Adaptations to CMAM programming in Cox’s Bazar in the context of the COVID-19 pandemic
By Tracy Dube, Mary Chelang'at Koech, Piyali Mustaphi, Sandra Harlass, Jessica Bourdaire and Karanveer Singh
Tracy Chiridza Dube is a Public Health Nutritionist, currently working as Programme Officer for the World Food Programme (WFP) Bangladesh Mission based in Cox’s Bazar. She has worked in both emergency and development contexts at national and international level for over ten years, including in Zimbabwe, Liberia, Ethiopia, South Sudan, Nigeria and Iraq.
Mary Chelang'at Koech is Nutrition Officer for United Nations High Commissioner for Refugees (UNHCR) Cox’s Bazar sub office supporting the nutrition and food security programmes. She has experience working in nutrition for 12 years in Kenya Rwanda, Tanzania, Ethiopia and Bangladesh.
Piyali Mustaphi is Chief of Nutrition section in Bangladesh Country office, overseeing both development and emergency nutrition programmes. She has 28 years of experience as a public health nutritionist, 22 years of which have been with United Nations Children’s Fund (UNICEF), with experience working in multiple countries across the South Asia; East and Southern Africa; and Middle East and North Africa regions.
Sandra Harlass is a public health specialist currently working as senior public health officer with UNHCR in Cox's Bazar, overseeing the health and nutrition programme. She has worked in public health for the past 18 years in different countries in Africa, Asia and Europe.
Jessica Bourdaire is a Nutrition Specialist at the Nutrition Division of WFP Headquarters. She has been working in public health and nutrition for 12 years primarily in emergencies across Africa and Asia.
Karanveer Singh is a child health and nutrition medical professional currently working as Nutrition Manager in UNICEF Cox’s Bazar. He has worked as a clinician and in humanitarian and development programmes for over 30 years in India, South Sudan, Yemen and Bangladesh.
We thank the Government of Bangladesh for its willingness to host the refugees and for providing humanitarian space for the Cox’s Bazar response and the Nutrition Sector and all its member for contributing to the successful implementation of nutrition programmes in Cox’s Bazar. Special thanks go to Bakhodir Rahimov, Nutrition Sector lead, for his technical support in the drafting this document and Abid Hasan, Nutrition Sector Information Management Officer, for providing data and information referenced in this article. We also acknowledge our colleagues at headquarters, regional bureaus and country offices including Britta Schumacher, James Kingori, Kerstin Hanson, Deborah Wilson and Gwenaelle Garnier from WFP; Valerie Gatchell from UNHCR; and Harriet Torlesse, Zivai Murira and Golam Mohiuddin Khan from UNICEF for their technical support and advice as well as our various donors for their outstanding financial support that has enabled us to successfully treat and prevent acute malnutrition in Cox’s Bazar. In addition, we thank our staff for their hard work, energy and resilience in the face of COVID-19 and the people of Cox Bazar for their generosity in hosting the refugees and humanitarian workers. Last but not least, we thank the refugees we serve for the confidence they have placed in us, and for playing an active role in the provision of integrated nutrition services.
Location: Cox’s Bazar, Bangladesh
What we know: The COVID-19 pandemic has had a widespread impact on nutrition programmes; wasting management programmes have had to adapt to ensure the continuation of services.
What this article adds: Wasting management services in Cox’s Bazar Rohingya camps, coordinated by the Government of Bangladesh and the United Nations Children’s Fund-led Nutrition Sector, have continued in the COVID-19 context with adaptations to reduce the risk of the transmission of the virus. Adaptations have included use of mid-upper arm circumference (MUAC) only for the screening, admission, follow up and discharge of children aged 6-59 months, the increasing of MUAC thresholds (to <120 mm for severe wasting and ≥120 mm and <135 mm for moderate wasting) to reduce the number of children missed for treatment, Mother-led MUAC for screening supported by camp volunteers, the integration of screening into the vitamin A supplementation campaign, the doubling of rations and reduced frequency of visits to Integrated Nutrition Facilities (INFs) to reduce contact, Infection Prevention Control (IPC) measures at INFs, the remote training and supervision of staff and volunteers and remote programme monitoring. The rapid implementation of adaptations was helped by the pre-existing coordination of stakeholders and emergency preparedness plans, strong communication between Nutrition Sector partners and INFs, a stock of ready-to-use therapeutic food (RUTF) supplies and the quick adoption of innovations. A challenge has been the large increase in caseload of moderately wasted children due to the increase in MUAC thresholds. This is being investigated.
Background
Cox’s Bazar is a coastal district in Bangladesh that is one of the most impoverished areas of the country. This district is also home to one of the world’s most protracted refugee situations where, since the early 1990s, a Muslim minority group from Myanmar’s northern Rakhine State, known as Rohingyas, have settled in camps and makeshift site settlements in the area. In August 2017, there was a major influx of 700,000 Rohingya people into Cox’s Bazar, placing considerable pressure on already scarce natural resources and livelihood opportunities. Today, Cox’s Bazar’s Ukhiya and Teknaf subdistricts hold more than 800,000 registered and unregistered Rohingya refugees in 34 demarcated camps.
The Nutrition Sector, operating under the Inter Sector Coordination Group (ISCG), is co-led by the Government of Bangladesh and United Nations Children’s Fund (UNICEF). Nutrition Sector membership is comprised of implementing partners (non-governmental organisations (NGOs)) who work in partnership with and receive financial, logistical and technical support from various stakeholders including UNICEF, the World Food Programme (WFP) and the United Nations Children’s Fund (UNHCR). The Nutrition Sector aims to ensure a well-coordinated and integrated nutrition response in Cox’s Bazar that prevents and treats malnutrition in children under five years of age and related morbidities. Nutrition services are largely delivered through 45 integrated nutrition facilities (INF) (Box 1).
Box 1: Integrated nutrition facilities (INF) - progress in delivering continuity of care
Prior to 2020, nutrition services were delivered at 106 different sites across the Rohingya camps with little or no integration. In each camp, these nutrition services were supported by different United Nations (UN) agencies and implemented by different implementing partners (NGOs). This led to considerable overlaps, gaps and duplication of both services and target beneficiaries.1 The Nutrition Sector undertook a rationalisation exercise in 2020 to address these challenges which resulted in reorganising nutrition services at 45 integrated nutrition facilities (INFs) across 34 camps.
INFs provide comprehensive nutrition services targeting children under five years and pregnant and lactating mothers. These include community-based management of acute malnutrition (CMAM) services (outpatient therapeutic programmes (OTPs) and targeted supplementary feeding programmes (TSFPs)), blanket supplementary feeding programmes (BSFPs), social and behaviour change communication (SBCC) on infant and young child feeding (IYCF) and maternal health and nutrition and other nutrition-sensitive programmes.
The management of children with severe acute malnutrition (SAM) is supported by UNICEF in 20 camps and UNHCR in 14 camps. The World Food Programme (WFP) supports the management of children and pregnant and lactating women/girls (PLW/G) with moderate acute malnutrition (MAM) across all 34 camps. In the 20 camps where both UNICEF and WFP are supporting services, the same implementing partner is being used and the staff structure, salaries and layout of the centres have been jointly agreed to help to reduce the possibility of one person benefiting twice from the same service (e.g. by being admitted in two or more treatment sites). In the 14 camps where services are supported by UNHCR and WFP, implementing partners are engaged through a tripartite agreement based on a global memorandum of understanding (MOU) between UNHCR and WFP.
In the INFs, SAM children are treated to full anthropometric recovery (mid-upper arm circumference (MUAC) â¥125mm for two bi-weekly consecutive visits). The TSFP only treats children enrolled as MAM from the outset. Children with severe acute malnutrition (SAM) and medical complications are treated in five stabilisation centres (SC) within the camps. WFP and UNICEF also support nutrition programmes in the host population in the surrounding subdistricts.
Disruptions to nutrition programming as a result of the COVID-19 pandemic
The first COVID-19 case was recorded in Bangladesh in mid-March 2020 in Dhaka. By 16 August 2020, the number of COVID-19 patients passed 276,500 including 79 cases in the Rohingya camps. At this point, Bangladesh ranked 16th globally in terms of the total number of positive COVID-19 cases. A national taskforce, which includes the UN mission in Bangladesh, was set up in March to support the government’s response to the pandemic with sub-committees at divisional and district levels. On 22 March, Bangladesh declared a 10-day shutdown effective from 26 March to 4 April which was extended and reviewed as the pandemic unfolded. To curb infections, and as part of the response plan agreed on by the taskforce and especially for Cox’s Bazar, all flights and public transport to and from the district were stopped, hotels were closed and no tourists allowed and curfew and strict travel restrictions were put in place (including a 14-day quarantine for people coming from other parts of the country and restriction of travel into the camps). Measures were kept in place until the last week of July 2020 after which they were gradually relaxed.
The restrictions, which coincided with the start of the monsoon season (a period of increased risk of undernutrition), had a major impact on the continuation of nutrition programming in the camps. In particular, there were restrictions on the number of nutrition programming staff entering camps (including those working in integrated nutrition facilities (INFs)) and the cessation of all community and group-based activities. Agencies were requested to classify all humanitarian work within the camps as either critical or non-critical. The UN agencies advocated with the Inter Sector Coordination Group (ISCG) and the Government of Bangladesh to ensure that curative nutrition services were classified as critical (including outpatient therapeutic programmes (OTPs), targeted supplementary feeding programmes (TSFPs), blanket supplementary feeding programmes (BSFPs), stabilisation centres (SC) and infant and young children feeding in emergencies (IYCF-E). Social and behaviour change communication (SBCC) activities, including nutrition education and community support groups, and growth monitoring activities were put on hold to reduce the risk of infection. While community-based management of acute malnutrition (CMAM) services were able to continue, several adjustments had to be made to ensure the safety of beneficiaries and staff and effective infection prevention control (IPC) within the INFs. These changes were guided by the guidance issued by UNICEF, Global Nutrition Cluster (GNC) and Global Technical Assistance Mechanism for Nutrition (GTAM) on 27 March 20202 and are described in this article.
Adaptations made to community-based management of acute malnutrition (CMAM) programme in the COVID-19 context
Mid-upper arm circumference (MUAC)-only programming
As part of COVID-19 preparedness activities, nutrition programmes were reviewed and evaluated to identify potential infection risk points. One potential risk factor identified was the diagnosis of acute malnutrition using weight-for-height z-scores (WHZ). With guidance from technical advisors of all three UN agencies at headquarter, regional and country levels, and in line with global recommendations,3 the Nutrition Sector agreed to adopt MUAC-only plus oedema for the screening, admission, follow-up and discharge of children aged 6-59 months in all CMAM programming within the camps. A local decision was made by Nutrition Sector partners to increase MUAC thresholds, influenced by the results of routine Cox’s Bazar SMART survey results, which demonstrated poor concordance between MUAC and WHZ, with some children with a MUAC as high as 135 mm identified as acutely malnourished using WHZ. To ensure that no children were missed, final MUAC cut-offs were agreed to be <120 mm for outpatient therapeutic programmes (OTPs)3 and â¥120 mm and <135 mm for targeted supplementary feeding programmes (TSFPs).
After an initial significant decrease in admissions to OTPs and TSFPs during March and April, admissions subsequently increased from May onwards (Figures 1 and 2). TSFP admissions were three times the level in June 2020 (9,347) compared to March 2020 (3,038 admissions). Discussions to review the cut-off points for moderate acute malnutrition (MAM) have since begun and will be concluded shortly to inform a decision on the appropriate MUAC cut-offs to be used for admission and discharge.
Mother-led MUAC for screening
After COVID-19 containment measures (March-August) were put in place in the camps, there was a drastic reduction in CMAM screening of children aged 6-59 months especially from March to April. This was partly attributed to fear of transmission by mothers who, as a result, refused household access to community nutrition workers (CNWs) to conduct nutrition screening. This contributed to the decrease in number of admissions to OTPs and TSFPs during March and April. To increase the number of children being screened every month, the Nutrition Sector made the decision to build the capacity of mothers/caregivers (May/June) to use MUAC tapes to measure their own children independently. Mothers were trained on a one-to-one basis at the integrated nutrition facilities (INFs) by the Nutrition Sector staff. The UN agencies procured enough MUAC tapes to ensure that each mother had one for her household. Due to limited access to the camps by the nutrition staff residing outside the camps, Rohingya Nutrition Volunteers were recruited and deployed to train and support mothers to conduct Mother-led MUAC on a one-to-one basis.
Supply issues and rations
In order to reduce the frequency of visits and crowding at the centres, rations of therapeutic and supplementary food were doubled and the frequency of visits halved (from weekly to bi-weekly for OTP and bi-weekly to monthly for TSFP). Given that weight measurements were not taken due to using MUAC-only, the ready-to-use therapeutic food (RUTF) ration size was modified so that, instead of issuing rations based on the child weight reference chart (as per national protocols), all severe acute malnutrition (SAM) children aged 6-23 months were issued with two sachets of RUTF and all SAM children aged 24-59 months were issued with three sachets of RUTF per day for 14 days. To ensure no pipeline breaks of RUTF in the case of a sudden lockdown of the camps, every INF was provided with a two-month supply of RUTF.
There were no alterations in TSFP rations for children (one sachet of ready-to-use supplementary food (RUSF)/day). Double rations were also provided less frequently for pregnant and lactating women in both the TSFP and blanket supplementary feeding programme (BSFP) and vegetable oil was omitted to protect the ration from rancidity due to longer anticipated storage time before consumption. In June, a temporary break in the pipeline of Super Cereal led to substitution with Super Cereal plus.
To further decongest nutrition sites, BSFP distribution was shifted from the INFs to General Food Assistance (GFA) distribution points from June. Super Cereal is now being distributed to all households to provide extra nutrients to boost immunity. Now that most sectors are re-opening, discussions are currently underway about moving BSFP back to the INFs.
Infection prevention and control (IPC) measures
Since the beginning of the pandemic, the Nutrition Sector has worked to improve infection prevention control (IPC) measures at INFs. Measures have included the installation of additional handwashing points at the entrance of each nutrition centre, mandatory handwashing and temperature screening for children and caretakers on entry, the provision of basic personal protection equipment (PPE), including masks, to staff, ensuring hand hygiene after each beneficiary, regular disinfection of sites and equipment according to Nutrition Sector guidelines and ensuring physical distancing within the centres. In addition, the decision was made not to use biometrics for registration for OTP/TSFP (which prior to the pandemic have been used for camp registration and registration for food assistance) to minimise the risk of COVID-19.
The UN agencies unanimously approved activation of emergency preparedness budget lines in the partners’ budgets for the procurement of necessary additional supplies to support IPC measures. Some supplies, such as infrared thermometers and MUAC tapes, were purchased centrally by UN agencies and distributed to partners and others were procured locally in Bangladesh by partners directly.
Messaging
Social and behaviour change communication (SBCC) and growth monitoring activities were not identified as critical interventions, therefore they have been put on hold for the time being. Messaging on COVID-19 and changes to nutrition programmes have been broadcast using megaphones and radio as well as through written posters, word of mouth at INFs and General Food Assistance (GFA) sites and via tom-tom drivers recruited by the World Food Programme (WFP). Infant and young children feeding (IYCF) counselling is provided to mothers and caregivers on a one-to-one basis at the centres, respecting social distancing.
Preparation for treating children with SAM and COVID-19
In addition to updating emergency preparedness documents, a Standard Operating Procedure (SOP) on programming during the COVID-19 response was developed. Three specialised COVID-19 treatment facilities called SARI ITC (severe acute respiratory infection isolation and inpatient treatment centres) equipped to function as stabilisation centres were established to treat children with SAM and COVID-19 as well as breastfeeding mothers with COVID-19 and elderly people with COVID-19 and SAM (MUAC <18.5 cm). Screening and referral pathways were also developed for suspected children/caregivers with COVID-19 from centres to the designated health facilities. To date, no cases of SAM with suspected COVID-19 have been transferred or treated within SARI ITCs.
Integration with other nutrition services
Mass vitamin A supplementation campaigns for children have been modified in the context of the COVID-19 pandemic. A key modification has been the integration of mass screening of children for acute malnutrition within this campaign through the use of a separate MUAC tape for each child and IYCF messaging. The details of this experience are shared in a separate article in this edition of Field Exchange.4
Remote training, supervision and monitoring
Training and support on COVID-19 prevention and CMAM programme adaptations are being provided to partners and staff through online training platforms (e.g., Zoom and Microsoft Teams). Pre-COVID-19, UNICEF had an agreement with CARE International to provide technical support to implementing partners. During COVID-19, in the light of limitations on the number of staff entering the camps per agency, CARE International, who are not implementing any nutrition programmes, was tasked with the role of independent programme monitoring. Monitors from CARE pay regular visits to INFs supported by UNICEF and WFP and monitor remotely using mobile phones. Ongoing weekly calls are also made by UNICEF Emergency Nutrition Officers to each INF supervisor to collect information on the functioning of the INF, the staff present and the stock position. During these calls, information is collected randomly from two mothers present at the INF at the time of the call, including access to the INF, services being provided and access to, availability and cost of fresh food in the market.
Outcomes so far
After an initial significant decrease in admissions to outpatient therapeutic programmes (OTPs) and targeted supplementary feeding programmes (TSFPs) during March and April, a subsequent increase in admissions was observed (Figure 1) with TSFP admissions in June 2020 (9,347) three times higher than in March 2020 (3,038). A similar pattern was also seen for OTP admissions. As discussed above, the initial dip in admissions was likely due to lockdown measures and fear of transmission in accessing services. The subsequent rise in admissions coincides with the integration of acute malnutrition screening within the vitamin A supplementation campaign (June to July 2020) which enabled a high coverage of screening.5 The increase in admissions from May onwards also coincides with the building of mother/caregiver capacity to take mid- upper arm circumference (MUAC) measurements at home; between April and July 2020, 3,669 children aged 6-59 months with a MUAC <135 mm were referred by the 82,921 mothers trained to use MUAC.
Programme outcomes for OTPs and TSFPs remained relatively stable over this period (Tables 1 and 2). It is not possible to compare 2020 outcomes with previous years given the difference in treatment sites (non-integrated sites previous to 2020) as well as the changes in admission and discharge criteria and MUAC cut-off thresholds in 2020.
Figure 1: Trends in admissions to OTP and TSFP from January to July 2020
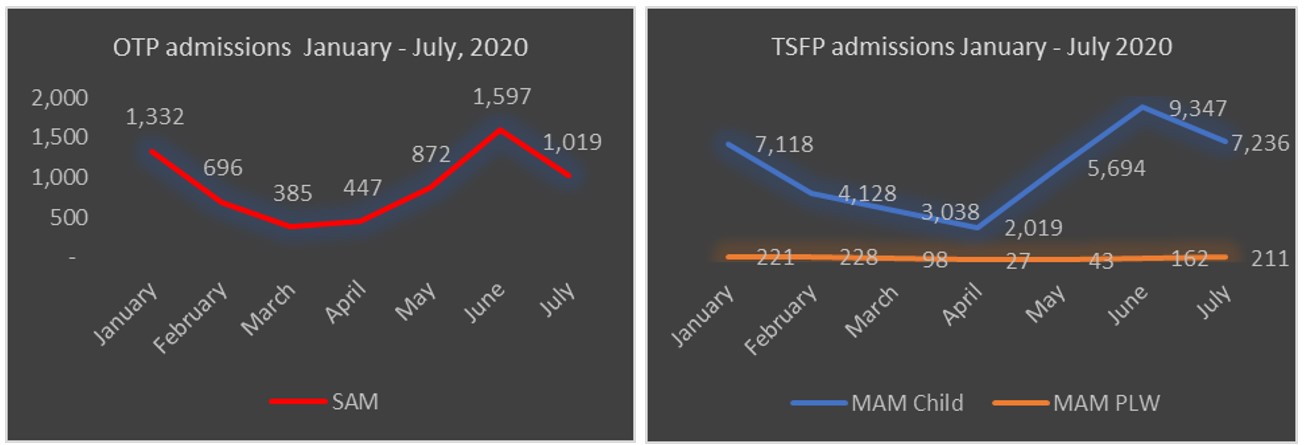
Table 1: Programme outcomes for OTPs in Rohingya camps in Cox’s Bazar April to July 2020
| SAM 2020 | ||||||
| Month | Cured (%) | Defaulter (%) | Death (%) | Non-response (%) | Average length of stay (days) | Average weight gain (kg) |
| April | 89.99% | 0.57% | 0.14% | 9.30% | 69.53 | 3.11 |
| May | 84.80% | 0.19% | 0.00% | 15.01% | 66.29 | 2.85 |
| June | 86.95% | 0.25% | 0.25% | 12.56% | 68.20 | 2.92 |
| July | 93.44% | 0.11% | 0.11% | 6.34% | 67.93 | 2.90 |
Table 2: Programme outcomes for TSFPs in Rohingya camps in Cox’s Bazar April to July 2020
| MAM 2020 | ||||||
| Month | Cured (%) | Defaulter (%) | Death (%) | Non-Response (%) | Average length of stay (days) | Average weight gain (kg) |
| April | 91.69% | 0.97% | 0.22% | 7.12% | 74.99 | 1.85 |
| May | 84.09% | 0.68% | 0.00% | 15.23% | 86.27 | 1.61 |
| June | 76.12% | 0.48% | 0.10% | 23.30% | 101.22 | 1.59 |
| July | 85.18% | 0.28% | 0.23% | 14.31% | 95.39 | 1.82 |
No cases of severe acute malnutrition (SAM) with COVID-19 were admitted to severe acute respiratory infection isolation and inpatient treatment centres (SARI ITCs) which had a low overall bed occupancy. A total of 162 acutely malnourished children with suspected COVID-19 were referred from 27 UNICEF and WFP run integrated nutrition facilities (INFs) to health facilities but none of these tested positive. Around 185 mothers were asked questions via weekly mobile phone remote monitoring between June and mid-August. Of these mothers, 70% reported feeding less diverse food to their children, 53% reported feeding less food to their children and 45% reported food shortages within their households since the onset of the pandemic.
Lessons learned
Pre-existing coordination and collaboration between stakeholders and emergency preparedness plans prepared the way for the continuation of nutrition programming
Preparedness is critical. The existing strong coordination and collaboration between the three UN agencies and solid Nutrition Sector leadership during the COVID-19 response enabled a quick response to the changing situation and the uninterrupted implementation of nutrition services over this period, albeit with adaptations. Prior to the outbreak of COVID-19, the Nutrition Sector had an emergency preparedness document in place that only required updating to the COVID-19 context, rather than writing from scratch. This guided the response. UN partnerships with non-governmental organisations (NGOs) had emergency lines embedded within their budgets and this helped a quick turnaround when the need to procure COVID-19 related resources arose. The need to have these emergency budget lines was adopted from prior experience in responding to the monsoon floods.
Strong communication between integrated nutrition facilities (INFs) and the Nutrition Sector and ongoing monitoring enabled a quick response to challenges
Continued communication and routine information exchange between the Nutrition Sector and INFs enabled the prompt development of contextualised technical guidance and targeted capacity building of partners, allowing nutrition programming to continue. Use of an independent monitoring agency (CARE International) to monitor the implementation of programme adaptations and infection prevention control (IPC) measures also helped to identify gaps for early corrections. Challenges observed by monitors related to difficulties switching to mid-upper arm circumference (MUAC)-only admission and the use of new MUAC cut-offs, the uptake of Mother-led MUAC, the follow-up of supplementary and therapeutic food stocks both at beneficiary and at treatment site level, the implementation and maintenance of functional extra hand washing points at entry to the INFs and the respect of physical distancing. As a result of this information, it was possible to provide support and capacity building to INF staff to overcome the challenges. The use of online platforms was key in rapidly sensitising staff on protocols and disseminating information in a timely fashion. Monitoring information was also critical in tracking trends and anticipating the initial fall in admissions and to inform an effective response.
Provision of adequate stock of supplies enabled implementation of critical adaptations
The pre-positioning of adequate therapeutic and supplementary food stocks enabled programmers to increase the quantity of rations given to beneficiaries at each visit when the frequency of visits was reduced. The pre-positioning of stock has also been important to prepare for potential breaks in the supply chain in the case of sudden lockdowns.
Raising MUAC thresholds has raised the level of admissions of children with moderate acute malnutrition (MAM) which has programming implications
The MUAC cut-off point of <135 mm for referral to TSFP seemed too high, given the observed sharp increase in MAM caseloads. The situation was closely monitored and the MUAC cut-off point adjusted to <130 mm, from the 1 September 2020, following the anthropometric data analysis of 20% of children admitted in targeted supplementary feeding programmes (TSFP).
The rapid application of programme innovations enabled services to continue
It was important to consider all available opportunities to reach the community and embrace innovations. For example, the vitamin A supplementation campaign provided an opportunity for the screening of children for acute malnutrition and to communicate messages on infant and young child feeding (IYCF) focusing, for example, on violations of the Breastmilk Substitutes (BMS) Act. In addition, tom-tom drivers were used for social and behaviour change communication (SBCC). Other examples are the rapid recruitment and use of volunteers within the Rohingya community to support nutrition programming when staff were unable to enter the camps due to movement restrictions, the recruitment of an independent monitoring mechanism to identify gaps and the use of technology to enable remote communication with staff. These innovations were critical in enabling the continuation of nutrition services in the camps.
Conclusions
Programme adaptations remain in place at the time of writing. COVID-19 is present within the camps at a low level but the true situation is unknown due to limited testing. Although nutrition services are ongoing, the inability to implement all routine nutrition services has disadvantages. One example is the removal of the mid-upper arm circumference (MUAC) screening of children in blanket supplementary feeding programme (BSFP) services, since BSFPs were moved from the integrated nutrition facilities (INFs) to the General Food Assistance (GFA) platforms to minimise people gathering which may have delayed the detection of new cases of acute malnutrition. Therefore, adaptations are continually being reviewed and changed. Transition back to routine programming will depend on the local and national COVID-19 situation and Inter Sector Coordination Group (ISCG) directives and is expected to be undertaken systematically in a phased approach through engagement of each technical coordination platform.
Some of the programme adaptations will be continued post COVID-19. They include a family led MUAC approach as a form of active case finding for severe acute malnutrition (SAM) and moderate acute malnutrition (MAM) alongside screening by community nutrition workers (CNVs) and staff at nutrition sites, the involvement of CNVs and caregivers in the promotion of engagement with nutrition services and the use of multiple platforms for social and behaviour change communication (SBCC). Another good lesson learned is the inclusion of emergency budget lines in partnership agreements even before the advent of the emergency which means that resources can readily be made available to implementing partners in times of crisis. These adaptations may be relevant in other contexts where community-based management of cute malnutrition (CMAM) is being implemented in the context of COVID-19, including in humanitarian contexts and in hard to reach areas.
The nutrition programme in the Rohingya refugee camps was able to quickly adapt to the rapidly changing, uncertain and extremely difficult programming situation as a result of the COVID-19 pandemic. This was largely due to strong technical leadership and the ownership, collaboration and coordination of Nutrition Sector partners who joined strengths and efforts and showed willingness to think ‘outside the box’ and learn and change with the evolving situation with one goal in mind - to reach every child and mother with quality life-saving nutrition services without any break.
For more information please contact Tracy Dube.
1 Read a previous Field Exchange article about this at https://www.ennonline.net/fex/62/myanmarnationalsinbangladesh
2 https://www.ennonline.net/covid19wastingbrief
3 In line with 27th March 2020 guidance from UNICEF, GNC and GTAM https://www.ennonline.net/covid19wastingbrief
4 See article in this edition entitled ‘Integrating screening for acute malnutrition into the vitamin A supplementation campaign in the Rohingya camps in the context of COVID-19’
5 See article in this edition entitled ‘Integrating screening for acute malnutrition into the vitamin A supplementation campaign in the Rohingya camps in the context of COVID-19’


