The ‘CMAM Surge’ approach: setting the scene
By Amanda Yourchuck and Kate Golden
Amanda Yourchuck is an Emergency Nutrition Advisor for the United States Agency for International Development (USAID) Advancing Nutrition. She has over 10 years of experience supporting wasting treatment and prevention activities. Amanda was previously a Nutrition and Health Advisor with Concern Worldwide and served as the technical focal point for global CMAM Surge activities.
Kate Golden is Senior Nutrition Adviser at Concern Worldwide. Her career started in Ethiopia in 2003 in one of the early pilots of community-based management of acute malnutrition. Since then, she has worked in South Sudan, Sudan and Lebanon and supported Concern nutrition programming and strategy development in roughly 20 countries across Africa and Asia as a global adviser.
The authors acknowledge the support of Chris Pain, Head of Technical Assistance at Concern Worldwide and Regine Kopplow, Senior Food and Nutrition Security Adviser, in the writing of this article.
Community-based management of acute malnutrition (CMAM)1 will celebrate its twentieth anniversary this year. Since its inception in Ethiopia in 2000, and subsequent pilots by Concern Worldwide (Concern) in partnership with Valid International in Malawi (2002) and Ethiopia (2003), it has evolved from a primarily non-governmental organisation (NGO)-driven emergency response to an increasingly integrated part of government-run child health services. Now more than 70 countries are implementing CMAM, many where treatment is integrated into routine basic health services (UNICEF, 2014). An estimated 5.2 million children with severe wasting accessed treatment in 2018. While this shows a remarkable increase from the first pilot, it still only represents 31% of the 16.6 million severely wasted children in need (State of Acute Malnutrition, 2020).
Despite CMAM’s incredible contribution to the management of child wasting,2 it is clear that more must be done to strengthen and increase coverage of services for wasting within health systems to ensure all children who need life-saving treatment receive it. Concern has continued to identify ways to improve the quality of and access to CMAM services as a core part of its nutrition and health programming. This is achieved through support to existing government health systems, more direct service provision in emergencies where necessary and by piloting new, innovative approaches.
The CMAM Surge approach is one of many ongoing efforts to improve the efficiency and effectiveness of treatment services for wasting during both normal and emergency periods (Kueter et al, 2018; McGrath & Shoham, 2019). The approach uses routine CMAM services as an entry point to strengthen the capacity of health systems to better anticipate, prepare for and respond to peaks in caseloads of wasted children.
The need for a more predictable, sustainable approach to responding to caseload increases, particularly when they reach emergency levels, was first articulated in Field Exchange in 2010. In their article, Suggested New Design Framework for CMAM Programming, Peter Hailey and Daniel Tewoldeberha (2010) highlighted the challenges of CMAM programming as it was typically implemented at that time. They described the seasonal vulnerability of livelihoods and other local systems that drive predictable spikes in CMAM caseloads at particular times of year. The article challenged the traditional ‘stop-start’ emergency response model that failed to adequately address these caseload spikes as responses often began too late, missing the most opportune time to save the most lives. In addition, the article highlighted that traditional emergency responses often led to disruptions in health systems strengthening initiatives, given their parallel nature, and that additional capacity was withdrawn at the end of an emergency, leaving nothing behind to build upon when the next emergency inevitably occurred. Emergency responses relied heavily on external capacity and support from NGO and United Nations (UN) partners which, while meeting immediate needs and providing life-saving support, did not enable governments to build more sustainable country-led response systems.
Around the same time, Concern began searching for ways to improve its own response to nutrition emergencies. Despite decades of experience managing wasting in both emergency and non-emergency settings (including at least a decade before the development of CMAM), Concern faced many of the same challenges and frustrations articulated in the Hailey & Tewoldeberha article.3 While it was clear that Concern and government health staff in most countries were well aware of the local warning signs of an imminent nutritional emergency, this knowledge was not being sufficiently leveraged to trigger early action. Concern also saw that capacity varied considerably between health facilities and that relatively modest but tailored support could help health teams better cope with increases in demand for services. Finally, Concern could see that CMAM admission numbers could be a practical and efficient trigger of timely support but they needed to be understood relative to historical trends and a health facility team’s own capacity to respond. Based on experience from multiple countries, this prompted Concern to develop and pilot what is now known as the CMAM Surge approach in Kenya in partnership with the Kenya Ministry of Health and UNICEF beginning in 2012 (Kopplow et al, 2014).
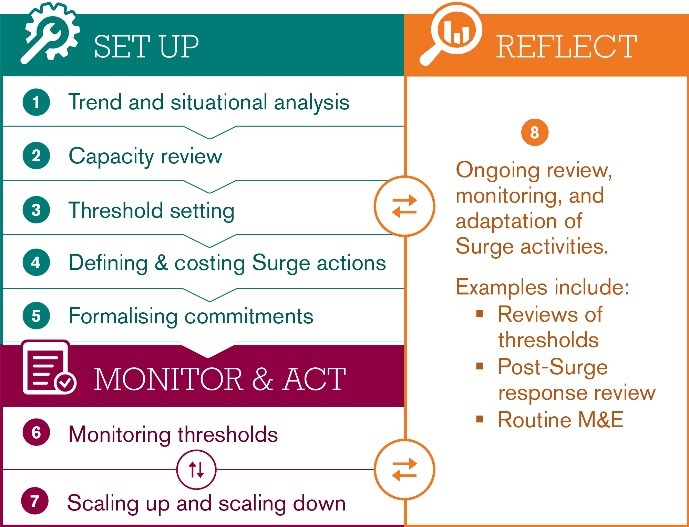
The CMAM Surge approach uses eight steps to help government health teams respond to relative changes in capacity and caseloads (Figure 1). These steps begin with an analysis of the local context, including a review of seasonal trends and known risk factors that drive child wasting rates (Step 1) and individual health facility capacity (Step 2). The analysis process culminates in the setting of health facility-specific thresholds that, when crossed, trigger a shift from normal implementation into a higher phase of action based on the severity of the situation (alert, serious, emergency) (Step 3). Pre-agreed Surge actions and support from both government and non-government actors are agreed (Step 4 and 5) and activated (Step 7), with the first level of action often being taken from within the health facility itself, sometimes in collaboration with communities. Thresholds are monitored on an ongoing basis by health facility staff using routine health facility data (Step 6), enabling action as soon as a threshold is crossed. The status of each health facility is also monitored by the higher level health authority (e.g., district health management team) that can, in turn, monitor trends across a wider geographic area and call for higher-level regional or national response if the situation continues to deteriorate.
Figure 1: The CMAM surge approach
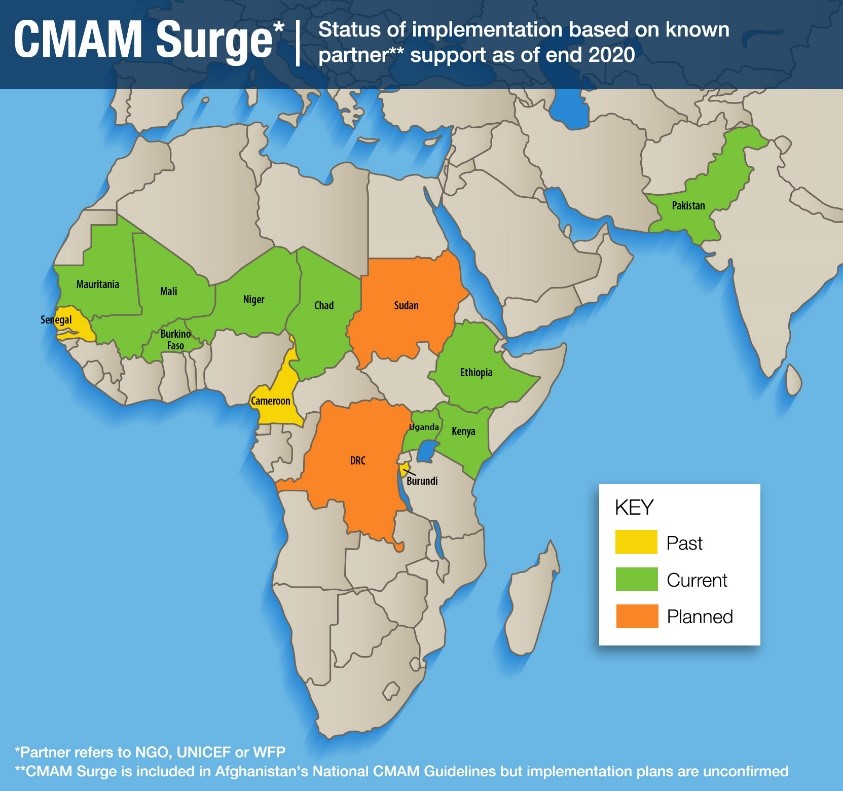
Now, nearly eight years later, CMAM Surge is being implemented in 12 countries with technical assistance to governments provided by multiple NGO and UN partners and financial support from both development and emergency donors across humanitarian and development contexts (Figure 2). Concern has had a direct implementation presence in seven4 of these countries. In other countries, partners have either introduced CMAM Surge on their own using Concern’s CMAM Surge Operational Guidance or worked in coordination with Concern to bring CMAM Surge to scale with multiple implementing partners. During this time, a wealth of knowledge has been generated that points to lessons learned and best practices. It is important to now take stock of what we know and chart the way forward for practitioners to further refine and scale up the approach.
Since 2012, both CMAM programming and the contexts in which Concern supports delivery of treatment services for wasting have changed, demanding new thinking on how to best adapt and scale up health systems strengthening approaches such as CMAM Surge where they are most needed. Services are being delivered in increasingly challenging contexts against a backdrop of protracted crises with varying levels of government capacity and support. Seasonal patterns are being disrupted by climate change and more systemic issues such as supply chain breakdowns as well as security and economic factors disrupt health seeking behaviours and patterns in service delivery and uptake. With the Covid-19 pandemic pushing health systems to their limits and challenging our traditional way of delivering CMAM services, this stock-taking is even more timely.
Figure 2: Countries implementing surge CMAM
This series of articles highlights the accomplishments and experiences of a wide range of CMAM Surge practitioners and other stakeholders. We begin by sharing experiences from Kenya, home of the original CMAM Surge pilot, where scale-up and innovations in CMAM Surge continue. We then turn to francophone West and Central Africa where CMAM Surge was rapidly scaled up by NGO implementing partners across the Sahel from 2018-2019. We examine the cost-effectiveness of the approach in light of its aim to optimise the efficiency of treatment service delivery, particularly during peak periods. The potential elements of a Health Surge that seeks to apply CMAM Surge principles to a broader set of child illnesses is then outlined. Finally, we reflect on key lessons learned through both formal evaluations and diverse field experiences to help guide the way forward for the continued refinement and scale-up of the approach. We hope that this series is a useful consolidation of many years of rich learning that can contribute to the ongoing effort to bring wasting treatment services to scale, even in the most challenging of contexts.
Subscribe freely to receive Field Exchange content to your mailbox or front door.
Endnotes
1 CMAM aims to reach the maximum number of acutely malnourished children with treatment services at decentralised outpatient care sites. The CMAM approach consists of four main components: community outreach, outpatient care for the management of SAM without medical complications, inpatient care for the management of SAM with medical complications and programmes for the management of moderate acute malnutrition (MAM), such as a supplementary feeding programme (SFP).
2 There has been a recent shift towards use of the term ‘wasting’ rather than acute malnutrition to emphasise its importance outside ‘acute’ emergencies. Wasting is also easier to visualise and, therefore, more likely to move people to action. CMAM, however, treats both children who are wasted and/or have nutritional oedema.
3 For more information about Concern’s experience delivering CMAM and other wasting treatment services see the following two reports: https://reliefweb.int/report/world/concern-worldwide-s-learning-15-years-community-management-acute-malnutrition
4 Concern has implemented/is implementing CMAM Surge in Burundi, Chad, Ethiopia, Kenya, Niger, Pakistan and Uganda.
References
Hailey, P. and Tewoldeberha, D. (2010). Suggested New Design Framework for CMAM Programming. Field Exchange 39, September 2010. p41. www.ennonline.net/fex/39/suggested
Kopplow, R., Yishak, Y., Appleford, G. and Erasmus, W. (2014). Meeting demand peaks for CMAM in government health services in Kenya. Field Exchange 47, April 2014. p3. www.ennonline.net/fex/47/meeting
Kueter, AM., Prudhon, C., Keane, E. and Gayford, M. (2018). Report on innovations in CMAM. Field Exchange 58, September 2018. p41. www.ennonline.net/fex/58/reportoninnovationsincmam
McGrath, M. and Shoham, J. (2019). Editorial perspective on the continuum of care for children with acute malnutrition. Field Exchange issue 60, July 2019. p2. www.ennonline.net/fex/60/extendededitorial
State of Acute Malnutrition. Accessed on 14/12/2020. https://www.acutemalnutrition.org/en/countries
UNICEF. 2014. Nutridash 2013: Global Report on the Pilot Year. New York: UNICEF. https://unicefeapronutritionwashtoolkit.files.wordpress.com/2017/09/unicef-global-nutridash-report-2013.pdf.


