Improving minimum dietary diversity for children aged 6-23 months when household affordability is a major constraint in northeast Bangladesh.
By Md Masud Rana, Sheikh Shahed Rahman, Md Al-Amin Shovan, Bazlul Kabir Joarder and Mohammad Raisul Haque
Md Masud Rana is a nutrition advisor for Save the Children, with a particular focus on supporting nutrition programmes in South Asia and East Africa region. Masud has worked for over 10 years in the design, delivery and evaluation of nutrition, food security and livelihoods programmes in Asia and Africa.
Dr Sheikh Shahed Rahman is Chief of Party for the Suchana programme, Save the Children International in Bangladesh. He has worked in food security and nutrition programmes in development and emergency settings for more than 15 years. He is a medical graduate and obtained his MPH from Emory University, USA.
Md Al-Amin Shovan is Manager – Monitoring, Evaluation, Accountability and Learning (MEAL) of the Suchana programme. He has over 15 years of experience working as a MEAL Specialist in the development sector in Bangladesh.
Bazlul Kabir Joarder is Technical Manager – Nutrition for Save the Children in Bangladesh in the Suchana programme. He has over 14 years of experience of working in health and nutrition-focused programmes for multiple non-governmental organisations (NGOs) in Bangladesh.
Dr Mohammad Raisul Haque is Senior Advisor – Nutrition for Save the Children in the Suchana programme. He has over two decades of public health service delivery and programme management experience for multiple NGOs and donor agencies. He holds a master’s degree in population and reproductive health research and a PhD in demography.
The authors would like to thank the donors of the Suchana programme, including the European Union (EU) and the UK Department for International Development (DFID). The findings, interpretations and conclusions in this article are those of the authors. They do not necessarily represent the views of Save the Children, EU or DFID and should not be attributed to them.
Location: Bangladesh
What we know: Mutli-dimensional approaches are needed to achieve a minimum acceptable diet for young children to prevent stunting, including increasing household income.
What this article adds: Two studies were carried out to inform the Suchana programme (2015-2022) that aims to reduce stunting prevalence in Sylhet, Bangladesh through social and behaviour-change communication (SBCC), promoting optimal infant and young child feeding (IYCF) and household food production activities to increase household income and food availability. A barrier analysis among 106 mothers from 16 villages was performed to identify barriers to and boosters of minimum dietary diversity (MDD) among children aged 6-23 months. Household income, food price and understanding of an MDD and its benefits were important determinants of MDD. Failure to remember to include diverse foods was a main barrier. Adaptations to the SBCC component were subsequently made to address this. A cost-of-the-diet (CotD) analysis was then performed to estimate the hypothetical minimum amount of money a typical household needs to purchase food to meet recommended nutrient intakes, analysed against current household income, expenditure, production and consumption. Findings show that all major nutrient requirements can be met using local markets and households can potentially afford a diet that meets energy, protein, fat and micronutrient requirements and takes into account typical dietary habits within existing levels of income, but not when non-food expenditures are taken into account. Free food from home food production activities goes some way to filling affordability gaps; however, more needs to be done to increase household income to achieve an MDD and intended programme outcomes.
Introduction
Bangladesh has made remarkable progress in reducing stunting and wasting in children under five years of age over the last 20 years. However, the rate of decline in the annual stunting rate has slowed in the last decade and an estimated six million children remain chronically undernourished (NIPORT and ICF International, 2016). More than one in three children suffer from impaired linear growth (i.e. stunting) with higher prevalence in rural areas (37.9%, versus 30.8% in urban areas) and among children from the lowest wealth quintile (49.2%, vs 19.4% in the highest wealth quintile). Geographically, Sylhet division in the North-East of the country has the highest burden where around half of all children under five years are moderately to severely stunted (NIPORT and ICF International, 2016). While causal factors are multiple and poorly understood, research has identified several, including severe food insecurity; poor maternal nutrition; poverty; poor sanitation and hygiene practices; and inappropriate complementary feeding (Choudhury et al, 2016; Ahmed et al, 2016).
In response to the multi-dimensional challenges of malnutrition, the UK Department for International Development (DFID) and European Union (EU)-funded Suchana1 programme aims to reduce prevalence of stunting in Sylhet Division. Suchana is a six-year (2015-2022), £48 million programme that aims to reach over 220,000 poor households (representing around 1.1 million people) by targeting women of reproductive age and/or adolescent girls. The programme provides a set of nutrition-specific and nutrition-sensitive interventions to improve household-level nutrition and food security and child care practices to break the inter-generational cycle of under-nutrition.2[2] Suchana’s nutrition-specific component includes a comprehensive set of social and behaviour-change communication (SBCC) interventions promoting optimal infant and young child feeding (IYCF) and maternal and child nutrition in the first 1,000 days. The nutrition-sensitive component promotes increases in household income and availability of food through home food production (HFP) interventions.
To ensure both types of interventions address context-specific immediate, underlying and basic causes of undernutrition, Suchana carried out a barrier analysis and cost-of-the-diet (CotD) assessment in Sylhet and Moulvibazar districts within Sylhet Division. This article shares experiences and findings related to improvement of dietary diversity among young children that were used to inform the programme to improve outcomes further.

A barrier analysis: Identifying barriers to achieving minimum dietary diversity (MDD) of children in Sylhet and Moulvibazar districts
Methods
In October 2017, Suchana commissioned a barrier analysis to identify barriers to and boosters of minimum dietary diversity (MDD) among children aged 6-23 months in response to multiple programme monitoring assessments identifying MDD as the worst performing IYCF indicator. The baseline study undertaken in mid-2017 found only 14.7% of girls and 15% of boys received a diversified diet containing four or more food groups. The study primarily employed a ‘doer/non-doer analysis’ to identify behavioural determinants (barriers and enablers) among those who consumed a diversified diet (‘doers’) and those who did not (‘non-doers’). It followed the barrier analysis methods specified in the ‘designing for behaviour change framework’ (TOPS, 2017; Kittle, 2013) and employed a cross-sectional survey of 106 mothers of children aged 6-23 months (53 doers and 53 non-doers) from 16 villages in the two districts.
Results
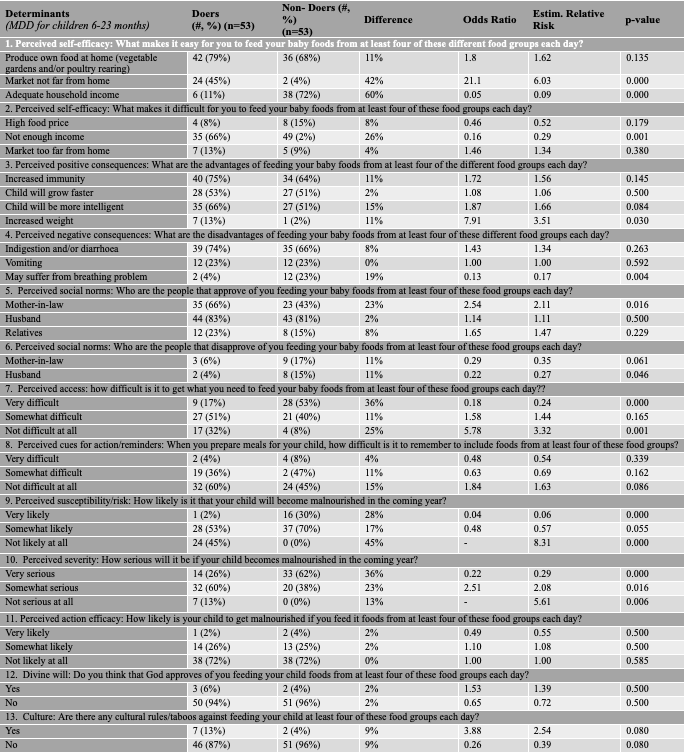
Table 1 shows a summary of the barriers and facilitators constructs generated from the data. Overall, an overwhelming proportion of respondents from both groups (doers and non-doers) identified economic factors (e.g. household income and food price) as the main facilitator for achieving MDD. As most households were primarily reliant on markets for access to food, distance to the market was also a big predictor. The barrier analysis additionally identified existing misconceptions around consuming a diversified diet (e.g. certain foods can cause indigestion/breathing problems) and a lack of full understanding of the benefits, as well as perceived difficulty of remembering to include foods from different food groups, as other important determinants of MDD. Approval and support of husbands and mothers-in-law were found necessary for practising the behaviours. However, no social, cultural or religious restrictions or taboos against consumption of a diversified diet by women or children were identified.
Table 1: Barriers and boosters of MDD among children aged 6-23 months in Sylhet and Moulvibazar districts in Bangladesh
Follow-up actions: Based on the findings of this analysis, the existing SBCC strategy and activities were revised in early 2018, as follows:
- Specific messages were developed to raise awareness of the necessity and benefits of women and children aged 6-23 months consuming a diversified diet. All of the project-specific SBCC guidelines and materials were subsequently adapted to include these messages, using multiple communication channels to reinforce impact.
- To increase family members’ support, mothers-in-law were included in existing monthly mother and child group courtyard sessions and separate male groups were formed to inform husbands/male household members. In addition, frontline staff were trained to involve family members in discussions during household-level counselling sessions.
- A new poster on MDD was distributed which visually displays different food groups to help households remember to choose food from different groups.
- One of the major contributions of the barrier analysis was an understanding of the extent to which financial constraints affect consumption of a diversified diet in this context and the important contribution of the nutrition-sensitive component of the programme (i.e. income generation) in improving household affordability. To further inform this aspect of the programme, a CoDt assessment was subsequently conducted.
A CotD analysis: When affordability is a major barrier
Rationale and objectives
While the Suchana programme’s regular monitoring data was suggesting a notable increase in household income and increased availability of food from the HFP intervention, the barrier analysis identified affordability of nutritious food as a major barrier to dietary diversity. In response, a CotD analysis was conducted in Sylhet and Moulvibazar districts to investigate the extent of the gap between household income and expenditure. This would inform necessary adjustments in programme implementation to maximise the impact on child nutrition. Specifically, the assessment set out to estimate the minimum cost of a nutritionally adequate and culturally acceptable diet for typical households and estimate the potential effect of income-generating activities (IGAs) and the HFP intervention on a household’s ability to afford a nutritious diet.
Method
The CotD3 method and software were developed by Save the Children in order to estimate the hypothetical minimum amount of money a typical household would need to purchase food to meet recommended intakes of energy, protein, fat and micronutrients, using locally available foods (Deptford et al, 2017). Food price data were collected through a market survey involving 16 urban, peri-urban and rural markets in Sylhet and Moulvibazar. Local food consumption patterns and cultural practices were identified through individual interviews covering 84 individuals and 12 focus group discussions (FGDs). Household income and expenditure, household size and composition, and HFP and consumption data were obtained from the most recent programme survey.
Key findings
Overall, the analysis found that markets in Sylhet and Moulvibazar have a diverse range of food items and can fulfil all major macro- and micro-nutrient requirements for households. However, calcium was found to be most difficult to obtain; i.e. the most significant cost driver, followed by folic acid and vitamin B12.
The cost of four hypothetical diets was estimated using CotD software for a typical household of six individuals (including a 12-23 month-old child and a breastfeeding mother); including: (i) a lowest-cost diet that only meets recommended average energy requirements (energy only (EO) diet); (ii) a lowest-cost diet that meets the average energy and the recommended protein and fat requirements (macronutrient(MAC) diet); (iii) a lowest-cost diet that meets specifications for energy, protein, fat and micronutrients but does not take into account typical dietary habits (minimum-cost nutritious (NUT) diet); and, (iv) a lowest-cost diet that meets specifications for energy, protein, fat and micronutrients and takes into account typical dietary habits and cultural acceptability (food habit nutritious (FHAB) diet).
The lowest annual cost of an EO, MAC and NUT diet for a six-person household was BDT 40,630.00, BDT 41,523.00 and BDT 64,312.00 respectively (Figure 2). However, the cost of a FHAB diet was 67% higher than the NUT diet, at BDT 107,459 per year. Within the household (Figure 3), the cost of meeting the nutritional requirements of a breastfeeding women was highest (22% of the household cost of diet), followed by the adult male (21%) and 10-11 year old children (20%).
The affordability calculation (Figure 4) shows that households can potentially afford the FHAB diet, but cannot afford to meet both the cost of the diet and additional non-food expenditures (NFE) with their existing level of income. The affordability gap ranges from BDT 193 to BDT 14,181 per year, depending on the beneficiary type and their livelihoods options. However, when the effect of the HFP element of the programme, which provides free food for the household, was also taken into account (Figure 5), the annual cost of an FHAB diet was reduced by between 2.2% and 3.2% (16-24% reduction in the household affordability gap); this demonstrates some gain, albeit not as much as the project team expected.
Figure 1: The percentage of energy and the recommended nutrient intakes for micronutrients met by a FHAB diet for the whole family
 Figure 2: Annual cost of the various diet type for a standard household with six members and average annual income
Figure 2: Annual cost of the various diet type for a standard household with six members and average annual income
Figure 3: Individual cost of the diet expressed as a percentage of total cost of the FHAB diet

Figure 4: The affordability of an EO, NUT and FHAB diet by Suchana beneficiary type (IGA intervention type and phase)
The x-axis bars refer to different project beneficiary types. Phase 1 and Phase 2 refer to the beneficiary selection cycle. On/Off-Farm refer to the ‘Income-generating activity (IGA)’ support beneficiaries received from the project. On-Farm IGAs are linked to food production through agriculture, poultry/livestock and aquaculturem; e,g. training, inputs and provision of seeds, fertilisers and pesticides. Off-Farm IGAs are livelihoods options other than farming/food productions, including water fishing, tea stalls, vegetable trading, bamboo crafting and a ferry business.
Figure 5: The potential effect of different HFP activities on the annual cost of an FHAB diet for a household with six members, including a child aged 12-23 months
Discussion and recommendations
It is well known that interventions focused on reducing poverty (i.e. generating income) as part of a multi-sector nutrition programme are not enough to have a positive impact on nutritional outcomes. Household income must go beyond a certain threshold to enable household members to practice recommended child feeding practices. This CotD analysis set a benchmark for the livelihoods component of the Suchana programme, by which increases in household income could be monitored to ensure that they are large enough to meaningfully impact household food security and nutritional status. Results of the analysis indicate that the programme should consider identifying beneficiary households that are below this benchmark and struggling to cross the threshold to prioritise them for linkages with existing government social protection programmes.
When results of this CotD analysis are compared to a previous CotD analysis conducted in the same region in 2013, it appears that the current affordability gap (BDT 193 to BDT 14,181 per year) of very poor beneficiary households is significantly lower than the previous gap of BDT 39,300 per year. This reduction cannot necessarily be attributed to the programme intervention alone; however, there are strong reasons to believe that programme interventions are meaningfully contributing to it. Furthermore, the CotD modelling exercises show that the HFP interventions appear to be improving the availability and consumption of nutritious food at household level.
Nevertheless, gains were not as great as expected and more needs to be done to increase production to eliminate affordability gaps and to improve consumption to meet an MDD. The programme should therefore continue to aim to increase household income and food production and promote equitable intra-household food distribution and consumption through its SBCC activities. The Suchana programme is considering the following recommended actions as a result of the findings presented here:
- Revisit the programme’s current livelihoods strategy and market system strategy to improve year-round production, linking beneficiaries with markets (and actions to identify potential ways) to further improve return on investment and household income.
- Strengthen activities that link the most vulnerable households with the government’s social protection scheme, health and nutrition services, and other services.
- Conduct a cost-effectiveness analysis of the kitchen garden and HFP interventions to understand whether current production, loss-to-climate effect, access to market, consumption pattern and rate of return are cost-effective and investigate further opportunities to improve productivity and consumption.
- Use the FHAB diet cost as a benchmark to track the progress of beneficiary groups in upcoming socio-economic surveys and assessments and observe changes in affordability gap to assess whether new initiatives have worked.
- Promote the consumption of cheap, nutrient-rich foods identified by the CotD analysis through existing SBCC activities.
- Intensify efforts to further engage male family members in SBCC activities. The FGDs in the CotD data collection and previously conducted formative research highlighted the dominant role of husbands or male family members in household expenditure, food purchase decisions, access to markets and ultimately income generation. Without significantly engaging the male members in the process (and changing norms), the SBCC activities are unlikely to have a significant and lasting impact on changing behaviours and practices.
An independent evaluation is planned for the end of 2019, after which the impact of the Suchana programme on stunting prevalence will be reported.
For more information please contact Masud Rana.
Endnotes
1A Bengali word which means “the beginning of something positive”.
2For further information, see: (i) https://bangladesh.savethechildren.net/sites/bangladesh.savethechildren.net/files/library/Suchana.pdf (ii) https://devtracker.dfid.gov.uk/projects/GB-1-204131
3Further information about the CotD method is available from www.heacod.org
References
Ahmed, T., Hossain, M., Mahfuz, M., Choudhury, N., & Ahmed, S. (2016). Imperatives for reducing child stunting in Bangladesh. Maternal & Child Nutrition, 12, 242-245. doi: 10.1111/mcn.12284#
Choudhury, N., Raihan, M., Sultana, S., Mahmud, Z., Farzana, F., & Haque, M. et al. (2016). Determinants of age-specific undernutrition in children aged less than 2 years-the Bangladesh context. Maternal & Child Nutrition, 13(3), e12362. doi: 10.1111/mcn.12362
Deptford A., Allieri T., Childs R., Damu C., Ferguson E., Hilton J., Parham P., et al. . (2017). Cost of the Diet: A Method and Software to Calculate the Lowest Cost of Meeting Recommended Intakes of Energy and Nutrients from Local Foods. BMC Nutrition 3 1: 26.
Kittle, B. (2013). A Practical Guide to Conducting a Barrier Analysis. New York, NY: Helen Keller International. Retrieved from https://coregroup.secure.nonprofitsoapbox.com/storage/barrier/Practical_Guide_to_Conducting_a
_Barrier_Analysis_Oct_2013.pdf
NIPORT, Mitra and Associates, and ICF International. (2016). Bangladesh Demographic and Health Survey 2014. Dhaka, Bangladesh, and Rockville, Maryland, USA: National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF International. Retrieved from http://dhsprogram.com/pubs/pdf/FR311/FR311.pdf
TOPS. (2017). Designing for Behavior Change: A Practical Field Guide. Washington, DC: The Technical and Operational Performance Support (TOPS) Program. Retrieved from www.behaviourchange.net/docs/designing_for_behavior_change_a_practical_field_guide.pdf


