Scale-up of malnutrition screening by the World Health Organization in Syria
By Mahmoud Bozo, Hala Khudari and Mutasem Mohammad
Mahmoud Bozo is a World Health Organization (WHO) Nutrition Technical Officer for Syria. He has extensive experience in malnutrition detection and management.
Hala Khudari is a WHO Technical Officer for the Eastern Mediterranean Regional Office, Cairo. Hala is a nutritionist with extensive experience in managing and coordinating health and nutrition emergency programmes in Syria and supporting other emergency contexts in the region.
Mutasem Mohammad is a Health Information Management Officer for WHO Syria. Mutasem is in charge of strengthening health information systems, assessments, data management and analysis for evidence-based planning and response.
The authors would like to acknowledge Elizabeth Hoff, WHO representative; Dr Ayoub Al-Jawaldeh, Nutrition Regional Adviser; and Ayman Al-Mobayed, Global Information Systems Officer for their support to this programme and in the writing of this article.
Location: Syria
What we know: Nutrition surveillance is a valuable means to identify cases of malnutrition, facilitate timely treatment, monitor caseloads and so plan services.
What this article adds: A pilot nutrition surveillance system (NSS) was established by the World Health Organization (WHO) and Ministry of Health (MoH) in 2014 in Syria, based on existing growth-monitoring services at 115 health facilities. The system was expanded to screen children at 802 health centres by 2018. Identified cases are referred for community-based management (86 centres) or to stabilisation centres (23) as appropriate; surveillance data informs district and national planning. From 2017, health-worker training and computerised reporting systems improved data collection and reporting quality. In 2018, of 928,000 children screened, 1.8% were moderately malnourished and 0.6% severely malnourished (0.1% complicated). System reach was expanded through mobile health teams to conflict-affected populations, non-governmental organisations and private doctors. Prevalence of global acute malnutrition (GAM) (12%) and stunting (30%) was considerably higher than national average among those identified via mobile screening. Capacity to manage complicated and uncomplicated acute malnutrition was increased through coordinated WHO, United Nations Children’s Fund and World Food Programme support. Nationally, GAM prevalence declined from 2015 (5.25%) to 2018 (2.4%). This was due to stabilisation of the situation and continued humanitarian support to meet basic needs, supported by early case detection and referral; more effective community-based management of acute malnutrition services; and infant and young child feeding interventions. Besieged populations remain highly vulnerable. Plans are to increase NSS coverage and to integrate into the national health information system.
Background
Eight years of protracted crisis in Syria has had an immense negative impact on the living conditions of the population. Violence, interruption of services and forced displacement have compromised access to basic commodities and services, including food, livelihoods, safe drinking water, sanitation, education, shelter and healthcare. This has increased the population’s vulnerability to poverty, food insecurity, poor dietary diversity and disease. This, coupled with inadequate infant, young child and maternal feeing practices and geographical and gender inequalities, has greatly heightened the risk of malnutrition in children under five years of age.
Impact of the crisis on the health system
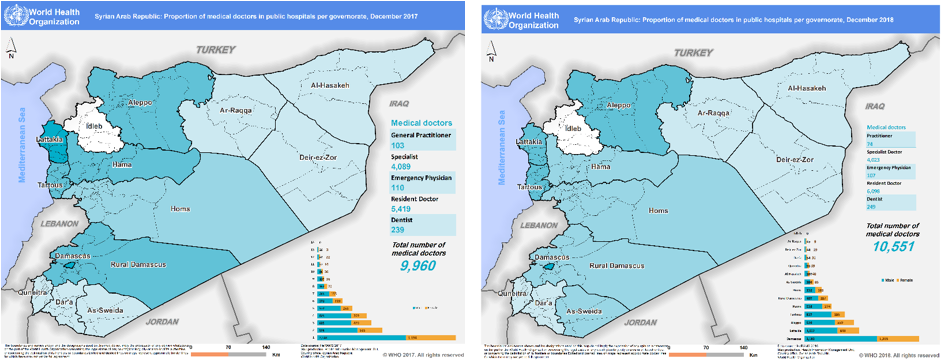
Health service delivery in Syria has been heavily disrupted as a result of the crisis and attacks have left health centres damaged and, in some cases, non-functional, significantly reducing the availability of essential health services to affected populations. By the end of 2018, out of 1,811 public health centres assessed, only 68% were reported to be functioning (46% fully and 22% partially) and, out of 11 public hospitals, 76% were reported to be functioning (52% fully and 24% partially). Thirty-one per cent of health centres were reported damaged (7% fully and 24% partially), as well as 45% of hospitals (11% fully and 34% partially) (HeRAMS 2018a; HeRAMS 2018b). Figure 1 shows the location of functioning and non-functioning health centers and hospitals across the country, which shows highly vulnerable and hard to reach or besieged areas with limited health services. This situation has been exacerbated by the fact that 50% of health workers have either fled from Syria or to safer locations within the country. Health workers are concentrated in areas considered safer (largely in the central governorates) with reduced availability of skilled health workers in vulnerable areas in the northeast, northwest and southern parts of the country (Figures 2 and 3).
Figure 1: Distribution of public health facilities per governorate in Syria, 2018
Figure 2: Proportion of medical doctors in public health centres per governorate in 2017 and 2018
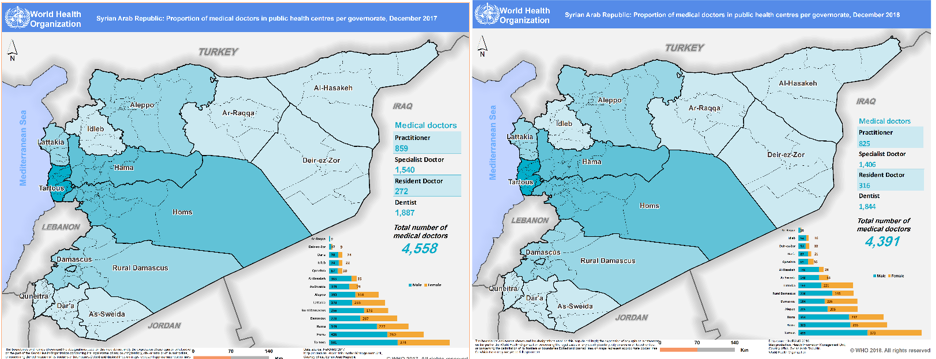
Figure 3: Proportion of medical doctors in public hospitals per governorate in 2017 and 2018
Responding to the emerging need of malnutrition
According to the Syrian Family Health Survey (2009), the nutrition situation of children under five years of age was already poor pre-crisis (23% stunted, 9.3% wasted and 10.3% underweight). Only 42.6% of infants under six months old were exclusively breastfed and only 42.2% of newborns were introduced to breastfeeding within the first hour of birth (WHO/MoH, 2009). Micronutrient deficiencies were also common pre-crisis, including prevalent anaemia (29.2%, MoH, 2011), vitamin A deficiency (8.7%, MoH 1998) and iodine deficiency (12.9%, MoH, 1998) amongst under-fives. Neonatal mortality rates, infant mortality rates and under-five mortality rates stood at 12.9/1000, 17.9/1000 and 1.4/1000 respectively. Pre-crisis, severe acute malnutrition (SAM) was managed in paediatric departments in some main referral hospitals. Community-based management of acute malnutrition (CMAM) services have since been established to cater for increased crisis-related burden. Supplementary feeding programmes (SFPs) and outpatient therapeutic feeding programmes (OTPs) are now co-located in 86 centres across the country, managed by the World Food Programme (WFP) and the United Nations Children’s Fund (UNICEF), respectively. Twenty-three stabilisation centres (SCs) for complicated SAM cases are based in public hospitals, supported by the World Health Organization (WHO).
Development of a nutrition surveillance system (NSS)
Prior to the conflict, a national NSS reported cases of acute and chronic malnutrition among children under five years old visiting health facilities for routine immunisations (targeting all children under five years – an estimated 2.7 million children). This service was intended to provide parents with information on their child’s growth through routine monitoring. After the onset of the crisis, concerns regarding increased risk of malnutrition and poor case detection led to a pilot surveillance system in 2014, building on existing growth-monitoring services at 115 health facilities. This was later transformed into an emergency nutrition NSS which, by 2018, covered 802 health centres (WHO Syria Annual report, 2018). The purpose of the NSS is to detect children with acute malnutrition for referral to management services at treatment centres. Global acute malnutrition (GAM) and other nutrition data are collected from public health centres and collated into national consolidated reports to inform evidence-based planning, forecast needs and evaluate programme impact. As children who attend centralised and decentralised health centres in multiple governorates for routine immunisations are monitored (except for inaccessible areas such as Idleb and parts of rural areas of Deir-ez-Zor and Raqqa), GAM rates through surveillance data are considered fairly representative of the country as a whole. Service coverage rates are not currently measured.
Pilot NSS system
The pilot initiative began in early 2014, in collaboration with the Ministry of Health (MoH), United Nations (UN) agencies and national non-governmental organisations (NGOs). The agreed logical approach was to adapt the existing NSS based on growth monitoring in selected health centres in 12 governorates. Adaptations included revised reporting and monitoring tools and training for health workers. The pilot governorates were selected using two criteria: (i) conflict-impacted areas (Daraa, Homs, Aleppo, rural Damascus, Idlib, Quneitera and Deir-ez-Zor); and (ii) densely populated areas with high numbers of internally displaced persons (IDPs) (Damascus, Tartous, Latakia, Hama and Sweida). In the selected health centres, coverage rates of nutrition surveillance, capacity of human resources, availability of physical space and equipment needs were assessed and gaps filled. Nutrition surveillance was also restarted in the highly conflict-affected governorate of Ar-Raqqa through the coordinated efforts of WHO field staff. Many constraints were reported by selected health centres during the pilot period, including lack of human resources, space, equipment and telecommunication-reporting utilities. These obstacles were especially evident in the case of Deir-ez-Zor, a significantly under-staffed and under-resourced area of the country. Despite these challenges, by the end of 2014, 115 health centres were integrated into the pilot NSS, covering 50,000 beneficiaries.
Countrywide NSS system – data and methods
Following the success of the pilot, the system was expanded to additional health facilities from 2015 onwards until, by the end of 2018, 802 health centres were included, screening a total of 928,000 children during 2018 (Figure 4). Of these children, 40% were aged under six months; 16.5% 6-12 months; 19% 12-24 months; and 25% 24-59 months. All children who attended the clinic were included in screening, including those who attended for immunisations and those seeing treatment for sickness. The NSS collects data on weight and height (to assess wasting and stunting), oedema, mid-upper arm circumference and on exclusive breastfeeding (maternal report). Cases of moderate acute malnutrition (MAM) are referred to SFPs, uncomplicated SAM to OTPs and complicated cases of SAM to SCs. WHO has worked closely with the MoH, UNICEF and WFP (co-members of the Nutrition Cluster) to strengthen communication channels between different levels of care to ensure quality referral services. In 2018, 848 complicated cases were referred to SCs and 905 cases admitted; this suggests that the referral system is working.
Data was initially entered manually on paper-based registries, submitted monthly by health centres to district level for collation and submission to Damascus. However, data quality was limited by human errors and a cumbersome (delayed) process. To address this, from 2017, monitoring, reinforced trainings, user-friendly Excel spreadsheets and computerised reporting were implemented at district and central levels. Reporting formats were improved further in 2018 to differentiate between new and returning cases in order to strengthen the quality of data, treatment and follow-up. Since mid-2017, infographics such as those presented in Figure 5 are published on a regular basis to aid communication.
Figure 4: Map of nutrition surveillance centres, 2018
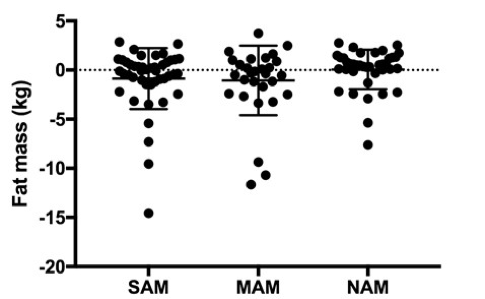
Figure 5: Infographic presenting data from the NSS, 2018
Engaging NGOs and the private sector
In areas where health services were severely disrupted, additional partners were needed to undertake nutrition screening. As a result, surveillance training was expanded to local NGOs able to perform screening in Homs, Aleppo, Hama, Hassakeh, and Raqqa in areas receiving large influxes of IDPs. Training was also provided to 30 private doctors in 2016 and 175 doctors in 2018 in eight governorates (Damascus, rural Damascus, Homs, Aleppo, Latakia, Tartous, Sweida, and Hama) in collaboration with the Paediatric Society. In Aleppo alone, 878 children were screened by private doctors in 2018. Of these, one was found to have complicated SAM, 12 uncomplicated SAM and 54 MAM.1 All cases were referred to the public health system for treatment.
Reaching the most vulnerable with nutrition screening
In situations such as the East Ghouta evacuation, the Raqqa offensive, or the latest displacement from Hajin and Baghouz in Deir-ez-Zor, hundreds of thousands of people who had been suffering from long-term food insecurity with limited access to health services, water and hygiene, arrived in informal settlements or camps needing urgent support. Among them, children under five years old were at particularly high risk of malnutrition. In response, mobile teams were established, made up of NGO or MoH staff or trained members of the local community, to rapidly screen all children on arrival and refer identified cases of malnutrition for management. A total of 46 mobile teams have been supported by WHO to rapidly screen over 128,000 children in 2018, including in East Ghouta, (70,000 children) Aleppo (4,500 children), Hassakeh (7,000 children), Daraa (26000 children), Quneitera (10,000) and Homs (10,000 children). WHO worked closely with UNICEF to share identified cases and UNICEF deployed mobile teams to provide CMAM services, with complicated SAM cases referred to the nearest SC. Among those screened, GAM prevalence was 12% (1% SAM and 11% MAM) and 30% of children were identified as stunted (higher than the national average of 2.4% in 2018).
Analysis of NSS expansion and GAM trends
Between 2014 and 2018, the number of nutrition surveillance centres expanded from 115 to 802, growing by approximately 200 health centres per year across the country (Figure 6) and increasing the number of children screened (Figure 7). In 2018, among 928,000 children screened, the prevalence of GAM was 2.4% (MAM 1.8%, SAM 0.6% and complicated SAM 0.1%); these cases were referred to SFP, OTP and SCs for treatment.
Since 2015, several approaches have been used to expand the NSS and associated treatment services, including:
- Geographical expansion through an increased number of facilities integrating nutrition surveillance to increase geographical coverage of screening.
- Capacity-building of health workers in selected health facilities on nutrition screening to increase the number of qualified health workers to undertake this activity.
- Increased availability of nutrition supplies in health centres and hospitals providing nutrition services.
- Increased monitoring and supervision of work established at facility level to help improve quality of care and nutrition services.
An improved security situation in some locations since 2015 (which increased access to facilities by beneficiaries, health workers and supporting agencies) has also facilitated surveillance and treatment. Figure 8 shows the increase in the number of health centres with integrated nutrition surveillance over time. By the end of 2018, the NSS was implemented in all governorates with the exception of Idlib, which was inaccessible from 2015, and Deir-ez-Zor, which was under ISIS control and inaccessible between 2015 and 2017.
Figure 6: Number of nutrition surveillance centres in Syria, 2014-2018

Figure 7: Number of children screened in nutrition surveillance centres, 2014-2018

(Totals rounded up to the nearest thousand)
Figure 8: Number of health centres with integrated NSS 2014-2018 by governorate

The main aim of the surveillance expansion was to ensure early detection and treatment of acute malnutrition cases. Figures 9 and 10 show that overall GAM prevalence remained within moderate limits and reduced over time from 5.25% in 2015 to 2.4% in 2018 (928,000 screened); SMART surveys found 2.5% GAM in 2015 and 1.7% GAM in 2019. Governorates such as Damascus, rural Damascus, Homs, Hama, Latakia and Tartous all showed reductions in GAM rates from 2015 to 2018, which can be explained by the stabilisation of the situation in these areas and continued humanitarian support to meet basic needs. Spikes that can be seen in Aleppo, Daraa and Hassakeh correlate to acute emergency situations, such as the evacuation in Aleppo at end of 2016, escalation of violence in Daraa mid-2018 and the massive displacement of people in Raqqa and Deir-ez-Zor to Hassakeh in mid-to-late 2018. As people moved from long-term besiegement or fled from violence to safer or more accessible areas, screening improved and the reporting of malnourished children consequently increased. In the cases of Hassakeh, Ar-Raqqa and Deir-ez-Zor that were under ISIS control prior to 2017, NSS did not expand as planned until later (2018-2019), when more NSS centres were activated.
Factors that likely contributed to the reduction of GAM in certain governorates include the implementation of the NSS system enabling early detection and referral; raised awareness among mothers of child health and malnutrition; strong infant and young child feeding interventions at health centre and community level by various nutrition partners; the improved food security situation; close management of SAM and MAM cases within the CMAM system, with follow-up at health centres and hospitals; improved security situation; and better living conditions.
Figure 9: GAM prevalence identified through surveillance by governorate, 2015-2018

Figure 10: GAM prevalence identified through surveillance in Syria 2015-2018

Development of treatment services for acute malnutrition
Complicated case management
Prior to the crisis, the MoH took the lead on most nutrition-related initiatives and WHO provided technical guidance on growth monitoring and infant and young child feeding initiatives (e.g. the International Code of Marketing of Breastmilk Substitutes and the Baby-friendly hospital initiative). During the crisis, WHO took the lead in both nutrition surveillance and management of complicated SAM together with the MoH, NGOs and health partners. To manage complicated SAM, from 2014, WHO supported the establishment of 10 SCs within the paediatric departments of main public hospitals; additional SCs were established in private hospitals and implemented by NGOs where public services were too badly damaged or inaccessible (Figure 11). WHO supported SCs with capacity-building of the health workforce (training 350 health in SAM management protocols to date); providing medicines, medical supplies and equipment for treatment of complicated SAM (e.g. anthropometric equipment, antibiotics, minerals, vitamins and F100, F75 formulas); and providing technical support for treatment protocols and reporting. Referral rates demonstrate strong complementarity of programmes; by 2017 all cases of complicated SAM referred to SCs were admitted, compared to 60% of cases in 2015. Furthermore, with continued capacity-building and support, programme implementation and quality has improved, reflected in reduced mean length of stay at hospital from 12 to approximately 6 days and reduced mortality from 9% to 2.2% in four years (Figures 12 and 13). This demonstrates high efficiency and quality of service.
Figure 11: Location of SCs in Syria, October 2018
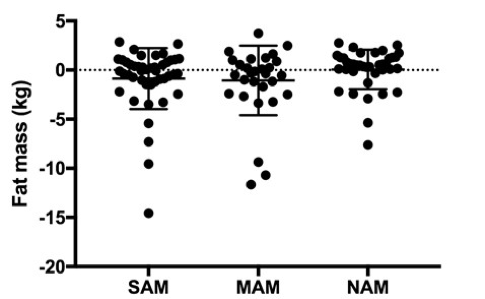
Figure 12: Mean length of stay in SCs, 2015-2018

Figure 13: Mortality rate among complicated SAM cases at SCs, 2015-2018 (based on a total of 905 cases over the period)

Uncomplicated case management
UNICEF and WFP have supported public health centres to provide outpatient nutrition services to manage uncomplicated SAM and MAM cases using the CMAM approach. Outpatient centres have expanded over time across the country and there is good complementarity between the NSS and inpatient and outpatient programmes, with referrals regularly happening between them.
Co-planning of services
Surveillance data, together with SMART survey data, are heavily relied on to estimate annual targets and caseloads to support WHO, UNICEF and WFP acute malnutrition programming. Implementation and linkages between SFPs, OTPs and SCs are managed by nutrition officers in MoH who have oversight of MoH activities at different levels and who play an important role in planning for expansion and deciding where new services are needed.
Conclusions
Transforming the existing growth-monitoring system into an NSS has had tremendous value in the timely detection and management of acute malnutrition in Syria. A strong network of trained health workers has been established and health facilities have been equipped to provide quality services for screening and case management. This has complemented interventions supported by UNICEF and WFP and has paved the way to strengthen CMAM interventions. Data provided by the NSS has enabled MoH, WHO, UNICEF and WFP to plan and design appropriate interventions and has provided vital information for country-level planning; for example, for the annual humanitarian needs overview and the humanitarian response plan, which are used to advocate for funds for the emergency response. NSS data has revealed a reduction in GAM rates since 2015; a trend consistent with SMART survey data. This suggests an improvement in the overall nutrition situation in the country and points to the benefits of quick referral, timely management of acute malnutrition cases identified, and complementary service provision. However, besieged populations remain highly vulnerable; mobile services proved a successful approach to cater immediately for those displaced from inaccessible areas and securing humanitarian access remains a priority concern.
Future plans for the NSS are to increase screening coverage. Based on the immunisation target of 2.77 million children under five years old, just one third are currently screened for acute malnutrition, so there is room to go further. Other ambitions of WHO and MoH are to integrate surveillance services into all functional health centres and improve coverage of children in health facilities already within the NSS. Integrating NSS into health information system online platforms is also required to move health facilities from paper-based systems to further improve quality and timeliness of data. Moreover, with the slow shift to early recovery in parts of the country, the expectation is for the system to move towards routine growth monitoring (while continuing to report on acute malnutrition to inform the services still provided) with a renewed focus on stunting and other ongoing nutrition concerns, such as micronutrient deficiencies.
For more information please contact Mahmoud Bozo.
Endnotes
1There was no additional charge for this service above normal patient fees charged by the private clinics.
References
HeRAMS Annual Report-January-December 2018a - Public Hospitals in Syrian Arab Republic. http://applications.emro.who.int/docs/syr/CoPub_HeRAMS_annual_rep_public_Hospitals_ 2019_EN.pdf?ua=1
HeRAMS Annual Report- January-December 2018b -Public Health Centres in Syrian Arab Republic. http://applications.emro.who.int/docs/syr/CoPub_HeRAMS_annual_rep_public_health_2019 _en.pdf?ua=1
Ministry of Health, Nutrition surveillance system report, Syria, 2011.
Ministry of Health, Vitamin A deficiency Study, MoH, 1998
WHO/MOH. Syrian Family Health Survey, Syria, 2009