≥12.5cm or WHZ ≥ -2). In practice, if a Targeted Supplementary Feeding Programme (TSFP) exists, some programmes discharge recovering SAM children from the OTP at MUAC ≥ 11.5cm / WHZ ≥ -3 and refer to the TSFP for treatment completion. This was the situation in the IRC programme area. Qualitative data collected from clinic staff and caregivers revealed poor continuity of care between the OTPs and TSFPs under this practice; it appears that few caregivers completed the referral to a TSFP. At the time of the study, while both OTPs and TSFPs were present in Benadir district, OTPs and TSFPs were not co-located and were supported by different implementing partners. Pre-pilot data on referral completion rates between OTP and TSFP were not available.
Clinic staff believed that the rate of recovery from SAM to full recovery is significantly improved in the test protocol compared to previous practice. This does not necessarily mean that co-location of SAM and MAM treatment is sufficient in itself to ensure continuity of care in every location; programmatic experience from other contexts has found poor treatment completion despite co-location of SAM and MAM services. In this study, physical proximity of the beneficiaries to the clinic is likely to have contributed to high treatment adherence to full recovery. For areas with less straightforward access, further insights into infrastructure and behaviours are needed to determine how best caregivers can be supported to continue treatment for their children through to full recovery.
We consider that MAM cases in recovery from SAM are more at risk than children who present with MAM. In line with Somalia national guidelines and WHO 2013 SAM guidance, the study protocol facilitates treatment to full recovery and improves continuity of care for SAM cases.
Caseload considerations
The IRC’s vision for a combined treatment protocol is for SAM and MAM to be treated in the same location, including direct admissions of MAM cases.2 However this study only enrolled SAM cases. In the research design phase, staff of the clinic, nutrition staff of IRC Somalia and the Principal Investigator concluded that, without sufficient additional financial and human resources needed to absorb both SAM and MAM cases, the clinic would be unfairly over-burdened if direct MAM admissions were included. This risked compromising the potential success of the combined protocol for logistical reasons rather than the efficacy and effectiveness of the protocol itself. Thus, the study was restricted to enrolling SAM cases only. This decision was justified a few months after the end of the study when TSFP programmes were opened in OTP locations in Benadir district, including Karaan Clinic where this study was held. No additional human or financial resources were provided to Karaan Clinic to absorb the influx, which led to unreasonably long hours for staff, reduced functionality of the OTP programme and insufficient physical space to absorb the extra MAM children. This experience highlights that any ambitions to expand current OTP-only or TSFP-only programmes to include broader categories of children must take account of the inevitable initial growing pains and long-term implications for sustainability by providing sufficient resources.
Conclusion
This study shows that SAM children without complications can be successfully treated under a simplified dosage protocol that supports a continuum of treatment; the protocol was consistent with national guidelines to treat children to full recovery. We believe that the simplified protocol tested has the potential to ease logistical constraints (e.g. using lesser amounts of one product, simplify dosage calculation for clinic staff) of delivering services, particularly during emergencies or in severely access-limited locations. Further exploration is needed on the right dosage, timeline and behaviour communication with caregivers to optimise recovery rates and length of time to recovery, as well as further examination of human resource and cost implications, particularly for including direct admissions of MAM cases into programmes that currently only treat SAM cases.
For more information, please contact Naoko Kozuki.
Endnotes
1Full results from this study will be published in a future peer-reviewed publication and shared in Field Exchange.
2www.ennonline.net/fex/53/thecompasstudy


