Integration of management of children with severe acute malnutrition in paediatric inpatient facilities in India
By Praveen Kumar, Virendra Kumar, Sila Deb, Arpita Pal, Keya Chatterjee, Rajesh Kumar Sinha and Sanjay Prabhu
Praveen Kumar is a paediatrician working as Director Professor at the Department of Paediatrics, Kalawati Saran Children’s Hospital (KSCH), Lady Hardinge Medical College, NewDelhi. He is also the Lead Coordinator of the National Centre of Excellence (NCoE) for severe acute malnutrition (SAM) management.
Virendra Kumar is a paediatrician working as Head of Department of Paediatrics, Kalawati Saran Children’s Hospital, LadyHardinge Medical College, New Delhi. He supervises functioning of NCoE for SAM management.
Sila Deb is an Additional Commissioner of the Child Health Division (Nutrition in charge), Ministry of Health and Family Welfare (MoHFW), Government of India, overseeing the National Child Health Programme for Child Health and Nutrition.
Arpita Pal is Nutrition Officer (Monitoring and Evaluation) at United Nations Children’s Fund(UNICEF), New Delhi. She has over 10years of experience in public health and nutrition with government and UNICEF, India.
Keya Chatterjee is a public health professional and formerly Nutrition Specialist with UNICEF. Shehas wide experience of implementing community nutrition programmes at community and facility level.
Rajesh Kumar Sinha isProgramme Manager (Senior Consultant) with NCoE, Kalawati Saran Children’s Hospital, New Delhi. Hehas around two decades of experience in research and publications on public health and nutrition and conducting economic evaluations.
Sanjay Prabhu is Senior Consultant at Bai Jerbai Wadia Hospital, Mumbai and is incharge of the Nutrition Rehabilitation Centre at the hospital.
The authors acknowledge UNICEF Delhi and National Health Mission, New Delhi for their support in running SAM treatment facilities at KSCH.
Location: India
What we know: Children with wasting in India are currently managed as inpatients in nutrition rehabilitation centres (NRCs).
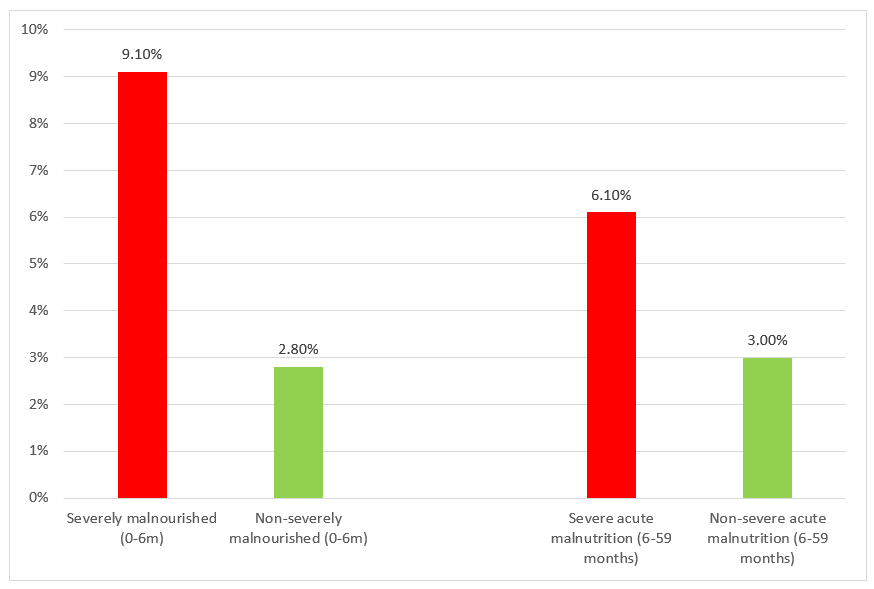
What this article adds: Due to limitations of treatment for severe acute malnutrition (SAM) in NRCs in India (lack of skilled manpower and capacity),inpatient management of complicated SAM cases was integrated into the paediatric wards of a large tertiary hospital in New Delhi. A nutritionist was stationed in each ward to take anthropometric measurements, administer therapeutic feeds and counsel caregivers. Operational research was undertaken to understand prevalence of SAM in paediatric wards, mortality rates in SAM children vs non-SAM children and observe protocol compliance. Between February 2018 and October 2019, of 3,444 admitted infants under 6 months of age (U6m), 44.8% had complicated SAM; of 6,758 children aged between 6 and 59 months, 27.6% had complicated SAM. SAM infants U6m had 3.44 times higher risk of death than non-SAM infants (9.1% vs 2.8%); SAM children aged 6 to 59 months had double the risk of death compared to non-SAM children (6.1% vs 3.0%). Challenges experienced during implementation included missed night feeds (due to less staff support at night), poor coordination of follow-up visits and lack of clear protocols for management of infants U6m. With additional staff capacity and training, inpatient management of complicated SAM can be integrated into paediatric wards in India to alleviate pressures on NRCs, increase treatment coverage and reduce SAM mortality rates.
Introduction
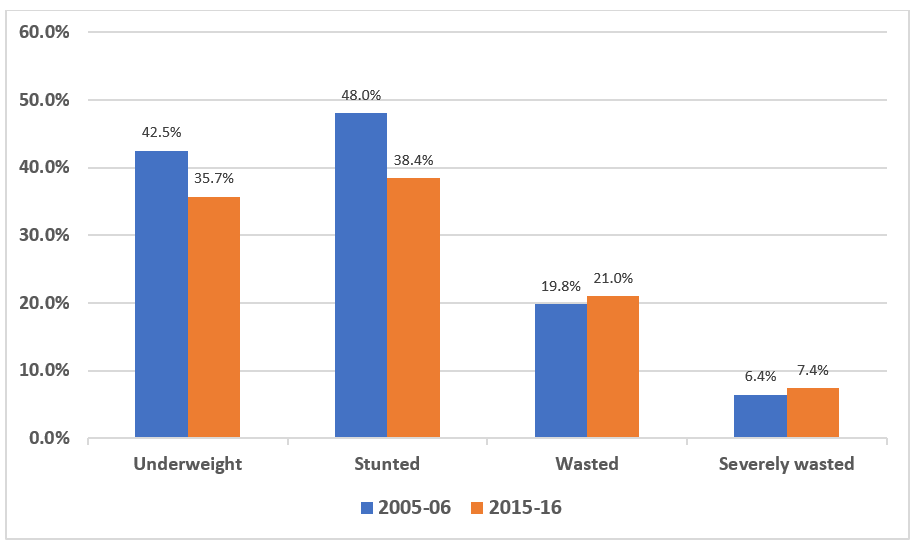
Undernutrition contributes to around two thirds of child mortality in India (Swaminathan et al, 2019), with many states across the country experiencing extremely high burdens. Progress has been made in the reduction of underweight and stunting in children under five years of age in India over the last decade, but levels of wasting have increased (Figure 1). There is an urgent need for more attention to its effective management, particularly in states with persistently high burdens.
Figure 1: Prevalence of underweight, stunting, wasting and severe wasting among children under five years old in India
Management of severe acute malnutrition (SAM) in India
SAM management guidelines
In 2007 a global joint statement was issued by the World Health Organization (WHO), World Food Programme (WFP) and the United Nations Children’s Fund (UNICEF) in support of community-based management of acute malnutrition (CMAM) to enable rapid scale-up of treatment services and prevent deaths associated with untreated SAM (WHO et al, 2007). The 1999 WHO guidelines on the management of SAM were updated in 2013 (WHO, 2013). In India, acute malnutrition management is guided by the 2007 Indian Academy of Pediatrics (IAP) and 2011 Ministry of Health and Family Welfare (MoHFW) guidelines for facility-level SAM management. These guidelines are currently being updated by the Government of India (GoI) to incorporate guidance on the management of uncomplicated SAM at community level. Ahead of this, a small number of CMAM programmes are currently being piloted in several states.1
Nutrition rehabilitation centres (NRCs)
Currently in India, complicated cases of SAM2 are treated in nutrition rehabilitation centres (NRCs) that are attached to existing inpatient paediatric facilities across all states. Children without medical complications may also be admitted at the NRCs, especially where no CMAM programs exist locally. NRCs provide management of medical complications, therapeutic feeding using locally prepared starter and catch-up diets (in place of standard F-75 and F-100), and counselling of caregivers on feeding and care practices. SAM cases receive additional routine services, including micronutrient supplementation, separately according to government guidelines (GoI, 2011).
Limitations of the NRC approach
The past performance of NRCs reveals that not all are functioning optimally. Studies suggest that, in the absence of CMAM programming, around 50 to 60% of SAM cases admitted to NRCs are medically uncomplicated, with mortality rates ranging from 0.4% to 3.5% (Aguayo et al, 2014; Aguayo et al, 2013; Singh et al, 2014). Inpatient care is expensive for the state and incurs high travel and opportunity costs for families (Puett et al, 2012; Tekeste et al, 2012). High opportunity costs for families also impact access and utilisation of NRC services. Quality of care in NRCs is often impeded by lack of paediatric oversight (particularly when NRCs are located outside of hospital premises) and lack of manpower in some states, as well as high staff attrition (Tandon et al, 2019). In practice, therefore, SAM children with medical complications are often admitted to inpatient paediatric departments, after which they are discharged home or to NRCs for further recovery.
Providing dedicated facilities for the management of its 9.5 million children under five years old with SAM (IIPS, 2017) is a huge challenge in India. An estimated 0.9 million of these cases have medical complications (assuming prevalence of complications is around 10%) and therefore require inpatient care.3 Currently, there are around 1,100 operational NRCs across the country, with bed strengths ranging from 10 to 20. Even if run at 100% bed occupancy, assuming that all admissions are complicated SAM cases with an average stay of 15 days, only around 0.4 million children can be treated annually. Thus, even in the best-case scenario, existing NRCs in India can only treat 30% to 44% of all medically complicated SAM cases. Therefore, it is imperative that some inpatient care for complicated SAM cases is offered by paediatric wards in India, alongside community-based management of uncomplicated SAM cases, to enable necessary coverage of treatment services.
Testing the feasibility of integrating management of complicated severe acute malnutrition (SAM) in paediatric wards
In response to this problem, the National Centre of Excellence (NCoE) for SAM Management, Kalawati Saran Children’s Hospital (KSCH), New Delhi, in collaboration with United Nations Children’s Fund (UNICEF) India, conducted operational research between February 2018 and October 2019. KSCH is one of the largest tertiary-care children’s hospitals in Delhi, with a dedicated paediatric emergency ward, general paediatric wards, neonatal units, intensive care units and a 12-bed NRC unit. The NRC, established in 2012, initially only provided services to children admitted directly. However, between 2013 and 2015, its services were gradually expanded to SAM children in other parts of the hospital through the provision of therapeutic feeds to children admitted to other wards. This approach evolved further so that, from 2018, a dedicated nutritionist was placed in each of the three paediatric wards to carry out anthropometric measurements of all children aged under five years within 12 to 24 hours of admission, provide therapeutic feeds and conduct counselling sessions for caregivers.
To understand the impact of this approach, operational research was carried out at KSCH between February 2018 and October 2019 to study the prevalence of SAM among all children under five years old admitted for inpatient care in paediatric wards and their outcomes in relation to nutrition status. We also documented the experiences and challenges of integrating SAM management protocols within paediatric wards.
Methods
Weight and height/length measurements were taken for each child and age established to calculate weight-for-length z score (WHZ) and weight-for-age z-score (WAZ). For anthropometric measurements, a digital weighing machine (SECA 334) with a sensitivity of 5g, a UNICEF-supplied wooden infant-cum-stadiometer and non-stretchable mid-upper arm circumference (MUAC) tapes were provided. For infants under six months of age, SAM was defined as WAZ<-3 and/or weight-for-length z-score (WLZ)<-3 and/or bilateral oedema; for children aged 6-59 months, SAM was defined as WHZ<-3 and/ or MUAC<115mm and/or bilateral pitting oedema. All SAM cases were classed as complicated, given that they were admitted to the paediatric unit on the basis of their medical condition. Children with moderate acute malnutrition (MAM) were treated for their medical complications using standard protocols and nutrition counselling was given to their caregivers as per current government guidelines. SAM cases were treated according to SAM management protocols. Mothers of SAM infants under six months of age (U6m) were provided with breastfeeding support from the ward nutritionist and the dedicated infant and young child feeding (IYCF) centre in the hospital.
All children admitted to the hospital were followed from admission to outcome (defined for this study as exited alive; discharged as cured; leaving against medical advice (LAMA); defaulted; medically transferred; or died during treatment). Cured was defined as improved medical conditions, course of antibiotics completed, age-appropriate immunisation completed, and caregivers educated on appropriate childcare and feeding. For SAM cases, weight gain of 5gm/kg/day for three consecutive days was included as an additional discharge criterion from the facility. Following discharge, caregivers were counselled to bring their child for regular follow-up in the outpatient department and to attend community growth-monitoring sessions. Discharge from follow-up occurred when the child reached MUAC â¥125mm (if admitted using MUAC) or WHZ â¥-2 (if admitted using WHZ).
Analyses were conducted to assess the overall caseload of SAM against total admissions in the study period (February 2018 to October 2019) and any difference in mortality rate between SAM and non-SAM children. Data was disaggregated by age (infants U6m and children aged 6-59 months). In addition to the quantitative study, periodical reviews were undertaken with health staff, and caregivers and the researcher’s own observations were documented. Integration experiences were also documented for Bai Jerbai Wadia Hospital in Mumbai (Box 1).
Results
All admissions for the period (n=10,214 children) were enrolled in the study, 12 of whom were excluded from the analysis due to incomplete data. Of the 10,202 (99.9%) children included, 3,444 (33.8%) were U6m and 6,758 (66.2%) were aged between 6 and 59 months. Of the infants U6m, 1,543 (44.8%) children were SAM using WLZ<-3 and/or WAZ<-3and/or bilateral oedema criteria. Among children age 6-59 months, 1,865 (27.6%) children had SAM (WLZ/WHZ<-3 and/or MUAC<115mm and/or bilateral oedema.
A total of 3,249 (94.3%) infants U6m and 6,496 (96.1%) children aged 6 to 59 months exited alive and a total of 195 (5.7%) infants U6m and 262 (3.9%) children aged 6 to 59 months died during treatment. Among those who exited alive, 85.6% (n=8732) were discharged as cured, 10.1% (n=1033) were defaulters and 4.3% (n=437) were medical referrals to other facilities. Among the 1,543 severely malnourished infants U6m (by WHZ and/or WAZ), inpatient mortality was 9.1% (n=141) compared to 2.8% (n=54) among non-severely malnourished children (Figure 2). Severely malnourished infants U6m were at 3.44 (OR 3.44, P<0.001) times higher risk of inpatient mortality compared to non-severely malnourished infants in this age group. The inpatient mortality rate of SAM children aged 6 to 59 months was 6.1% (n=114) compared to 3.0% (n=148) among non-SAM children (Figure 2). SAM children in this age group were at twice (OR 2.09, P<0.001) the risk of inpatient mortality compared to non-SAM children.
Figure 2: Inpatient mortality of severely malnourished and non-severely malnourished infants and children
Discussion
Results reveal that a large proportion of children admitted for inpatient paediatric care had SAM and that these children had elevated risk of mortality compared to non-SAM children, particularly in the U6m age group. This highlights the critical importance of identifying and appropriately managing children with SAM in paediatric inpatient settings in India, particularly in states with high burdens of wasting/severe wasting. The present study shows that medically complicated SAM cases can be effectively managed in this context with some additional training for existing staff and the addition of a nutritionist in each ward. This protocol has potential for providing greater coverage of inpatient complicated SAM treatment in response to the limited capacity of NRCs and reducing mortality risk in this vulnerable group. Observations revealed several challenges during implementation that needed to be overcome, as follows:
Identification: Kalawati Saran Children’s Hospital (KSCH) is a tertiary-care hospital with large numbers of patients that is always overcrowded. As a result, it is not routinely possible to record length/height and MUAC for every admitted child. Therefore, SAM treatment is usually initiated on the basis of weight-for-age z score (WAZ) criteria alone. Appointment of a dedicated trained nutritionist in the paediatric wards supported the facility to comprehensively take all anthropometric measurements and admit SAM children according to national protocols.
Therapeutic feeding and breastfeeding support: The addition of ward nutritionists enabled SAM feeding protocols to be fulfilled. Ward nutritionists calculated the amount of starter feed (prepared with cow’s milk, sugar, rice powder and vegetable oil to provide approximately 75 kcal and 0.9g protein per 100 ml) and catch-up diet (to provide approximately 100 kcal and 2.9g protein per 100 ml) to be offered to admitted SAM children, based on their daily weight measured between 10am and 11am. Starter and catch-up diets were prepared in the NRC unit and the correct amounts for 24 hours for each child were distributed to wards in jars and kept in refrigerators. In the daytime each feed was provided by the nutritionist posted to that ward. Having a staff member dedicated to administering feeds through the night was not feasible; therefore, night feeds were provided by caregivers (based on the guidance given by the nutritionist) with follow-up each morning by the nutritionist.
While this protocol was largely successful, reports demonstrated that caregivers commonly missed one to two night feeds per night, indicating a weak point in management. Night feeding has been found to be poorly adhered to in general in NRCs in India, indicating this to be a problem across different settings (GoI, 2011; Aguayo et al, 2014; Singh et al, 2014). Other challenges were the use of site-prepared starter and catch-up diets; experiences in other hospitals (Box 1) suggest that there may be utility in using WHO recommended F-75 and F-100 therapeutic milk products to aid quicker recovery. This needs further investigation. For infants under six months of age, breastfeeding support was provided by nutritionists in each ward and the hospital infant and young child feeding (IYCF) support centre. However, support using the supplementary suckling technique could not be provided in this context.
Management of shock and anaemia in sick SAM children: Deviations from national guidelines were observed in the management of shock, dehydration and anaemia. Most of the resident doctors are trained in and follow Paediatric Advanced Life Support guidelines, which recommend larger bolus for children with shock. Resident doctors were reoriented regarding fluid therapy for SAM children and observations suggest that most complied. However, even though the WHO and Government of India (GoI) guidelines recommend blood transfusion only for SAM children with haemoglobin less than 6g/dL in the presence of cardiorespiratory distress, doctors on duty deviated and gave transfusions to children with haemoglobin less than 8g/dL, in line with critical care guidelines but contrary to SAM management guidelines.
Counseling sessions/play therapy: We initially faced difficulty organising counselling sessions for mothers and caregivers because there was no dedicated cubicle for management of SAM children in the hospital. Cases were dispersed across the paediatric wards and it was difficult to bring their caregivers together for counselling sessions. We tried to overcome this problem by keeping all haemodynamically stable SAM children in one cubicle to enable group sessions. This was also logistically helpful for the daily weight monitoring of children with SAM to monitor their progress.
Discharges before meeting discharge criterial: Several patients were discharged on resolution of medical complications but before reaching criteria for nutritional recovery.
Follow-up of discharged children: Follow-up was extremely challenging to coordinate. Since these children were discharged from paediatric units, they were called for follow-up in outpatient department units, where it was difficult to trace them due to overcrowding. To address this, in future SAM cases will be discharged to the Paediatric Gastroenterology, Hepatology and Nutrition clinic for the first and fourth follow-ups. Second and third follow-ups will be carried out in the community by accredited social health activists (ASHAs) or Anganwadi workers at Anganwadi centres, where they will also receive take-home rations. Caregivers will be counselled to this effect.
Box 1: Integration experiences from BJ Wadia Hospital, Mumbai
BJ Wadia Hospital for Children in Mumbai is the largest paediatric tertiary-care hospital in western India. An integrated nutrition rehabilitation centre and paediatric ward system for the management of severe acute malnutrition (SAM) was implemented in 2019. During 2019, 211 patients with SAM were treated in this new system following WHO SAM management protocols using WHO-recommended F-75 and F-100 formulations.
Since the programme began, 182 (86.3%) of SAM children have been discharged as cured, with average weight gain of 5.7g/kg/day and mortality rate of 2%. A total of 76% of children were fully cured at 12 weeks of follow-up (defined as reaching weight-for-length z score (WHZ â¥2SD) at Anganwadi centres. Average length of stay in the hospital was 10.7 days. Of the admitted SAM cases, 54 (25.6%) were infants under six months old (U6m), who were managed with F75 and intensive breastfeeding counselling and support. Reported advantages of using F-75 and F-100 were easier preparation and storage, correct micronutrient mix, and acceptability in the majority of patients. Paediatric staff considered use of commercially prepared F-75 and F-100 to have contributed to the high performance indicators of this programme. In addition, nutritional care was started immediately on admission, night feeds were always given and no anthropometric measurements were missed.
Next steps
The present experience shows that integrating management of SAM within hospital paediatric wards can provide a wider and more sustainable model of care for medically complicated SAM children and increase treatment coverage. To be effective, this model requires the equipping of paediatric wards with additional infrastructure and ward nutritionists. This approach will also be greatly facilitated by clear protocols of SAM management of infants U6m and the release of the forthcoming updated Government of India (GoI) operational guidelines for the facility-based management of severe acute malnutrition (which will include clearer guidance on follow-up procedures). Other necessary inputs will be training of all paediatric medical staff in the management of SAM and routine screening for SAM in paediatric wards. There is anecdotal evidence that the use of commercial F-75/F-100 may help in the successful management of SAM cases in this context, as quality assurance of locally prepared therapeutic feeds in paediatric wards is challenging.
The authors of this paper submitted a report of the findings described to the GoI Ministry of Health and Family Welfare (MoHFW). The MoHFW has accepted the integration of complicated SAM management into paediatric wards as an effective and sustainable approach. In the upcoming revised operational guidelines, all paediatric health facilities will therefore be advised to designate four to five beds in their paediatric ward as beds for the management of SAM children with medical complications. SAM children with acute medical conditions who may need intensive care should be managed in the Paediatric Intensive Care Units (PICUs)/Paediatric ward, where providing such intensive care is possible. These children will receive therapeutic feeds and other components of SAM management in PICU/Paediatric wards. Once these children are stabilised, they can be moved to NRC beds.
Findings also highlight the key role of paediatricians in the management of SAM with complications, which has been absent in many NRCs. The upcoming SAM operational guidelines will therefore advise that new NRCs should only be established in those facilities where paediatric care is available. States should also bring existing NRCs under the supervision of paediatricians from the health facility (district/sub-district hospital) for appropriate medical management of SAM children with complications. An existing paediatrician deployed in the health facility should be designated as the NRC incharge, responsible for medical management in the NRC.
The MoHFW will also recommend the establishment of one state centre of excellence (SCoE) for SAM management where there are more than 25 NRCs. The SCoE will be located at a government medical college with a pediatric department with functional SAM management facilities. The SCoE on SAM management will provide technical advice on all matters related to programme implementation and monitoring and evaluation, and will provide training content for different levels of health worker for the NRCs.
Conclusion
This study is one of the few to examine the utility of the management of children with SAM in paediatric wards in India according to national guidelines for the management of complicated SAM. There are certain challenges in managing these children in paediatric wards that need to be overcome. However, despite these challenges, the study suggests that the routine screening for and appropriate management of SAM cases with medical complications on paediatric wards, with support for the nutritional management of these cases from on-site NRCs, is an effective model for ensuring the appropriate inpatient management of children with SAM with medical complications at scale.
References
Aguayo, V. M., Jacob, S., Badgaiyan, N., Chandra, P., Kumar, A., & Singh, K. (2014). Providing care for children with severe acute malnutrition in India: new evidence from Jharkhand. Public health nutrition, 17(1), 206-211.
Aguayo, V. M., Agarwal, V., Agnani, M., Das Agrawal, D., Bhambhal, S., Rawat, A. K., ...& Singh, K. (2013). Integrated program achieves good survival but moderate recovery rates among children with severe acute malnutrition in India. The American journal of clinical nutrition, 98(5), 1335-1342.
International Institute for Population Sciences (IIPS) and ICF. 2007. National Family Health Survey (NFHS 3), 2005-06: India. Mumbai: IIPS.
International Institute for Population Sciences (IIPS) and ICF. 2017. National Family Health Survey (NFHS 4), 2015-16: India. Mumbai: IIPS.
Isanaka, S., Boundy, E. O. N., Grais, R. F., Myatt, M., &Briend, A. (2016). Improving estimates of numbers of children with severe acute malnutrition using cohort and survey data. American journal of epidemiology, 184(12), 861-869.
Ministry of Health and Family Welfare (MoHFW), Government of India, UNICEF and Population Council, 2019. Comprehensive National Nutrition Survey (CNNS) National Report. New Delhi.
Puett C, Sadler K, Alderman H, Coates J, Fiedler J L & Myatt M (2012). Cost-effectiveness of the community-based management of severe acute malnutrition by community health workers in southern Bangladesh. Health Policy and Planning, doi:10.1093/heapol/czs070
Singh, K., Badgaiyan, N., Ranjan, A., Dixit, H. O., Kaushik, A., Kushwaha, K. P., & Aguayo, V. M. (2014). Management of children with severe acute malnutrition: experience of Nutrition Rehabilitation Centers in Uttar Pradesh, India. Indian pediatrics, 51(1), 21-25.
Swaminathan, S., Hemalatha, R., Pandey, A., Kassebaum, N. J., Laxmaiah, A., Longvah, T., ...& Gupta, S. S. (2019). The burden of child and maternal malnutrition and trends in its indicators in the states of India: The Global Burden of Disease Study 1990-2017. The Lancet Child & Adolescent Health, 3(12), 855-870.
Tandon, M., Quereishi, J., Prasanna, R., Tamboli, A. F., & Panda, B. (2019). Performance of Nutrition Rehabilitation Centers: A Case Study from Chhattisgarh, India. International journal of preventive medicine, 10, 66. https://doi.org/10.4103/ijpvm.IJPVM_194_17
Tekeste A, Wondafrash M, Azene G &Deribe K (2012). Cost effectiveness of Community-Based and In-Patient Therapeutic Feeding Programs to Treat Severe Acute Malnutrition in Ethiopia. Cost Effectiveness and Resource Allocation, doi:10.1186/1478-7547-10-4
WHO, 2007.Community-based management of severe acute malnutrition: A Joint Statement by the World Health Organization, World Food Programme, United Nations System Standing Committee on Nutrition and United Nations Children’s Fund.www.who.int/nutrition/publications/severemalnutrition/9789280641479/en/
WHO, 2009. Management of severe malnutrition: A manual for physicians and other senior health workers. Geneva, World Health Organization; 1999 www.who.int/nutrition/publications/severemalnutrition/9241545119/en/
WHO, 2013. Guideline: Updates on the management of severe acute malnutrition in infants and children. Geneva: World Health Organization; 2013.
1 See field article in this edition entitled “Community management of acute malnutrition in Rajasthan, India”
2 Weight-for-length/height z-score (WHZ) <-3 and/or mid-upper arm circumference (MUAC)<115 mm and/or bilateral pitting oedema with medical complications.
3 When using Comprehensive National Nutrition Survey (CNNS) data (MoHFW, 2017) (a likely underestimation) the estimated caseload of medically complicated wasted children is 0.6 million; when corrected for incidence (using an incidence correction factor of 1.6 as suggested by Isanakaet al, 2016), this changes to between 0.9 and 1.4 million annually.


