Wasting prevention and treatment - central to stunting reduction in Pakistan
Click here to listen to more information on the work being done in Pakistan on the ENN podcast channel
By Saba Shuja, Eric Alain Ategbo, Yasir Ihtesham and Khawaja Masood Ahmed
Saba Shuja is a Nutrition Officer for UNICEF Pakistan and a public health professional with over 15 years’ experience of working in health and nutrition both in emergency and developmental contexts with the United Nations (UN) and other humanitarian organisations.
Eric Alain Ategbo is Chief of Nutrition for UNICEF Pakistan and a nutritionist with over 30 years of experience working in Ethiopia, the Democratic Republic of Congo, Niger, Uganda and India. Eric was previously a faculty member of the Department of Nutrition and Food Science, Faculty of Agricultural Sciences, University of Benin.
Yasir Ihtesham is Acting Head of Nutrition for World Food Programme (WFP) Pakistan and a public health practitioner with over 12 years of experience working in nutrition in emergency and development contexts with UN agencies.
Khawaja Masood Ahmed is the National Coordinator of the Nutrition and National Fortification Alliance of the Ministry of National Health Services, Regulations and Coordination, Government of Pakistan. Khawaja has over 30 years of experience working in health and nutrition.
Location: Pakistan
What we know: Both wasting and stunting remain highly prevalent in Pakistan despite national targets to meet the Sustainable Development Goals. There is growing evidence and recognition that wasting and stunting are interlinked.
What this article adds: Stunting reduction has been prioritised in Pakistan. Coverage of wasting treatment services in Pakistan is low (below 5%) which likely contributes to resistant stunting levels. Efforts are underway to integrate wasting treatment within primary healthcare services to catalyse scale-up. The Multi-Sectoral Nutrition Strategy 2018-2025 guides sector-specific action at federal and provincial levels (health, social protection, water, sanitation and hygiene (WASH), education, agriculture and livelihoods). Provincial interventions to address stunting and wasting are often siloed with variable coverage but have good potential to more closely align. There is strong political commitment and growing action to integrate wasting prevention and treatment with stunting reduction strategies in Pakistan. At federal level, a new five-year initiative to 2025 has been launched to tackle stunting with an integrated wasting management component targeting 35% of Pakistan’s poorest population. To accelerate progress, a comprehensive national and provincial level nutrition review is being planned to inform a national nutrition policy and programming approach to guide a more holistic, harmonised response across the life cycle and all forms of malnutrition.
Context
The high prevalence of all forms of malnutrition among vulnerable groups is a major concern in Pakistan. Undernutrition (both stunting and wasting), overweight/obesity and micronutrient deficiencies, either in isolation or in combination, have a marked effect on young children and women of reproductive age across the country. Globally, Pakistan is home to the highest number of stunted children after India and Nigeria. Over 40% of Pakistan’s children under five years of age are stunted (12 million children) and 17.7% are wasted with 2.5 million children under five years of age estimated to be severely wasted (Government of Pakistan (GoP), 2018). Pakistan is one of the first countries in the world to nationally adopt the global Sustainable Development Goals (SDGs) to achieve a 40% reduction in stunting in children under five years of age and to reduce and maintain childhood wasting below 5%. However, progress is slow and Pakistan is far from achieving these targets - since 2001 there has been a marginal decline in the prevalence of stunting (an average annual reduction rate of around 0.4%) and an increase in the prevalence of wasting (17.7% in 2018) compared to 1990 levels (12.5%) (GoP, 2018).
The links between wasting and stunting
Evidence of wasting as a direct cause of stunting and the relationship between both manifestations of undernutrition is currently being explored globally (Wasting-Stunting Technical Interest Group (WaSt TIG), 2018). Growing evidence suggests that wasting is a direct cause of stunting, with studies showing that periods of wasting during childhood increase the risk of later stunting (Richard et al, 2012; Schoenbuchner et al, 2018). There is also evidence that growth in height slows down in wasted children until their weight gain recovers (Briend et al, 2014). The risk of death for children concurrently wasted and stunted is high comparable to that of severely wasted children (WaSt TIG, 2018), making this a problem of particular concern.
An estimated 5.9% of children under five years of age in Pakistan are concurrently wasted and stunted (Government of Pakistan (GoP), 2018) with the prevalence of concurrent wasting and stunting highest in rural areas (6.8%), among children of mothers without any education (7.7%) and households within the poorest wealth quintiles (10.7%). Concurrent wasting and stunting is also slightly more prevalent among boys (6.5%) compared to girls (5.4%). In terms of geographical spread, the highest prevalence of concurrent stunting and wasting is in Sindh province (10.0%) followed by Balochistan (6.5%), Punjab (4.3%) and Khyber Pakhtunkhwa (3.7%).
Different analyses reveal several common predictors of wasting and stunting in Pakistan, including poor maternal nutrition (underweight or low stature) and poor water or sanitation (Kim et al., 2017; Harding, Aguayo and Webb, 2018). The age distribution of wasting and stunting differs but there are common drivers and both conditions may already be present at birth and persist concurrently in the first year of life. The high prevalence of concurrent stunting and wasting among the districts with high rates of maternal underweight (body mass index (BMI) <18.5 kg/m2) suggests that maternal factors play a major role in early infant growth failure and that integrated strategies for prevention and management should target pregnancy and early infancy (GoP, 2018).
Pakistan has very high levels of undernutrition among women of reproductive age. According to the National Nutrition Survey 2018, 42.7% of women are anaemic and uptake of iron and folic acid (IFA) supplementation is low (GoP, 2018).1 Furthermore, 14.4% of women are underweight and overweight and obesity have increased from 28% in 2011 to 38% in 2018. In Pakistan, infant and young child feeding practices are also suboptimal. Less than half of mothers (45%) practice early initiation of breastfeeding and only around half (48%) of infants aged less than six months are exclusively breastfed. Only one in every three infants age 6-8 months is fed complementary food and only 3.6% of children 6-23 months receive complementary foods that meet the requirements of a minimum acceptable diet (GoP, 2018).
These data point to a continuum of undernutrition throughout the lifecycle in Pakistan with a close association between undernutrition in women and their offspring. This is reflected in the high prevalence of low birth weight (LBW) in the country at 20%, whereby in-utero origins of undernutrition result in many infants being born wasted and stunted which is then exacerbated by poor infant and feeding practices after birth. Notably in Pakistan, more than half of all childhood stunting and wasting is apparent by six months of age and the bulk established by 24-36 months of age (GoP, 2018).
Low coverage of wasting treatment in Pakistan as a driver of stunting
Despite provincial community-based management of acute malnutrition (CMAM) programmes to manage severe wasting in Pakistan, the coverage of treatment services remains below 5%. This is largely due to CMAM programming being, until recently, emergency-driven with short term and unpredictable funding and a lack of integration of wasting treatment services into the routine health system, particularly in development settings. Efforts are now underway to address this by implementing wasting treatment services through an existing cadre of government health workers (Lady Health Workers (LHWs)). This is explored fully in another article in this issue of Field Exchange.2
Another contributing factor to the low investment in wasting management in Pakistan has been the global drive to scale up multi-sectoral nutrition programming to reduce levels of stunting through the Scaling up Nutrition (SUN) movement. While this has helped put stunting reduction high on the national political agenda in Pakistan, it has also somewhat ‘divided’ interests, contributing to a separation in national policy-making and programming for stunting and wasting and with stunting (nutrition-sensitive programing) and wasting (nutrition-specific programming) falling under separate government entities.3 This separation has been exacerbated by the historical impression that wasting is a short-term problem that is quickly reversible with the right treatment when, in reality, many children in Pakistan face repeated or persistent episodes of wasting in their early years which contribute to an increased risk of stunting and death. Given the close link between wasting and stunting in Pakistan, this failure to provide treatment to the majority of wasted children most likely contributes to the high prevalence of stunting in the country.
It is increasingly understood that wasting treatment and prevention are essential components of efforts to promote the healthy growth and development of children in Pakistan. Both wasting and stunting should therefore be viewed through a single lens and wasting treatment and prevention included as a component of stunting prevention in all contexts where wasting exists - both humanitarian and development - to achieve stunting and mortality reduction.
Strategies and programmes to address stunting in Pakistan
Pakistan has developed strategies for stunting reduction (as well as wasting management, maternal and adolescent nutrition) at both the federal and provincial levels under the overarching strategic framework of the Pakistan Multi-Sectoral Nutrition Strategy (PMNS) 2018-2025. This strategy was designed to double the current average annual reduction rate (AARR) in stunting from 0.5% to 1% and therefore reduce the prevalence of stunting from 40% in 2018 to 33% by 2025. All provinces in Pakistan have developed, and are implementing to some extent, a multi-sectoral response in line with this strategy. The sectors involved usually include health, agriculture, fisheries and livestock, education, population welfare, water, sanitation and hygiene (WASH) and social protection. Specific actions by sector and plans within the provinces are described below.
Health sector: Selected nutrition interventions, including iron and folic acid (IFA) supplementation for pregnant women, child deworming, vitamin A supplementation, treatment of severe acute malnutrition (SAM), promotion of infant and young child feeding (IYCF) and multiple micronutrient powders (MNP) are currently delivered through the government health service delivery platform as a routine package of services for women and children. This is delivered through time-bound provincial nutrition projects (PC-1), delivered vertically through a specific cadre of staff in parallel with the primary healthcare system. Current work to integrate this system fully within the primary health care system (delivered through Lady Health Workers (LHWs)) is ongoing.4 Full integration into public healthcare is essential to ensure national coverage of wasting treatment and prevention and in order to have a meaningful impact on levels of stunting.
Social protection: The Benazir Income Support Program (BISP) under EHSAAS is the biggest federal nutrition-sensitive social protection scheme in Pakistan, launched in 2008, targeting 5.7 million of the poorest and most vulnerable of Pakistan’s population. The BISP is a nationwide conditional cash transfer programme that aims to improve the health and nutrition situation in Pakistan through the reduction of stunting. Families receiving cash grants are encouraged to improve their dietary intake through nutrition counselling (although the nutrition counselling component is so far quite weak). Early efforts are underway to link this service with the public healthcare system and service delivery platform, delivered through LHWs. Recently, a health and nutrition conditional cash transfer programme, Ehsas Nashwonuma, was launched to address stunting in children under 23 months of age in high burden districts, implemented through health facilities. This is funded by the Government of Pakistan (GoP) with implementation through the World Food Programme (WFP).
WASH sector: Federal and almost all provincial multi-sectoral stunting alleviation strategies include water, sanitation and hygiene (WASH) interventions and mainly focus on hygiene promotion, access to and use of safe water and the promotion of Open Defecation Free (ODF) villages using the Community-Led Total Sanitation (CLTS) approach. In provinces such as Sindh and Punjab, provincial WASH sector plans also include objectives such as a reduction in diarrhoea prevalence and improvement of safe hygienic feeding practices. However, the scale of implementation of these programmes is currently limited to specific geographic areas.
Agriculture and livelihoods to boost food access: Nutrition-sensitive interventions such as the promotion of kitchen gardening, fruit tree plantation, agriculture, fisheries and livestock are included in the multi-sectoral nutrition strategy and reflected in sectoral plans. The role of livelihood and food-based approaches needs strengthening and synergies identified and established to enable and sustain complementarity.
Education sector: The education sector is collaborating with the health sector to target adolescent girls and school-aged children with nutrition interventions. According to the National Guidelines on Adolescent Nutrition and Supplementation and National Adolescent Nutrition Strategy, all adolescent girls should receive weekly iron folic acid (WIFA) tablets. This strategy is included in national and some provincial nutrition programming and a pilot programme is currently being implemented in one district to assess its effectiveness, challenges and bottlenecks.
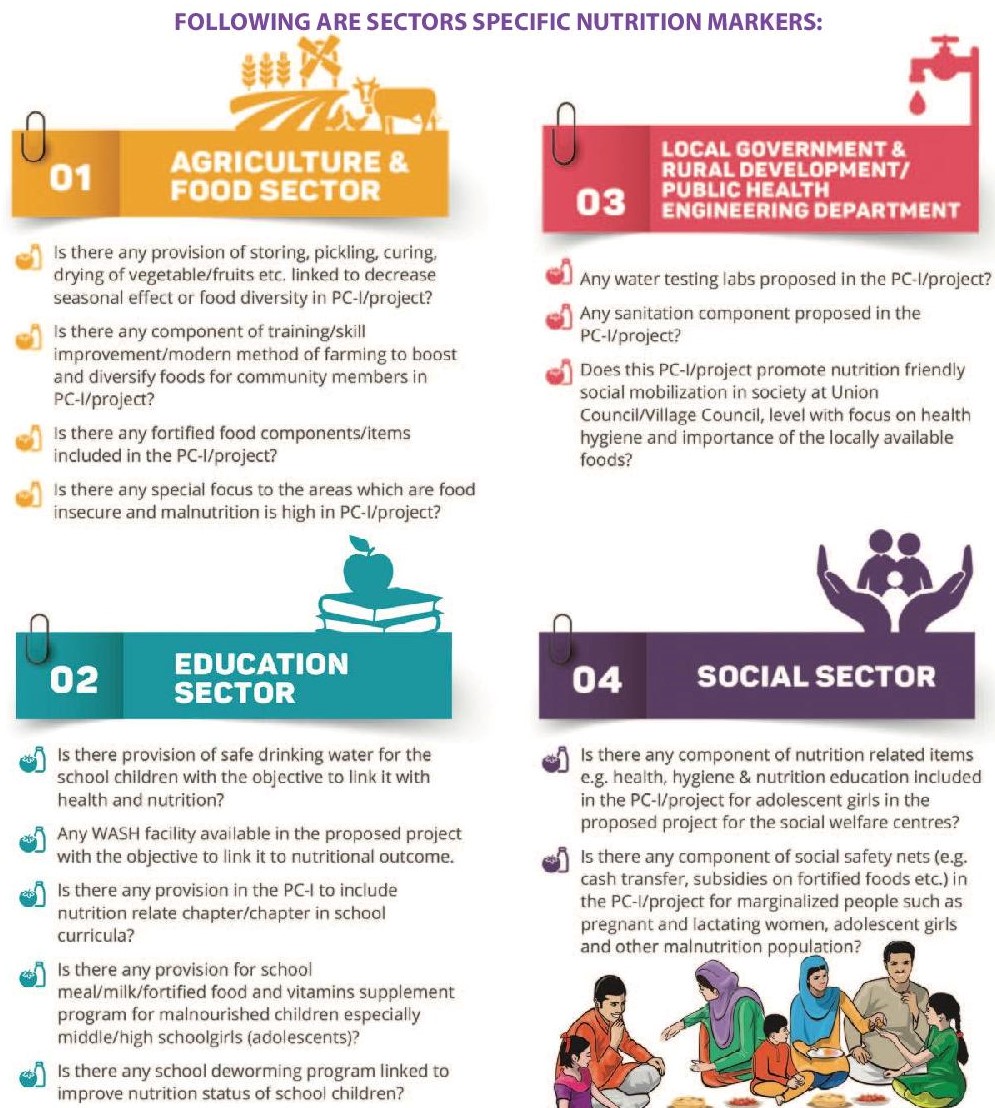
To ensure that different sectors include stunting reduction into their planning process, the Scaling up Nutrition (SUN) Secretariat of Khyber Pakhtunkhwa (KP) province has developed general nutrition markers (Figure 1) and sector-specific nutrition markers (Figure 2) for the Government of KP to use when assessing projects submitted for consideration for funding. This is so far being used in KP but there are plans to expand the use of the nutrition markers to other provinces.
Figure 1: General nutrition rules and markers - Government of Khyber Pakhatunkhwa, Pakistan

Figure 2: Sector-specific nutrition markers - Government of Khyber Pakhatunkhwa, Pakistan
Opportunities to link stunting and wasting reduction initiatives
Although provincial multi-sectoral strategies and plans exist to address the management of both wasting and stunting, the post-devolution scenario has resulted in the fragmentation of strategies across various programmes, projects and geographic areas. An integrated full package of interventions to address wasting and stunting simultaneously in all contexts does not yet exist. Owing to the clear demonstration of the concurrence of wasting and stunting in the National Nutrition Survey 2018, there is now understanding among national decision-makers and programmers that it is high time to rectify this issue and proactively identify opportunities to optimise efforts to treat and prevent wasting as part of ongoing stunting programming. Opportunities to integrate stunting and wasting programming exist at provincial level and some progress is being made, as described in Box 1.
At federal level, a provincial nutrition project (PC1) was initiated in 2020 for the next five years entitled, "Tackling Malnutrition Induced Stunting in Pakistan". This started as a stunting prevention initiative but, as a result of ongoing discussions with the provinces and considering the high prevalence of wasting in the country, a strong wasting management programme has been integrated within it. This PC1 will reach around 35% of Pakistan’s population, targeting the most poor, underprivileged and hardest to reach populations in Pakistan, at a cost of around USD2 billion over five years.
In order to accelerate the progress made to date, a comprehensive national and provincial level nutrition review is being planned. The intention is for this to inform the development of a consensus-based national nutrition policy and standardised nutrition programming approach to guide a more holistic, harmonised response that encompasses all major determinants and manifestations of malnutrition. This will be steered by the Ministry of National Health Services, Regulation and Coordination (MoNHSR&C) and the Ministry of Planning, Development & Reform (MPD&R) with technical support from UNICEF. Key to success will be a clear approach to improve the nutritional status of pregnant women and adolescent girls, the effective coordination and engagement of stakeholders, central oversight and effective monitoring. An ideal platform to provide this is the Pakistan National Nutrition Coordination Council (PNNCC) of the Prime Minister’s Secretariat. Currently, the Provincial Directorate Health General from each province and MoNHSR&C report progress on nutrition programming to the PNNCC which makes this a natural coordination platform. The Ministry of Finance and Planning Commission must be engaged to ensure adequate financing of nutrition initiatives at federal and provincial/ regional levels.
Box 1: Current initiatives and opportunities to integrate wasting and stunting programming at provincial level
In Punjab, a provincial nutrition project (PC1) is in place covering nutrition-specific interventions including the management of severe acute malnutrition (SAM), infant and young child feeding interventions and the delivery of multiple micronutrient supplements (MMS) to children and pregnant and lactating women. This is delivered through the Integrated Reproductive, Maternal, Newborn & Child Health and Nutrition (IRMNCH&N) Programme, the largest programme delivering nutrition services in all districts in the province. Separate to this, the Chief Minister’s Stunting Reduction Programme (encompassing a similar set of nutrition-specific interventions and nutrition-sensitive interventions spanning WASH, education, social protection and food security) is implemented in the seven districts of Southern Punjab with the highest levels of stunting in the province. Very little coordination and linkage can currently be observed between these two flagship programmes in the province.
In Khyber Pakhtunkhwa, the integration of health services delivery is being rolled out across 25 districts through an existing PC1. This integrates maternal nutrition and child health services, the Lady Health Workers (LHW) programme, wasting treatment and the expanded programme of immunisations. However, coverage is only around 20% owing to the lack of human and financial resources to enable scale. Recently, a multi-sectoral nutrition programme was implemented in Khyber Pakhtunkhwa, named KP SPRING. The objective of this programme is to reduce stunting in the southern part of the province with a target coverage of around 50%. The programme includes a range of nutrition-specific interventions (infant and young children feeding (IYCF) counselling, MMS and zinc for children, iron and folic acid (IFA) for pregnant women and nutrition counselling) and nutrition-sensitive interventions involving the following government departments: agriculture, livestock and fisheries, population welfare, education, public health engineering, local government and rural development and social welfare. This programme has a weak integration with the ongoing wasting treatment programme (integrated into health service delivery) given the narrow cross-over in terms of geographic location.
In Sindh, a ten-year multi-sectoral Accelerated Action Plan (AAP) for Reduction of Stunting and Malnutrition comprises both nutrition-specific and nutrition-sensitive interventions and is being implemented through eight sectors. In districts where the AAP is being implemented, approximately 58% of health facilities operate an Outpatient Therapeutic Programme (OTP) for the treatment of severely wasted children. Coverage of the World Food Programme implemented Targeted Supplementary Feeding Programme (TSFP) services for the treatment of moderately wasted children and pregnant and lactating women in the province is estimated to be only 3.6%.
In Balochistan, emergency and drought nutrition responses exist in 13 districts with almost 13% of health facilities providing services to treat SAM and to promote and support IYCF. Since December 2019 there has been no active PC1 for nutrition and therefore almost no government-funded nutrition programming in the province. Partner-driven stunting reduction programme initiatives exist in a few geographical locations. Funds for both wasting and stunting reduction programmes are external and emergency driven.
Gilgit Baltistan has recently approved a community-based nutrition PC-1 for all districts encompassing mostly preventive nutrition interventions.
In addition to the PC-1 programmes in each province, there are donor funded nutrition programmes currently operating in Sindh, KP and Balochistan with varied coverage.
Conclusions
Pakistan is confronted with a triple burden of wasting, stunting and childhood overweight and obesity. The country must move away from the vertical programming that addresses each manifestation of malnutrition separately towards the management of all children who are not growing well. Decision-makers must consider the full range of compromised growth and develop programmes that address both wasting and stunting at scale, also expanding this to encompass the reduction of childhood overweight and obesity. A national nutrition policy, informed by data from the National Nutrition Survey, is yet to exist in Pakistan but is crucial to accelerate progress. Another important strand is the integration of wasting management within the Primary Health Care (PHC) system to rapidly scale up and increase the coverage of wasting treatment services country-wide. Such efforts must be linked with multi-sectoral stunting reduction strategies to optimise efforts to address the multi-faceted causes of both manifestations of undernutrition within the country
For more information please contact Saba Shuja.
References
Briend A, Khara T, Dolan C. (2015). Wasting and stunting--similarities and differences: policy and programmatic implications. Food Nutr Bull.;36(1 Suppl):S15-23. PubMed PMID: 25902610
Government of Pakistan, Ministry of National Health Services, Regulations and Coordination, Nutrition Wing (2018) National Nutrition Survey 2018
Harding, K. L., Aguayo, V. M., & Webb, P. (2018). Factors associated with wasting among children under five years old in South Asia: Implications for action. PLoS ONE 13(7): e0198749. https://doi.org/10.1371/journal.pone.0198749
Kim, R., MejÃa-Guevara, I., Corsi, D.J., Aguayo, V.M., Subramanian, S.V. (2017). Relative importance of 13 correlates of child stunting in South Asia: Insights from nationally representative data from Afghanistan, Bangladesh, India, Nepal, and Pakistan. Social Science & Medicine, 187, 144e154.
Richard SA, Black RE, Gilman RH, Guerrant RL, Kang G, Lanata CF, et al. (2012) Wasting is associated with stunting in early childhood. J Nutr. 2012;142(7):1291-6. doi: 10.3945/jn.111.154922. PubMed PMID: 22623393; PubMed Central PMCID: PMCPMC3374667.
Schoenbuchner S, Dolan C, Mwangome M, Hall A, Richard S, Wells J, et al. (2018) The relationship between wasting and stunting: A retrospective cohort analysis of longitudinal data in Gambian children from 1976-2016. Under submission. 2018.
Wasting-Stunting Technical Interest Group (WaSt TIG) (2018). Child wasting and stunting: Time to overcome the separation (2018). www.ennonline.net/resources/timetoovercometheseparation
1 Around 32.9% women received IFA during pregnancy. Of those who received IFA, 67.2% did not take them, 22% continued IFA until 90 days or more, 5.8% continued for less than 60 days and 5% for 60-89 days.
2 See article entitled, “Integration of essential nutrition interventions into primary healthcare in Pakistan to prevent and treat wasting: A story of change“
3 Nutrition-specific programming is under the Ministry of Health Services, Regulation and Coordination (MoNHSR&C)
4 See article in this edition entitled, “Integration of essential nutrition interventions into primary healthcare in Pakistan to prevent and treat wasting: A story of change“


