Expanding CMAM Surge beyond nutrition – towards a broader Health Surge approach
By Erin McCloskey, Kate Golden and Amanda Yourchuck
Erin McCloskey is a Public Health Nutritionist and independent consultant currently working for Concern Worldwide. Erin has over 15 years of experience supporting the development of resilient health systems, empowered communities and an improved understanding of the nutrition and water, sanitation and hygiene (WASH) intersect.
Kate Golden is Senior Nutrition Adviser at Concern Worldwide. Her career started in Ethiopia in 2003 in one of the early pilots of community-based management of acute malnutrition. Since then, she has worked in South Sudan, Sudan and Lebanon and supported Concern nutrition programming and strategy development in roughly 20 countries across Africa and Asia as a global adviser.
Amanda Yourchuck is an Emergency Nutrition Advisor for the United States Agency for International Development (USAID) Advancing Nutrition. She has over 10 years of experience supporting wasting treatment and prevention activities. Amanda was previously a Nutrition and Health Advisor with Concern Worldwide and served as the technical focal point for global CMAM Surge activities.
The authors would like to acknowledge the support of Lucy Lafferty, Concern Niger Nutrition Adviser, Diane Moyer, Regional Nutrition Adviser for Save the Children International and Christine Bousquet and Breda Gahan, Concern HQ Health Advisers, for their support in the development of this article.
Location: Global
What we know: Demand for treatment services for childhood diseases (particularly malaria, diarrhoea and acute respiratory infection (ARI)) surge in response to seasonal changes and shocks.
What this article adds: A broader Health Surge approach is emerging, prompted by health facility staff beginning to apply community-based management of acute malnutrition (CMAM) Surge principles to other childhood disease services. Lessons learned from implementing countries to date (Sierra Leone, Burkina Faso, Chad, Niger, Ethiopia and Mauritania), including during the COVID-19 response, have informed working definitions, key elements of a package and key principles of an approach currently modelled on the CMAM Surge steps. Health Surge can be viewed as a quality improvement approach that empowers health workers to better anticipate, prepare for and manage fluctuations in demand for essential nutrition and child health services at facility-level in real-time, in complement to wider disease surveillance and response mechanisms. Health facility staff set specific thresholds for single diseases of public health importance in their catchment area to inform decisions and action on health facility capacity; information can be aggregated at district or regional levels to reveal rising stress on the health system. Adaptability of the approach is key and should always consider the context, effectiveness, local and national ownership, process transparency and sustainability. Experiences indicate that the Health Surge approach should protect services for the most vulnerable and will benefit from local prioritisation of illnesses, the tailoring of threshold setting methods according to how local health services are organised and disease-specific surge actions. Digital monitoring approaches will help real-time monitoring. Existing global and regional technical working groups on CMAM Surge are now coordinating Health Surge efforts. Tools and guidance are currently being developed by Concern and will be piloted in Niger, Kenya and Mali by Concern and Save the Children from early 2021.
The evolving Health Surge approach
Seeing the value of applying community-based management of acute malnutrition (CMAM) Surge to their nutrition tasks, many staff and supporting non-governmental organisations (NGOs) have begun to apply its principles to other areas of their workload, most often to services for common childhood diseases (malaria, diarrhoea and acute respiratory infection (ARI)). Disease surveillance and response mechanisms exist – at least in theory – in most countries. The emerging Health Surge approach aims to complement these mechanisms by supporting real-time monitoring of key illnesses so that the planning and allocation of resources to address caseload fluctuations can occur before a health facility is overwhelmed.
Figure 1: Countries where elements of a Health Surge approach have been initiated with partner support
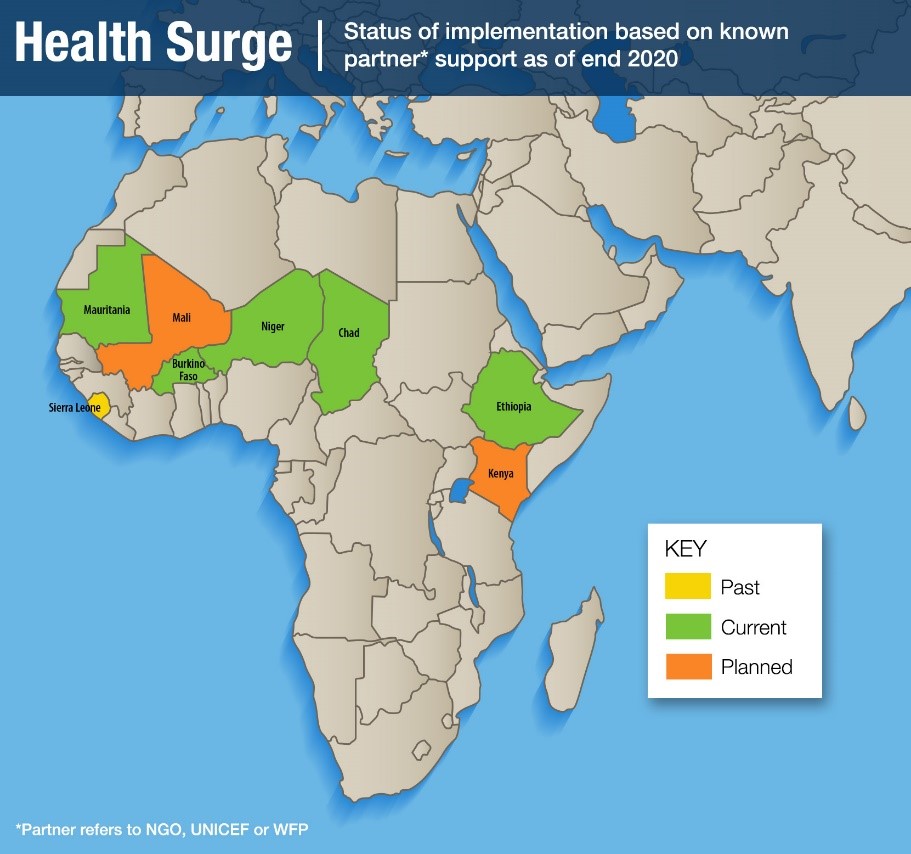
The concept of Health Surge was originally tried by health authorities in Sierra Leone in 2018 with support from Concern Worldwide (Concern) where existing CMAM Surge guidance was adapted for use in a malaria programme. Since the beginning of 2019, other stakeholders have been innovating and adapting CMAM Surge to the broader health agenda (Figure 1).1 Partners from Francophone West Africa came together recently to share early experiences from their Health Surge adaptations via the CMAM Surge Regional Taskforce (October 2020).2 The experiences shared highlighted the diversity of approaches taken and further underscored the need to agree on a common vision for the Health Surge approach while promoting further innovation and structured documentation and learning across contexts. Based on this experience, working definitions were developed by Concern in consultation with the Global CMAM Surge Technical Working Group (TWG) for both CMAM Surge and the emerging Health Surge approach (Box 1).
Box 1: Working definitions of CMAM Surge and Health Surge
CMAM Surge: The goal of the CMAM Surge approach is to support the health system, and empower health workers, to better anticipate, prepare for and manage fluctuations in the demand for wasting treatment services. It is the original surge approach and largely follows the Global CMAM Surge Operational Guide developed by Concern and the tools adapted for use in different countries.
Health Surge: The goal of the Health Surge approach is to support the health system, and empower health workers, to better anticipate, prepare for and manage fluctuations in the demand for essential nutrition and child health services. The modalities of this approach are currently being developed.
Within the broader landscape of health system strengthening, Health Surge is best viewed as a quality improvement initiative because it focuses specifically on refining the process of service delivery at health facility level, particularly during periods of peak demand. Quality improvement has been defined as “systematic, data-guided activities designed to bring about immediate improvement in healthcare delivery in particular settings” (Baily et al, 2007). Health Surge focuses on how services are organised and delivered to ensure that the correct services are provided where and when they are required. Health Surge aligns with the five principles of quality improvement activities (as outlined in Massoud et al, 2017):
- Client focused: Health Surge aims to protect the consistent delivery of services for patients, especially the most vulnerable, precisely at a time when quality is at risk of being compromised (health workers overwhelmed).
- Understanding work as processes and systems: Health Surge analyses existing capacity and processes for dealing with peaks in service demand and it looks to improve these to produce better results for clients and reduce the stress placed on health workers.
- Teamwork: Health Surge promotes collaboration between a health facility and health district management to foster ownership of the process. It also supports identification of key stakeholders for task shifting purposes during peak service demand periods such as community workers (health and other), cleaners, guards, etc.
- Testing changes using real-time data: Health Surge supports real-time data interaction and use, tracking changes in patient visits for different services against the capacity of the facility to cope, thereby ensuring service availability and quality when it is needed. Health facility teams should revise surge thresholds regularly based on any changes in their capacity which impact on their ability to manage caseloads.
- Shared learning: A learning review is built into the Health Surge approach on a monthly, annual and post-Surge basis.
This article provides a framework for Health Surge based on learning to date. The approach and related tools are still being developed and consolidated and will be shared throughout 2021.
Health Surge and existing disease surveillance and response systems
Since 1998, the World Health Organization (WHO) has been supporting Integrated Disease Surveillance and Response (IDSR) systems to ensure that diseases of public health significance are identified and responded to as needed.3 This system includes three categories for surveillance: epidemic prone diseases (e.g., Ebola), diseases targeted for eradication or elimination (e.g., measles) and other conditions of public health importance to a specific country. The first two disease categories require immediate notification to health authorities and have standard (usually national) thresholds that should trigger immediate action from the country’s outbreak response system. Health Surge is not intended to address these two categories of ‘notifiable diseases’ and replace their existing emergency response mechanisms. This was underscored and clarified by the experience of trying to adapt the CMAM Surge approach to COVID-19 which has now become a notifiable disease in most countries (see Case Study from Niger).
Case study: COVID-19 and CMAM Surge in Niger
In the early stages of the COVID-19 pandemic, it quickly became clear that even strong health systems in well-resourced countries had trouble coping with rapid increases in workload due to an influx of COVID-19 cases. In an effort to better prepare for and limit the risk of a similar scenario unfolding in Concern’s nutrition programme areas, Concern attempted to adapt its CMAM Surge guidance to the COVID-19 context. The pandemic served as an unexpected catalyst for defining a broader Health Surge approach that had already been under development for several years. Concern’s experience adapting CMAM Surge to the COVID-19 context in Niger provides the most practical learning. Ultimately, the adaptation of CMAM Surge raised more questions than answers but the experience has helped shaped thinking on the Health Surge approach, particularly what it can and cannot address.
Concern has been supporting CMAM Surge implementation in two health districts in the Tahoua Region of Niger since 2016, alongside other partners in other regions. From the outset of the pandemic, it was clear that COVID-19 had high potential to negatively affect wasting treatment services by a) increasing the number of individuals seeking treatment at health facilities, b) creating longer CMAM treatment consultation/review times due to heightened infection prevention and control (IPC) measures and c) reducing human resources due to staff being infected or re-prioritisation/ task shifting for certain services.
The main aim of adapting CMAM Surge to the COVID-19 context in Tahoua was to help health teams maintain quality treatment services for severe wasting while taking into consideration the additional challenges COVID-19 presented. However, given that health staff were likely to be overwhelmed by demand for services beyond just child health and nutrition, a new approach to tracking caseloads and assessing capacity was needed. Lastly, given the low testing capacity in Tahoua, the team saw potential for the new set of data they planned to track to be used to alert health authorities of possible spikes in COVID-19 cases.
The most immediate questions were: what data should be collected, how often and how should the data be used? The government’s disease surveillance system was already tracking and reporting confirmed COVID-19 cases where testing was available. Given the low testing capacity in Tahoua, however, the Concern team began exploring the feasibility of using fever, diarrhoea and/or acute respiratory infection (ARI) as a proxy marker for COVID-19 and setting some broader workload thresholds that would define when health facility teams needed to take additional measures or seek external support. Diarrhoea and ARI data are routinely collected on a monthly basis to feed into the Health Management Information System (HMIS) and are monitored (usually on wall charts) as part of CMAM Surge. Of these, data on ARI seemed to be the most relevant and accessible, as diarrhoea was not considered a reliable sign of possible COVID-19 infection and fever data was not readily available and/or not reliable unless combined with malaria testing results. Given COVID-19 cases are more prevalent in adults, the programme decided to track ARI cases for all age groups – not just in children under five years, as is done routinely in CMAM Surge.
However, there were practical challenges in the collection of ARI data that made it impossible to collect reliable data frequently enough to monitor the situation (weekly). The working definition of ARI data also varied between health facilities (pneumonia, severe pneumonia or cough and cold). Given these challenges, and the fact that the worst-case scenarios of COVID-19 were not fully realised in Niger, the Ministry of Health (MoH) and the Concern team decided the data was not reliable enough to inform surge actions. The health facilities therefore reverted to implementing normal CMAM Surge while the MoH continued to scale up IPC measures and expand testing to the degree possible.
While CMAM Surge did not prove to be a perfect fit for the COVID-19 context, the experience has helped to more clearly define the parameters required to adapt CMAM Surge to a broader health context and refine the development of Health Surge. This includes a better definition of the types of morbidities that are appropriate for threshold setting, the frequency of data collection, the feasibility of including multiple age groups and how to define appropriate action plans. More on these lessons is shared throughout this article.
The Health Surge approach is much more focused on helping health facilities to manage their workload during periods of increased caseload than on alerting health authorities to a possible outbreak. Health Surge is therefore more suited to the third category – major diseases, events or conditions of public health importance. These diseases are country-specific, based on a given epidemiological context, and reported on a monthly basis through the Health Management Information System (HMIS). Most countries have defined thresholds for this category of diseases, however, this is often “an observed increase in cases over time” or something more specific such as a doubling of caseloads compared to a five-year average. Such a vague definition is often difficult to act on in practice and, when applied, thresholds are often set as absolute case numbers at an aggregated level (district/regional/national) that do not allow for variations across health facilities. The thresholds also do not consider the health system’s capacity to respond at different levels. By the time an outbreak is declared at an aggregated level, the situation at individual health facilities may already be very serious.
The value of the proposed Health Surge approach is that it works to define specific thresholds for single diseases of public health importance appropriate to a given catchment area and within the context of health facility capacity. It does not interfere with standard reporting for these diseases but it does initiate earlier action at local level to protect service quality in the face of rising caseloads. As seen with CMAM Surge, when information on the number of health facilities passing their context-appropriate surge thresholds is aggregated at a district or regional level, it provides a powerful visual of not only the rising caseloads of malnourished children but the real stress the rising caseloads have on the health system.4 The Health Surge approach has the potential to introduce the same tailored approach to monitoring and managing increased caseloads of child illness in light of a health facility team’s own capacity to cope.
Health Surge in practice
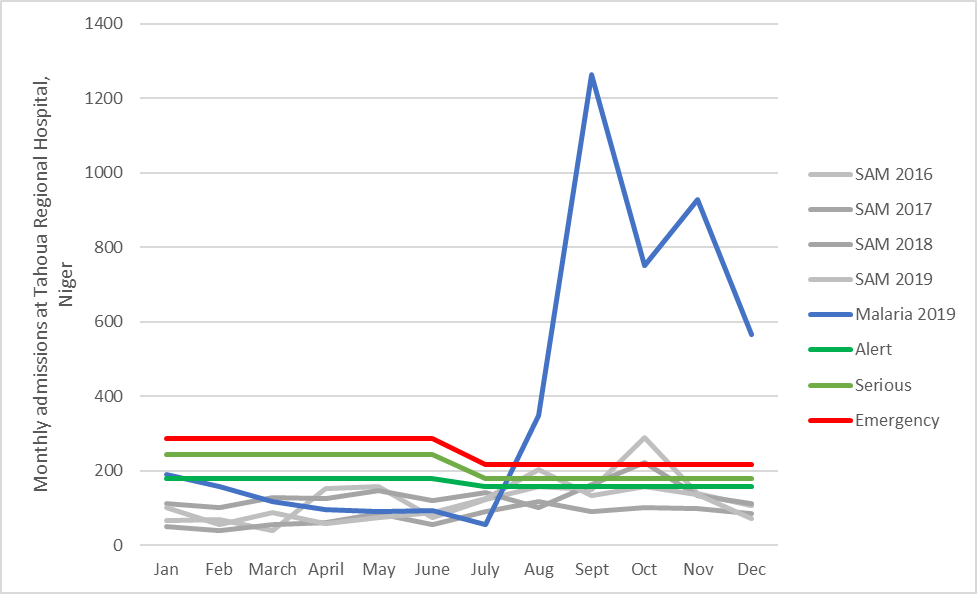
The value and potential of a Health Surge approach has been in evidence for years at the Tahoua Regional Hospital in Niger. The improved utilisation of monthly CMAM and other morbidity data by staff in the paediatric ward following engagement with the CMAM Surge approach led to a better understanding of the pressure that severe wasting and malaria both exert on the health system during the annual malaria spike (September/October). As a result, the hospital’s inpatient therapeutic centre now tracks malaria cases alongside malnutrition cases and lowers its CMAM Surge thresholds for the second half of the year to account for the reduced capacity of the facility due to the influx of malaria cases. Figure 2 shows wasting/oedema admissions (2016-2019) and CMAM Surge thresholds, contrasted with 2019 malaria admissions data.5
Figure 2: Severe wasting admissions and CMAM Surge dual thresholds, Tahoua Regional Hospital, Niger (2019)
In some contexts, seasonal peaks in wasting may not always materialise but other morbidities may still cause facilities to have increased workloads. In Ethiopia, severe wasting caseloads in the CMAM Surge pilot facilities were very low (most facilities saw fewer than 10 severely wasted children over the course of a month) with the majority of pilot facilities never passing thresholds or triggering Surge response actions. Instead of deciding that CMAM Surge was not helpful or relevant to them, health facility staff revised the approach and designed thresholds for diarrhoea cases instead. Bati woreda, where the Surge pilot took place, is particularly vulnerable to diarrhoea outbreaks and health facility workers have found the Surge process helpful for planning and bouncing back from outbreaks.
“CMAM surge has helped me understand and monitor the events in the community [that] affect the number of SAM cases coming here [to the health post]. I also monitor diarrhoea cases…knowing the events of this specific department helps us to prepare beforehand like securing... resources. For example, this is a rainy season with a lot of rain…it is common to have more diarrhoea, so this CMAM Surge will help us prepare for diarrhoea beforehand” Health Worker – Bati Heath Post, Ethiopia
Towards a common vision of the Health Surge approach
The Health Surge approach is currently evolving but several lessons can be drawn from the early experiences of those currently adapting CMAM Surge to address broader child health services. This includes the initial efforts to adapt CMAM Surge to support the COVID-19 response. This learning can move stakeholders towards a more coherent vision of a Health Surge approach. This will be essential to support the development of common programming tools, minimum quality standards and evaluation criteria which will be needed to refine and scale up the approach if it proves successful.
A key advantage of a Health Surge approach will, no doubt, be its adaptability. However, it is important that, wherever implemented, the Health Surge support package should foster:
Contextualisation: The approach should focus on severe wasting and the other illnesses in a given catchment area that contribute most to under-five mortality that place stress on the health system, exhibit fluctuations within or between years and are reasonably predictable. In addition, it should support and never duplicate existing outbreak response mechanisms where they exist.
Effectiveness: As a quality improvement initiative, support should be tailored to the needs and capacities of the health system to protect the continuity and quality of these services during periods of peak demand and/or reduced health facility capacity.
Ownership: Health workers, governments and the community should be empowered and should determine when and how they require additional external support to better manage services.
Transparency: Thresholds, support packages and delivery modalities for the response should be agreed with all relevant parties.
Sustainability: The package of support should strengthen the health system in a way that accounts for and prepares for better management of emergencies, allowing for greater long-term resilience.
CMAM Surge or Health Surge?
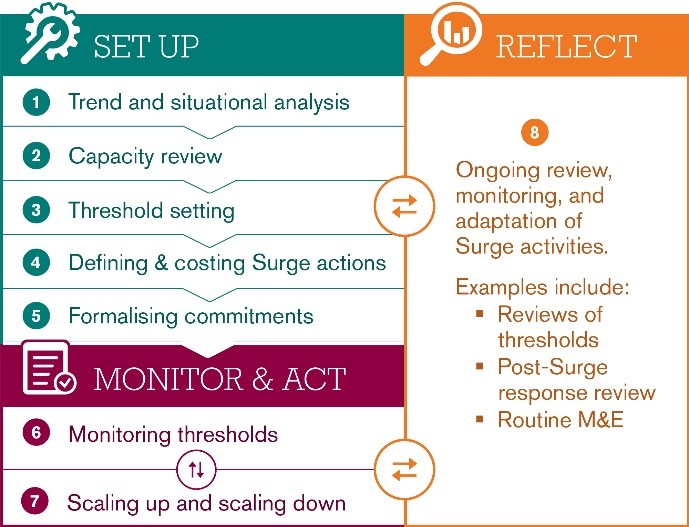
Many practitioners now trialling Health Surge have a solid background in CMAM Surge which has made the shift to include other child morbidities smoother. Others, however, have started directly with Health Surge and any new health facility or health district team may choose to do the same if they face significant surges of child wasting and common childhood illnesses. Some countries or areas may opt to simply continue with CMAM Surge or potentially start with CMAM Surge and introduce additional morbidities as their experience grows. In all cases, it is useful to move gradually through each of the eight steps of the CMAM Surge approach (see Figure 3) consolidating experience after each.
Figure 3: CMAM Surge steps
What have we learned that can inform development of a Health Surge approach?
Nutritionists must engage more with our health sector colleagues
CMAM Surge, while founded on shared health system strengthening and quality improvement principles and implemented by health facility staff and District Health Teams, was developed largely by nutrition experts. Developing the full Health Surge approach will require deeper engagement with a wide variety of health system actors and government departments including those responsible not just for child health (which may in fact cut across multiple departments) but for disease surveillance and response. The MoH in each country must be engaged and lead the development of a Health Surge approach. The fact that so many health facility staff in various countries have already initiated or embraced a shift from CMAM Surge to a more holistic Health Surge approach is a good sign but further engagement across all levels of the health system is now needed to solidify the approach.
Keep the focus on child survival
Many factors can drive health facility workload and capacities. There may be a temptation to try to address all health facility and health system challenges via a single approach but it is important to stay focused on protecting services for the most vulnerable: children under five years of age who are most vulnerable to wasting and illness and where interventions can have the most significant impact on mortality levels. While some programmes may set thresholds that consider services for a variety of age groups to account for their contribution to overall workload, the CMAM Surge and Health Surge are best suited to services to ensure continuity and quality of child health and nutrition services.
Determine priority illnesses to monitor
Which illness to track should be determined at health facility level based on the catchment population’s main burden and seasonal trends. It might be helpful, however, to first create a master list of morbidities that are of public health concern within a given district or region based on historical analysis of health data and seasonal trends.6 Health facilities could then select from this master list, based on the epidemiology of their catchment area. Many health facilities are already following key illnesses, as can be seen in Figure 4. It may also be useful to track an overall indicator of total consultations as a general indicator of workload fluctuations (see below). The availability and reliability of data via the existing HMIS and any other data collection mechanisms must also be taken into consideration when selecting which morbidities to consider, as highlighted in the COVID-19 case study.
Figure 4: Monthly wasting and morbidity consultations, Inkarkada Health Centre, Tahoua, Niger (Concern Worldwide 2018)
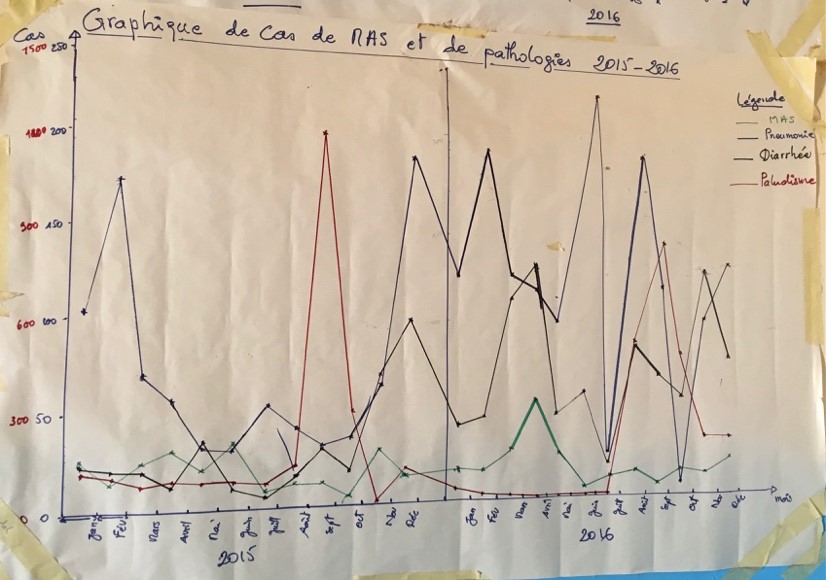
In this figure the green line represents severe acute malnutrition, the red line malaria, the blue line pneumonia and the black line diarrhoea.
The setting of thresholds needs to consider how health services are organised at facility level and how they realistically link to action
As articulated elsewhere,7 setting thresholds is a complex process that already poses challenges within the standard CMAM Surge model. Those who have already started Health Surge pilots have experimented with different threshold types. These fall into four main categories:
- Several single thresholds: facilities set and follow a maximum of three illnesses (severe wasting and two morbidities), creating separate thresholds for each.
- A multi-morbidity threshold: facilities create an index that aggregates severe wasting and several selected morbidities into a single threshold. Together they are meant to reflect both the illnesses that are the biggest risk to child survival as well as workload.
- A total consultations threshold: facilities simply track total consultations coming into the facility, generally regardless of age or service, to serve as an overall reflection of workload.
- Combination model: facilities track two of the above, usually several individual illnesses (severe wasting and maybe one or two other morbidities) and a total consultations threshold.
These threshold approaches are still a work in progress but may provide a helpful starting point for stakeholders embarking on the Health Surge approach who could then adapt to their context and share learning as they proceed. As above for the focal morbidities, it is recommended that a common approach to threshold setting is established for at least one district and ideally a whole country. This will allow for easier aggregation of Health Surge data to district, province and national levels.
An important factor when deciding which type of threshold approach to use is how the various services are organised at a health facility which determines patient flow and staff workload. In scenarios where a few staff are providing all services at a health facility, the ‘total consultations’ threshold may be most relevant. In scenarios where facilities have a larger, more varied group of staff with specific responsibilities and/or where wasting treatment services are still not well integrated into other outpatient services (and are delivered by different staff), ‘several single thresholds’ may be more appropriate. Health facility patient flow is usually determined by national guidelines for primary healthcare. These policy documents can help Health Surge practitioners decide on a common threshold approach for all facilities of the same type in a given country or district. A standard approach through an administrative region will be necessary, otherwise aggregation into district level dashboards will not be possible.
However, when determining how to set thresholds, it is important to think through how thresholds link to action planning and funding. While some actions may be the same regardless of morbidity (e.g., the need for additional staff), others will be disease-specific (e.g., buffer stocks of ready-to-use therapeutic food (RUTF) for increases in severe wasting, more malaria tests and drugs ahead of the peak malaria season or hygiene messaging during a diarrhoeal outbreak). If multi-morbidity or total consultation thresholds do not identify and/or account for which services are driving workloads up, then it may be difficult to trigger appropriate action based on Surge action plans. The ideal scenario may be to identify and set individual thresholds for the key conditions and morbidities that fluctuate and impact on staff workload while at the same time monitoring total consultations. If key conditions and morbidities have been properly defined then flucutations in total consultations during the year are mostly likely due to these. Following total consultations will help to clarify this and indicate if a major cause of health system stress has been missed.
Digital data solutions are even more vital when monitoring multiple indicators that include illness
As thresholds become more complex – beyond solely child wasting admissions (as in CMAM Surge) – digital systems for data gathering and synthesis become even more important. While monitoring several thresholds at health facility level will be feasible, monitoring the number of facilities that have passed their multiple thresholds at a higher level, such as distict or region, to detect a more system-wide emergency may be challenging. Digital, cloud-based data systems that are linked into governments’ District Health Information Systems (DHIS), disease surveillance and early warning systems will be critical to to ensure real-time monitoring. However, digitisation of data collection must not compromise a core component of the Surge approach which is to engage health staff at facility level to interact with and use their data for local decision making. Digital data systems should optimise data-driven decision making at all levels as CMAM Surge evolves further into the Health Surge approach.
Where to begin?
The development and implementation of the Health Surge approach must be grounded in the national and local health systems and embedded within or synchronised with other health system strengthening and quality improvement efforts and be based on a strong understanding of the capacity of the health system at different levels. On a practical level, it can borrow heavily from the tools and guidance that have successfully supported the scale-up of CMAM Surge. Therefore, revisions to the existing CMAM Surge Operational Guide will form the basis for the Health Surge approach. All eight steps from CMAM Surge will remain the same for Health Surge for the time being, although this may be adjusted as we learn. The main changes occur at the planning stage and in steps 1 to 4 (Figure 3).
Where steps are adapted, this will involve expanding the data collected, the thresholds set and monitored, capacities assessed and surge activities identified. More guidance on this is forthcoming in early 2021 from the Global CMAM Surge Technical Working Group which is currently led by Concern and includes representation from UNICEF, MoH Kenya and other agencies engaged in implementing or funding CMAM Surge.
Next steps
A Health Surge approach holds great promise for complementing ongoing health system strengthening efforts by increasing the shock-responsiveness of health systems at certain times of the year and beyond those for the treatment of child wasting. The approach still needs to be fully elaborated through engagement with a wide range of partners and its overall acceptability and effectiveness in improving the management of health services must be tested and further documented. The West Africa CMAM Surge Regional Taskforce8 will continue to facilitate its members to share the experience of trialling different aspects of the Health Surge approach. Meanwhile, the Global CMAM Surge TWG, led by Concern, will develop and support a coordinated plan to gather, document and share evidence and experience from the implementation of the Health Surge approach during the course of 2021. In addition, the Global CMAM Surge TWG is actively seeking to expand health sector representation throughout 2021.
In coordination with the Global TWG, Concern is working to develop a set of practical Health Surge tools that will be piloted in a coordinated fashion in Niger, Kenya and Mali by Concern and Save the Children from early 2021. These tools will be adapted from the existing CMAM Surge Operational Guide and toolkit and will be available to any health authorities or organisations looking to expand on the success of CMAM Surge. Learning from the pilot and other country experiences will be documented and shared throughout 2021 and will result in the revision of the current CMAM Surge Operational Guide into a global guide and toolkit for Health Surge by the end of 2021. Ministries of Health and other partners could then use this as a basis to develop their own tools and guidelines for their own country contexts based on their needs and wider health system strengthening activities.
Subscribe freely to receive Field Exchange content to your mailbox or front door.
Endnotes
1 As per Figure 1, this includes Ministry of Health (MoH) staff in Niger and Chad with support from the Croix Rouge Française (CRF) and Concern, in Mauritania with support from FRC, in Burkina Faso with support from Terre des Hommes and in Ethiopia and Sierra Leone with support from Concern.
2 Partners who participated in the webinar included NGO representatives, UNICEF staff and donor organisations.
4 See field article in this special section of Field Exchange entitled, “Implementing the IMAM Surge approach – experiences from Kenya”
5 2019 malaria admissions data demonstrate an illustrative malaria admission trend.
6 In most cases, this list likely already exists under Integrated Disease Surveillance and Response (IDSR) protocol.
7 See field article in this special section of Field Exchange entitled “CMAM Surge – lessons learned on the journey so far”
8 See field article in this special section of Field Exchange entitled “The Role of Coordination in CMAM Surge Scale-up in West and Central Francophone Africa ”
References
Liu, L., Johnson, H.L., Cousens, S., Perin, J., Scott, S., Lawn, J.E., et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet, 2012;379:2151-61. Medline:22579125 doi:10.1016/S0140-6736(12)60560-1
Lynn, J., Baily, M.A., Bottrell, M., et al. The ethics of using quality improvement methods in health care. Ann Intern Med. 2007;146:666–73. [PubMed], quoted in Patient Safety and Quality: An Evidence-based handbook for nurses. Hughes RG, editor.
International Vaccine Access Center (IVAC), Johns Hopkins Bloomberg School of Public Health. (2015). Pneumonia and Diarrhea Progress Report 2015: Sustainable Progress in the Post-2015 Era. Retrieved from www.jhsph.edu/research/centers-and-institutes/ivac/ resources/IVAC-2015-Pneumonia-Diarrhea- Progress-Report.pdf
Massoud, M.R., Gutierrez, R., Ottosson, A. (2017). Improving Health Care eLearning Course. Published by the USAID Applying Science to Strengthen and Improve Systems (ASSIST) Project. Chevy Chase, MD: University Research Co., LLC.
Massoud, M.R., Kimble, L. (2018). The USAID ASSIST Project’s approach to improving health care in low- and middle-income countries. Technical Report. Published by the USAID ASSIST Project. Chevy Chase, MD: University Research Co., LLC (URC).


