Managing at risk mothers and infants under six months in India – no time to waste
By Praveen Kumar, Sila Deb, Arjan de Wagt, Piyush Gupta, Nita Bhandari, Neha Sareen and Satinder Aneja
Praveen Kumar is a paediatrician working as Director Professor at the Department of Paediatrics, Kalawati Saran Children’s Hospital (KSCH), Lady Hardinge Medical College, New Delhi. He is also the Lead Coordinator of the National Centre of Excellence (NCoE) for severe acute malnutrition (SAM) management.
Sila Deb is an Additional Commissioner of the Child Health Division (Nutrition in charge), Ministry of Health and Family Welfare (MoHFW), Government of India, overseeing the National Child Health Programme for Child Health and Nutrition.
Arjan de Wagt is Chief of Nutrition Section, UNICEF India country office, New Delhi. He has over 25 years’ experience in several countries, including Nigeria, Zambia, New York and the Netherlands.
Piyush Gupta is a renowned professor, researcher, author and editor with 30 years’ experience in child health and care, medical education, research and publishing. He is the President-Elect of the Indian Academy of Pediatrics (IAP) and Chairperson of the Nutrition Chapter of IAP (PAN).
Nita Bhandari is Senior Scientist and Director of the Centre for Health Research and Development, Society for Applied Studies, New Delhi. She is a public health researcher with over three decades of research experience.
Neha Sareen is a Senior Consultant in NCoE on SAM and supports the MoHFW, Nutrition Division in management of children with severe acute malnutrition. She has nine years’ experience in maternal and child health nutrition in India.
Satinder Aneja is a paediatrician and Professor and Head Department of Paediatrics, School of Medical Sciences and Research, Sharda University, Greater Noida, India. She was formerly Director Professor and Head Department of Paediatrics at KSCH, Lady Hardinge Medical College, New Delhi.
The authors would like to acknowledge Dr Vishal Kumar, Shivani Rohatgi, Purnima Arora, Deepika Choudhary and Prachi Singh, who supported the work highlighted in this article at various stages, as well as the Child Health Division, MoHFW, Government of India, New Delhi.
Location: India
What we know: Current protocols in India do not allow for the adequate identification and management of nutritional risk in infants under six months of age.
What this article adds: Drawing from international learning, a group of experts in India developed new protocols for the management of at risk mothers and infants under six months of age (MAMI) for the identification of infants at moderate nutrition risk (for community management) and severe nutrition risk (for facility management). A training package for health workers on inpatient MAMI was developed and piloted at 10 nutrition rehabilitation centres (NRCs). Protocols were subsequently rolled out at the same NRCs between February and May 2019. A total of 258 infants was identified (69% severe and 31% moderate; moderate cases were included in lieu of community-based management not being available in India). Most breastfeeding mothers required breastfeeding support; skilled breastfeeding counselling resolved feeding difficulties in half of cases, while the remaining mothers received support using the supplementary suckling technique (SST). Success of SST depended on adequate and skilled manpower, including during the evening and night. Key challenges for roll-out of MAMI protocols in India will be ensuring an adequate and trained health workforce at both facility and community levels and provision of psychosocial support for mothers.
Background
Malnutrition in infants under six months in India - a significant public health problem
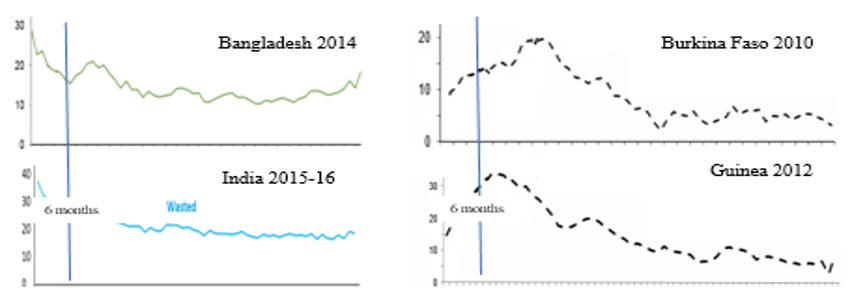
Adequate nutrition during the first six months of life is crucial for appropriate growth and the formation and development of the nervous system (Cusick and Georgieff, 2016; Fox et al, 2010). There are approximately 4.7 million infants under six months old (U6m) worldwide who are moderately wasted (weight-for-length ⥠â3 to -2 z) and 3.8 million who are severely wasted (weight-for-length -3 z) (Kerac et al, 2011), making malnutrition in this age group a significant global public health problem. The issue of U6m malnutrition is particularly serious in India, where the prevalence of wasting in this age group is 31.9% and that of severe wasting is 14.9% (IIPS, 2017). The prevalence of wasting is highest at birth (37%) and declines with age (IIPS, 2017) - a similar pattern to that seen in other South Asian countries, such as Bangladesh, but different to the pattern seen in west and central Africa, where prevalence of wasting is relatively low at birth and increases in infancy, peaking at around 12 months of age (WHO and UNICEF, 2004; de Wagt et al, 2019) (Figure 1).
Figure 1: Wasting prevalence (%) by age-based Demographic Health Survey (DHS) reports
This highlights that the origins of early-life undernutrition in South Asia often begin in utero with intrauterine growth restriction (IGR), resulting in many infants being born with low birth weight (LBW) each year. Of the 20.5 million LBW infants born annually in low- and middle-income countries, around 9.8 million are estimated to live in South Asia (UNICEF and WHO, 2019); it is estimated that 75% of infants born with LBW in South Asia live in India alone (Lee et al, 2013). A child born with LBW has higher risk of death in infancy and those who survive have higher risk of morbidity and acute malnutrition during infancy and early childhood. Individuals born with IGR are also at greater risk of non-communicable diseases such as hypertension, diabetes and dyslipidaemia in adulthood after a period of rapid weight gain (Hales et al, 1991). This highlights the imperative to address growth failure during pregnancy and in the early stages of life in South Asian countries. This is a central focus of the recently launched POSHAN Abhiyaan programme in India, which aims to improve antenatal care and breastfeeding practices nationwide, with a central target of decreasing LBW by 2% per annum.
Current state of care for vulnerable infants in India
To manage those infants born at risk, the Government of India (GOI) under the National Health Mission (NHM) has established special newborn care units (SNCUs). SNCUs provide specialised care to infants who are born preterm (<34 weeks) or birth weight of <1,800g1 and other sick neonates under 28 days of age. To date, 844 SNCUs have been established in district hospitals and medical colleges across India, treating nearly one million newborns per year (MoHFW, 2020). SNCUs undoubtedly save many lives, demonstrated by almost one million fewer newborn deaths in India in 2017 compared to 2000 (UNICEF, 2020).
At community level, the Home Based Newborn Care (HBNC) programme was launched in 2011 to accelerate the reduction of neonatal mortality rates, particularly in rural, remote areas where care is otherwise inaccessible. Accredited social health activists (ASHAs) undertake seven follow-up visits of all infants during the first 42 days of life, including LBW infants and infants discharged from SNCUs (day one is taken as the discharge date from SNCU), with ongoing follow-up for 18 months for all LBW infants (including infants born <1,800g admitted to SNCUs and infants born 1,800-2,500g in the HBNC programme) and 12 months for non-LBW preterm infants. During seven follow-up visits, ASHAs provide support to the mother to sustain exclusive breastfeeding for six months, ensure continued kangaroo mother care, perform regular growth monitoring, and identify signs of sickness in mothers and infants for early referral (MoHFW, 2014). After 42 days ASHAs provide an additional five follow-up visits to infants between 3 and 15 months of age under the Home Based Care for the Young Child (HBYC) programme. These visits are designed to improve nutritional status of young children, ensure proper growth, early childhood development, and prevent childhood illness (such as diarrhoea and pneumonia) and deaths resulting from them (MoHFW, 2018). In addition, some nutrition rehabilitation centres (NRCs) manage acutely malnourished infants U6m according to national severe acute malnutrition (SAM) protocols (those with weight-for-length z-score of <3SD or bilateral pitting oedema).
An important weakness of this current system is the lack of clarity on how to identify infants at nutrition risk (not just those already severely acutely malnourished) and appropriate actions for their management. Growth failure in infancy, resulting in infant malnutrition, is a complex, multifactor problem associated with many risk factors that encompass maternal, infant and social characteristics. A failure to identify and avert risks early is a key weakness of the existing system that inhibits the provision of nutrition care for this key vulnerable group.
MAMI approach in India – the opportunities
The Management of At Risk Mothers and Infants U6m (MAMI) Special Interest Group2 developed the Community-MAMI (C-MAMI) tool3 as a first step to help support the identification and management of uncomplicated, nutritionally at-risk mother-infant dyads in the community consistent with recommendations of the 2013 updated World Health Organization (WHO) guidelines (WHO, 2013). The encouraging results of pilots in Ethiopia and Bangladesh (Butler et al, 2018) sparked interest among Indian experts striving to improve the care of at-risk mothers and infants in India. As a result, two expert group consultation meetings were held to discuss evidence related to early growth failure identification and MAMI at facility and community levels in India.
The first consultation was held in October 2018 to discuss current understanding of growth patterns and deviations in early infancy. The co-lead of the MAMI Special Interest Group4 attended the consultation to share global MAMI learning and experience of using the C-MAMI tool. As follow-up, a group of experts developed a training package to strengthen inpatient care of infants under six months old (U6m) with severe malnutrition. With the approval of the Government of India (GoI) Ministry of Health and Family Welfare (MoHFW), the training package was subsequently piloted in 10 selected nutrition rehabilitation centres (NRCs). Experiences of the pilot study are shared below.
A second consultation was organised in October 2019 to further discuss and finalise algorithms and guidelines for the identification and management of infants U6m at nutrition risk in the community. Presentations by government representatives and eminent national scientists and ensuing discussions among experts from different states, the United Nations Children’s Fund (UNICEF), Save the Children, and the Breastfeeding Promotion Network of India (BPNI) provided the basic framework for finalising operational and technical guidelines on Early growth failure: identification and management through existing Government platforms. Following further revisions by participants, a final draft of the guidelines was presented to MoHFW with the recommendations outlined in Box 1. The recommendations leverage existing government health platforms for MAMI (including the Home Based Care for the Young Child (HBNC) programme, the Home Based Care for the Young Child (HBYC) programme, and Village Health Sanitation and Nutrition Days (VHSNDs) (MoHFW, 2019)), utilising existing health workers, including accredited social health activists (ASHAs), anganwadi workers (AWWs) and auxiliary nurse midwives (ANMs). The new guidelines have been agreed in principle, but no official order for their implementation has been issued as yet.
Box 1: Recommendations for identification and management of early growth failure in infants in India
1. Infants under 6 months of age (U6m) will be classified into three categories according to their nutritional risk: not at risk, moderate risk of malnutrition, and severe risk of malnutrition.
2. For identifying ‘at-nutrition risk’ infants, assessment in the following four broad areas will be used:
a) assessment for sickness as per Integrated Management of Neonatal and Childhood Illnesses (IMNCI) guidelines;
b) assessment for breastfeeding and feeding practices;
c) determination of weight-for-age (WFA) as per WHO 2006 growth standards; and
d) assessment of maternal nutrition, health and psychosocial status.3. If an infant has not regained birth weight by day 14, and/or has gained weight less than 20g/day (<150g/week) after the second week of life, they should be carefully assessed for any sign of sickness; feeding problems, including breast attachment and positioning; and maternal nutrition, health and psychosocial problems.
4. During each home/health facility contact, the infant’s nutritional risk should be classified as one of: not at risk, moderate risk of malnutrition, or severe risk of malnutrition (Table 1).
5. Existing government platforms should be effectively utilised to identify and manage at-nutrition risk infants.
6. Infants U6m at moderate risk of malnutrition should be managed in the community by trained mother’s absolute affection (MAA) frontline workers. All frontline workers, Anganwadi Workers (AWWs) who are not trained or who have sub-optimal skill should be trained/reoriented to take correct anthropometric measurements of infants and assess for signs of sickness. They should be empowered to identify infants at nutrition risk and help mothers with breastfeeding problems by improving attachment and positioning. If there is poor weight gain, even after two weekly contacts, or if there is further weight loss during the follow-up visit after one week, the infant should be referred to a health facility for evaluation.
7. Infants U6m at severe risk of malnutrition should be referred and managed at health facilities with nutrition rehabilitation centres (NRCs) or a paediatric facility with staff trained to help mothers with breastfeeding problems.
8. The nutrition division should strengthen services for mothers at severe nutrition risk at state and districts level, including the provision of support to mothers with adverse psychosocial status (currently limited to bigger hospitals).
9. Attempts should be made to improve convergence between programmes at ground level, including the Integrated Child Development Services (ICDS) programme, the Home Based Newborn Care (HBNC) programme, the Home Based Care for the Young Child (HBYC) programme, and Village Health Sanitation and Nutrition Days (VHSNDs), and to harmonise existing guidelines.
10. In the rare circumstances where there are no prospects of breastfeeding (such as in cases where the mother has died or is seriously ill and unable to breastfeed, the infant has been adopted, or the mother is unable to breastfeed successfully even after counselling and support), health workers should help families choose the best suitable replacement feeding option after discussing each option’s advantages and disadvantages. Options include: donor human milk, infant formula and fresh, undiluted animal milk. If the mother is unwell, exclusive breastfeeding should be re-established once her condition becomes stable. Mothers and caregivers of babies receiving infant formula or animal milk should be empowered to feed their infants with good hygiene, without over-dilution and with a katori/paladai*. Bottle-feeding should be proactively discouraged as a potential source of infections among infants.
* Katori is a stainless-steel bowl commonly used in India to feed children. Paladai is a low bowl with a spout (feeding device) traditionally used in India.
Table 1: Classification of infant nutritional risk
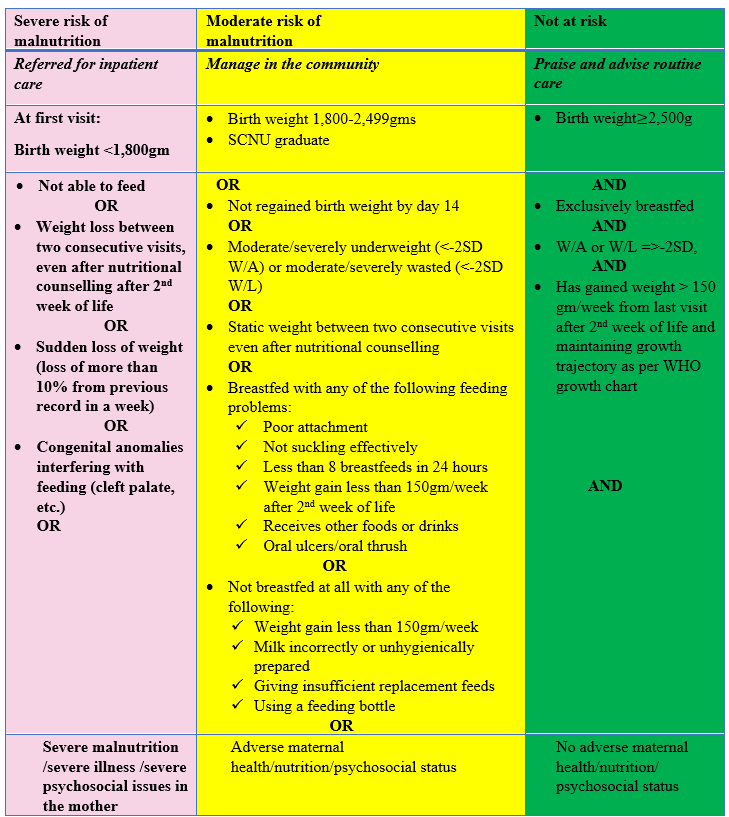
Key: W/A = weight-for-age; W/L = weight-for-length
Pilot Management of At Risk Mothers and Infants under six months of age (MAMI) programme
MAMI training programme
A four-day pilot training using the new inpatient care training package on management of infants under six months old (U6m) with severe malnutrition was held in November 2018 by the National Centre of Excellence on Severe Acute Malnutrition (NCoE SAM), with support from the United Nations Children’s Fund (UNICEF), at Kalawati Saran Children’s Hospital (KSCH), New Delhi, with the approval of the Ministry of Health and Family Welfare (MoHFW). A total of 27 participants from nutrition rehabilitation centres (NRCs) in 10 states5 attended, including paediatricians, medical officers, nutritionists and staff nurses. The training covered the following topics (similar to proposed guidelines): identification of infants U6m; care and management of infants U6m with prospect of being breastfed; management of infants who need relactation support; discharge criteria and follow-up; and conducting sensory stimulation and structured play therapy with age-appropriate toys. Training methods included classroom reading, watching videos and group clinical sessions (covering the taking of anthropometric measurements; calculation of standard deviation scores; and identification and management of infants at nutrition risk).
MAMI implementation experiences
Following the pilot training, staff from the 10 selected NRCs implemented the new protocol for the screening and classification of infants as: not at nutrition risk, at moderate nutrition risk and at severe nutritional risk. Infants U6m at moderate and severe nutritional risk were admitted and managed in NRCs, in line with proposed guidelines. Experiences of admitting and managing infants U6m during the pilot period (February to May 2019) were documented and shared with NCoE SAM monthly. Of 890 children presenting across the 10 NRCs during the study period, 258 (~29%) were infants U6m; over two thirds (69%) of whom were identified as having severe nutritional risk and admitted for inpatient care. Of the severe cases, 9.6% had length <45cm.6 The remaining 31% of infants were identified as having moderate nutritional risk. These infants were also admitted for care but could have been managed in the community, had community-level services been available.
A monitoring checklist assessed adherence to inpatient treatment protocols during supportive supervision (this checklist was designed for the pilot programme, although there are plans to use it for future supervision). The majority of NRCs adhered to the protocols; however, deviation from protocols for electrolyte supplementation of potassium and magnesium was seen in some NRCs due to a lack of clarity on whether health workers should supplement infants with prospects of breastfeeding or not. Staff from four NRCs reported operational challenges, including lack of stock supply of antibiotics and micronutrient supplements, and lack of personnel to manage evening and night shifts, leading to non-adherence to protocols, particularly with regard to support for the supplementary suckling technique (SST). Temperature recording and antibiotics were administered correctly, but blood glucose testing was irregular in three NRCs.
Out of 258 infant U6m admissions, 208 (80%) had prospects of breastfeeding (the mother was available and either currently breastfeeding or had stopped breastfeeding within the last two months). Of these, 166 (79.8%) had incorrect breastfeeding attachment and positioning, which was corrected in over half of cases (55.4%, n=92) with counselling and support from NRC staff. The remaining mothers with prospects of breastfeeding were supported using SST. A total of 47 mothers (who had not breastfed for longer than two months) consented for relactation by SST. Full success was seen in 45% (21/47) of cases; partial success was observed in 25% (12/47) of cases and was not successful in 30% (14/47). NRCs with more success with SST had adequate and skilled manpower; those with less success with SST had less skilled manpower available, particularly during evening and night shifts.
Key learnings from the pilot programme
The pilot programme demonstrated that, with training support, most NRCs can successfully identify and manage infants U6m at nutrition risk. The majority of mothers with prospects of breastfeeding had incorrect breastfeeding attachment and positioning, which was rectified in over half of the mothers through breastfeeding counselling. These infants could have been successfully managed in the community using existing government platforms if health workers providing these services were trained to provide this level of breastfeeding support.
Other infants U6m required admission to the NRC either for the management of medical complications or to implement SST. For these cases, the success of treatment depended on the availability of a paediatrician and round-the-clock supervision. Non-availability of human resources for evening and night shifts led to non-adherence of protocols in the NRCs. This is a key point of weakness in the current system that must be resolved with adequate manpower and appropriate staff training. It was noted that, after a gap of more than three months from cessation of breastfeeding, the success rate for relactation decreased. This highlights the critical importance of early intervention in mothers with breastfeeding problems.
Maternal health and nutrition services in India
The wellbeing of an infant is determined to a large extent by the wellbeing of their mother. The Management of At Risk Mothers and Infants under six months of age (MAMI) approach therefore always considers the infant-mother pair and includes a maternal mental-health care component. In the India context, the nutritional management of mothers is complex, both in terms of lack of availability of food and difficulties in the implementation of maternal nutrition programmes at the grassroots level. In 2011 the Government of India (GoI) launched the Janani Shishu Suraksha Karyakaram (JSSK) programme to provide free transport, drugs, diagnostics, blood and supplementary food to pregnant women delivering in health institutions (MoHFW, 2011). Several other schemes (including Anganwadi services, schemes for adolescent girls and Pradhan Mantri Matru Vandana Yojna (PMMVY) under the umbrella of the Integrated Child Development Scheme (ICDS)) also provide interventions to address the problem of malnutrition among women and children in the country (MoWCD, 2017). Support services also exist to address the multi-sector social determinants of health that affect women’s uptake of existing health services, including economic status, caste, ethnicity, maternal education, husband education, religion and culture. GoI programmes addressing this problem include Janani Suraksha Yojana (JSY), JSSK, Village Health Sanitation and Nutrition Committees (VHSNCs), and Village Health Sanitation and Nutrition Days (VHSNDs), which provide an institutional platform to foster convergence and address social determinants of health at ground level. Linkages with such services will be necessary for future successful community and facility-based MAMI.
An important challenge in India is the lack of existing services for maternal psychosocial assessment and support; maternal mental health has only recently come to be recognised as important for the wellbeing of at-risk mothers and infants. Currently, dedicated maternal mental health services are largely deficient in health facilities and health workers lack training in mental health issues. Availability of mental health specialists is also limited in peripheral healthcare facilities. Moreover, postnatal traditions (such as the period of seclusion at home observed in many cultures and reluctance of mothers to disclose mental health problems due to social taboos and stigma) negatively affect care-seeking behaviour in the postpartum period (Upadhyay et al, 2017). In the absence of adequate social support, identifying families’ psychosocial problems may further complicate issues. Although a challenging task, there is an urgent need to develop convergence and strong linkages between psychiatry, medicine, child development and maternal and social development to manage both mothers and their infants effectively.
Management of At Risk Mothers and Infants under six months of age (MAMI) in India – the way forward
In India, with high prevalence of severe wasting in infants aged under six months (U6m), it is not possible to provide inpatient care to all such infants. Given the profile of many infants requiring intervention, inpatient care is also not the best setting for their support. The ability to test the utility and feasibility of community-based management of infants U6m at moderate risk of malnutrition in India through existing government platforms could provide a major step forward in preventing growth failure and malnutrition in this vulnerable group.
Recently, the Prime Minister of India launched the flagship programme POSHAN Abhiyaan. This programme has given new hope for the provision of a continuum of care to improve nutritional outcomes for children, adolescents, pregnant women and lactating mothers through a comprehensive package of convergent interventions across multiple government schemes and programmes. Included in this integrated package is community-based management of SAM as one of a range of nutrition-sensitive and nutrition-specific interventions. The Ministry of Health has also launched the Mother’s Absolute Affection (MAA) programme to improve breastfeeding practices, which will be utilised for the scaling up of training of in-service health personnel to empower them to provide skilled support to mothers with breastfeeding problems. This provides a real opportunity to scale up widespread support for mothers to identify growth failure at the earliest possible point and provide a targeted intervention to avert further deterioration, and ultimately to prevent severe malnutrition in this critical age group. The pilot study described here demonstrates the utility, where infants continue to deteriorate or present key indicators of nutritional risk, of providing skilled, facility-based support to improve their nutritional status before discharge back into the community. This includes use of the supplementary suckling technique (SST), the success of which requires a high level of skilled personnel both day and night. This level of support must be factored into nutrition rehabilitation centres (NRCs) and paediatric facilities across India to ensure the viability of this approach.
We acknowledge that low birth weight and early growth failure is a huge problem in infants U6m in India. We have existing systems and government platforms and a large cadre of health workers across the country to deliver community-based health and nutrition programming from pre-pregnancy until five years of age to address these issues in a comprehensive manner and at scale. Should these systems and platforms be fully utilised, inpatient care for infants U6m may only be required for those at severe nutritional risk and who do not improve with community-based interventions, which is likely to be a more cost-effective approach for both government and families.
For more information please contact Prof. Praveen Kumar.
The C-MAMI Tool referred to in this article is currently being updated into a MAMI Care Pathway by the MAMI Special Interest Group. Dr Praveen Kumar is part of a working group informing this update. For more information, visit www.ennonline.net/ourwork/research/mami
References
Butler S, Connell N and Barthorp H. C-MAMI tool evaluation: Learnings from Bangladesh and Ethiopia. Field Exchange. 2018; 58: 62. www.ennonline.net/fex/58/cmamitoolevaluation.
Cusick SE, Georgieff MK. The Role of Nutrition in Brain Development: The Golden Opportunity of the "First 1000 Days". J Pediatr. 2016; 175: 16-21.
de Wagt A, Rogers E, Kumar P, et al. Continuum of care for children with wasting in India: Opportunities for an integrated approach. Field Exchange. 2019; 60: 82-85.
Fox SE, Levitt P, Nelson CA. How the timing and quality of early experiences influence the development of brain architecture. Child Development. 2010; 81: 28-40.
Hales CN, Barker DJ, Clark PM, et al. Fetal and infant growth and impaired glucose tolerance at age 64. BMJ. 1991; 303:1019-1022.
International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-4), 2015-2016; India. Vol. I. Mumbai: IIPS; 2017.
Kerac M, Blencowe H, Grijalva-Eternod C, et al. Prevalence of wasting among under 6-month-old infants in developing countries and implications of new case definitions using WHO growth standards: a secondary data analysis. Archives of disease in childhood, 96(11), 1008-1013. https://doi.org/10.1136/adc.2010.191882
Lee AC, Katz J, Blencowe H, et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health. 2013;1(1): e26-36.
Ministry of Health and Family Welfare (MoHFW) and Ministry of Women and Child Development (MoWCD). National Guidelines for Village, Health, Sanitation and Nutrition day (VHSND). Government of India. 2019.
Ministry of Health and Family Welfare (MoHFW). Facility based newborn care operational guide: Guidelines for planning and implementation. Government of India. 2011.
Ministry of Health and Family Welfare (MoHFW). Government of India. Real time monitoring and tracking of small and sick newborn. http://sncuindiaonline.org/d_loginAction. accessed 20 April 2020.
Ministry of Health and Family Welfare (MoHFW). Guidelines on Janani Suraksha Yojna (JSY). Government of India. 2005.
Ministry of Health and Family Welfare (MoHFW). Home Based Care for Young Child (HBYC). Strengthening of health and nutrition through home visits, Operational Guidelines. Government of India. 2018.
Ministry of Health and Family Welfare (MoHFW). Home based newborn care operational guidelines. Government of India. 2014.
Ministry of Health and Family Welfare (MoHFW). National Guidelines on Janani-Shishu Suraksha Karyakram (JSSK). Government of India. 2011.
Ministry of Women and Child Development (MoWCD). National Guidelines on Pradhan Mantri Matru Vandana Yojna (PMMVY). Government of India. 2017.
United Nations Children’s Fund (UNICEF), World Health Organization (WHO). UNICEF-WHO Low birthweight estimates: Levels and trends 2000-2015. Geneva: World Health Organization; 2019 Licence: CC BY-NC-SA 3.0 IGO
Upadhyay RP, Chowdhury R, Salehi A, et al. Postpartum depression in India: a systematic review and meta-analysis. Bulletin of the World Health Organization. 2017;95:706-717C.
WHO growth standards: a secondary data analysis. Arch Dis Childhood. 2011; 96: 1008-1013.
World Health Organization and United Nations Children’s Fund. Low birthweight: country, regional and global estimates. World Health Organization, Geneva, 2004.
World Health Organization. Updates on the management of severe acute malnutrition in infants and children. Guideline. 2013.
1 LBW infants born 1,800-2,500g are managed in the Home Based Newborn Care (HBNC) programme.
2 An international collective of programmers, policy-makers and researchers, coordinated by Emergency Nutrition Network (ENN) www.ennonline.net/ourwork/research/mami
3 C-MAMI tool (version 2) 2018 www.ennonline.net/c-mami
4 Marko Kerac from the London School of Hygiene and Tropical Medicine (LSHTM).
5 Bihar, Delhi (Kalawati Saran Children’s Hospital), Haryana, Jharkhand, Karnataka, Madhya Pradesh, Maharashtra, Odisha, Rajasthan and Uttar Pradesh.
6 Length <45cm was not included as a specific risk criterion as most infants of this length will be identified by the weight-for-age criteria.
About This Article
Jump to section
- Background
- MAMI approach in India – the opportunities
- Pilot Management of At Risk Mothers and Infants under six months of age (MAMI) programme
- Maternal health and nutrition services in India
- Management of At Risk Mothers and Infants under six months of age (MAMI) in India – the way forward
- References


