Implementing the IMAM Surge approach - experiences from Kenya
By Weldon Ngetich, Grace Gichohi, Francis Wambua, Tewoldeberhan Daniel, Yacob Yishak and Patrick Codjia
Weldon Ngetich is a Nutrition Specialist with Concern Worldwide in Kenya. He is an experienced Public Health Nutritionist with over 10 years of experience in nutrition programming in Kenya and other developing countries in Africa and Asia.
Grace Gichohi works with the Kenyan national government’s Ministry of Health, Division of Nutrition and Dietetics as the Program Manager, Nutrition in Emergency/Nutrition Commodities. She has extensive experience in integrated management of acute malnutrition (IMAM) programming in Kenya.
Francis Wambua has been a nutrition specialist with UNICEF Kenya since August 2015. Prior to joining UNICEF, he worked with the Ministry of Health Kenya as Nutrition Program Officer supporting Emergency Nutrition and Micronutrient Deficiency Control programmes for over 10 years.
Dr Tewoldeberhan Daniel is a Nutrition Specialist with UNICEF Kenya. He has over 15 years of experience working in public health and nutrition in Ethiopia, Sudan and Kenya and co-authored a suggested design framework for community-based management of malnutrition (CMAM) in 2010 that contributed to the initial conceptualisation of the IMAM Surge approach.
Yacob Yishak is Country Programs Director for Concern Kenya country office. He has over 15 years of experience in public health and nutrition in Africa.
Patrick Codjia is the Chief of Nutrition with UNICEF Kenya. He has previously worked on nutrition programmes for various UNICEF Offices (Eastern and Southern Africa Regional Office, Country Offices in Botswana, DRC and Malawi), an international non-governmental organisation (NGO) in Eastern Democratic Republic of Congo and a research centre in Burkina Faso.
Location: Kenya
What we know: The Arid and Semi-arid Lands (ASAL) of Kenya are prone to frequent droughts and floods and seasonal spikes in malnutrition, resulting in nutrition emergencies.
What this article adds: Following a successful Integrated Management of Acute Malnutrition (IMAM) Surge pilot in Marsabit County 2012-2014, Concern Worldwide (Concern), UNICEF and the Ministry of Health (MoH) scaled up the approach in 10 priority ASAL counties to improve health system shock-responsiveness. A national IMAM Surge toolkit was developed and training cascaded from national to health facility level. Data was shared at sub-county, county and national levels through an online ‘dashboard’. By June 2020, IMAM Surge was implemented in 63% of targeted ASAL county health facilities. The approach has enabled timely decision-making and planning of supplies and human resources in response to surges in demand, as demonstrated by a case study of Turkana county. Success factors include early and sustained government leadership and the involvement of decision-makers at sub-national level, the integration of IMAM Surge into key national and sub-national strategic planning documents, facility-level mentoring and on-the-job training, the empowerment of staff to appraise and react to data and online compilation of data. Challenges include the prioritisation of drought response over health system strengthening in acute situations, weak community-facility linkages and resource constraints which limited capacity for surge action. Plans include further scale-up in more health facilities and counties, the development of more formal linkages with broader early warning systems, the use of facility data to trigger seasonal preventive actions and trials of an IMAM Health Surge model.
Background
The Government of Kenya, as one of the signatories of the Alma Ata Declaration of 1978 and 2018,1 has a vision for the provision of sustainable Primary Health Care (PHC) services that are high-quality, safe, comprehensive, integrated, accessible, available and affordable for everyone, everywhere. In 2018, the president of Kenya declared Universal Health Coverage to be a national priority under the ‘Big Four Agenda’ for national sustainable development and has committed to make strategic investments in health to ensure that all residents of Kenya can access the essential health services they require by 2022 (MoHK, 2019). Unfortunately, frequent, large-scale disasters regularly challenge the realisation of this vision, leading to disruption of health service delivery and the frequent derailing of longer-term health system strengthening efforts.
Integrated Management of Acute Malnutrition (IMAM) in Kenya, adopted by the Ministry of Health Kenya (MoHK) in 2009 (previously supported by non-governmental organisations (NGOs)), has proven to be a high-impact and cost-effective approach for the treatment of wasting, enabling children with uncomplicated wasting to be treated as outpatients in the community (Collins, 2004). Treatment services for severe and moderate wasting are two of 11 High Impact Nutrition Interventions (HINI)2 (Lupao and Mogusu, 2019) that are integrated into routine health services for rollout via community health workers (CHWs) in areas with high burdens of malnutrition. In the past, the Kenyan health system responded to nutritional emergencies by mobilising external resources. This often led to a delayed, disjointed and inefficient response that negatively affected the quality, coverage and effectiveness of the services offered (Hailey & Tewoldeberha, 2010). It is increasingly recognised that health system strengthening (HSS) is needed in Kenya to improve the shock-responsive of the system to enable it to expand and contract in response to changing needs (Newton-Lewis et al, 2020).
The Arid and Semi-arid Lands (ASAL) of Kenya are spread across 23 of Kenya’s 47 counties. Historically marginalised and underserviced, Kenya’s ASALs are particularly prone to frequent droughts and floods, and nutrition emergencies and seasonal spikes in malnutrition are common. Consequently, the Kenyan government, with support from partners, has made significant investments to develop the capacity of county and sub-county authorities to manage emergencies. In an effort to build shock-responsiveness from within the ASAL health system, Concern Worldwide (Concern) and the Marsabit County Health authorities developed and piloted the IMAM Surge approach in 14 health facilities over two years from May 2012 to mid-2014.
A 2015 evaluation of the Marsabit pilot found the IMAM Surge to be feasible, effective and highly acceptable. As a result, MoHK endorsed the approach for implementation in other areas of Kenya with a high wasting burden. This article documents and shares lessons learned on the resulting scale-up of IMAM Surge in Kenya, highlighting the process, key successes and challenges to date.
Process for the rollout of IMAM Surge
There were several key phases in the rollout of IMAM Surge in the Kenyan context that contributed to its success, as follows:
Government leadership and development of IMAM Surge guidelines/tools
For any new initiative, a clear national policy and guideline is critical to ensure government ownership at all levels and to steer implementation. One of the first steps in the IMAM Surge rollout in Kenya was therefore to support the government to develop an IMAM Surge guide and toolkit, drawing from the experience of the Marsabit pilot. The toolkit was developed under the umbrella of the Emergency Nutrition Advisory Committee (ENAC) which hosted consultation meetings with key stakeholders to inform the process. A final guide/toolkit for health workers and a facilitator’s guide for trainers were ready for rollout by July 2016.3
A core team within ENAC was formed with representation from UNICEF, the MoHK and Concern to lead the rollout process in 10 ASAL counties with the highest burden of child wasting (Baringo, Garissa, Isiolo, Mandera, Marsabit, Samburu, Tana river, Turkana, Wajir and West Pokot). This was guided by a roadmap outlining the key steps and timelines for scale up at both national and county level. Key steps included the training of trainers, engagement with county/sub-county health management teams and other implementing partners, set-up at health facilities (Steps 1 to 4 of the IMAM Surge approach) and the development of a basic set of monitoring and reporting tools. The IMAM Surge toolkit was later integrated into county strategic planning documents including the County Nutrition Action Plan (2019-2023) and the County Integrated Development Plan (2018-2022). This has given IMAM Surge formal endorsement and a better chance for resource allocation during annual county budgeting processes.
Capacity development of key stakeholders via on the job training
A training of trainers (ToT) based on the IMAM Surge toolkit/guide and facilitators’ guide was conducted in September 2016. Course facilitators were drawn from MoHK national level, UNICEF and Concern and participants (IMAM Surge trainers) came from seven of the 10 target ASAL counties. These 15 national trainers subsequently went on to train 53 county/sub-county trainers from county health departments and implementing partners (including Save the Children, Action Against Hunger (AAH), Kenya Red Cross Society, World Vision Kenya, International Rescue Committee (IRC) and Concern). The county/sub-county trainings followed a standard four-day curriculum and focused on mentoring skills (to use with health facility staff) and the technical skills necessary to use the IMAM Surge toolkit. During the training, each county developed a detailed one-year roadmap for implementation and these have subsequently been revised annually based on learning and contextual changes.
Figure 1: The IMAM Surge approach steps
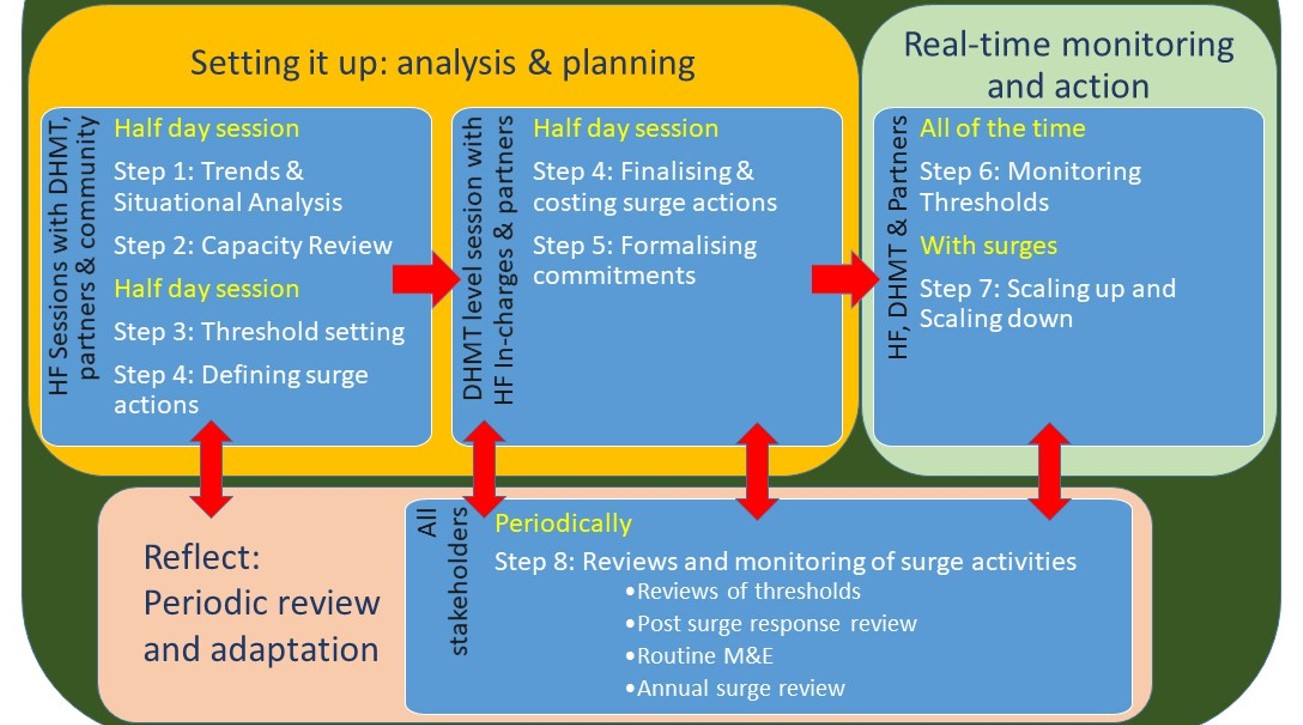
Before rolling out to health facilities, partners and national MoHK representatives engaged key decision/policy makers at county level, including County Health Management Teams (CHMT), the Chief County Officer in the Department of Health and the Director of Health, to build ownership of the approach and the rollout process.
Practical support to set up IMAM Surge at health facility level
Most of the counties adopted a mentorship/on-the-job training (OJT) approach whereby health staff were taken through each step of the IMAM Surge process at facility level. Others adopted a classroom training approach whereby health workers were trained centrally then moved to their respective facilities to set up IMAM Surge. Analysis from different counties showed that the mentorship/OJT approach was more successful because it allowed all health workers to participate in the process, provided adequate time to address individual facility issues and enabled the immediate development of clear, context-specific implementation and monitoring plans. The OJT set-up process was conducted in two to three sessions at each facility. A total of 469 health workers have received OJT to date. Once thresholds were defined and surge actions identified, health facilities were provided with monthly monitoring charts for real-time monitoring of thresholds and the tracking of planned surge action.
Active engagement of health staff in real-time monitoring of IMAM Surge data
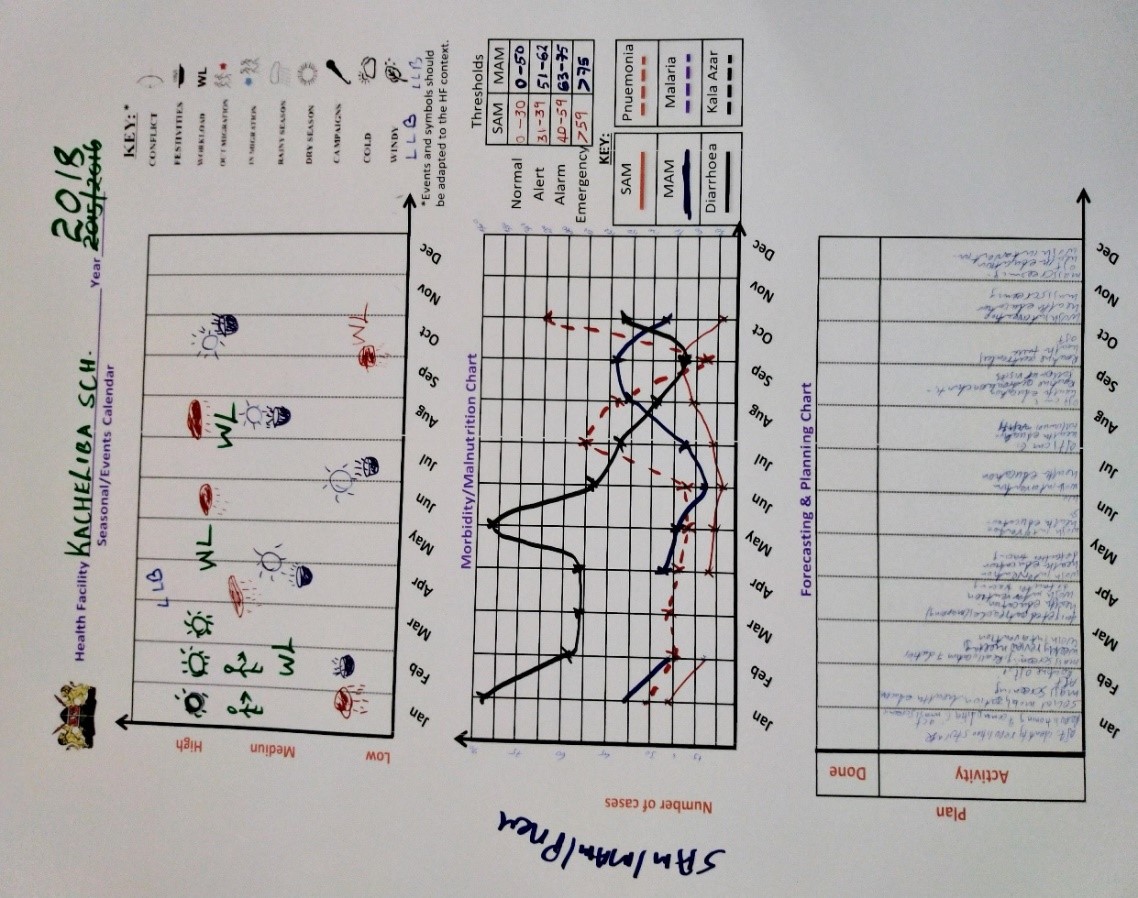
Monitoring caseloads and factors that may influence caseloads is an ongoing process throughout IMAM Surge implementation. At facility level, admissions of wasted children and activities that might affect care-seeking are monitored through facility registers and wall charts (Figure 2). Wall charts help health facility teams to visualise seasonal factors that affect caseloads (top chart in Figure 2), current monthly trends in moderate and severe child wasting admissions and child illness consultations compared to thresholds (middle chart in Figure 2) and identify actions that will be triggered if a threshold is passed (bottom chart in Figure 2). At the end of every month, health facility staff review their data to understand if either severe or moderate (or both) child wasting admissions are normal or have passed their respective alert, alarm or emergency thresholds. Actions are initiated accordingly and further actions planned for the coming three months if increases in cases are expected.
Figure 2: Kachelibasub county hospital monthly monitoring chart
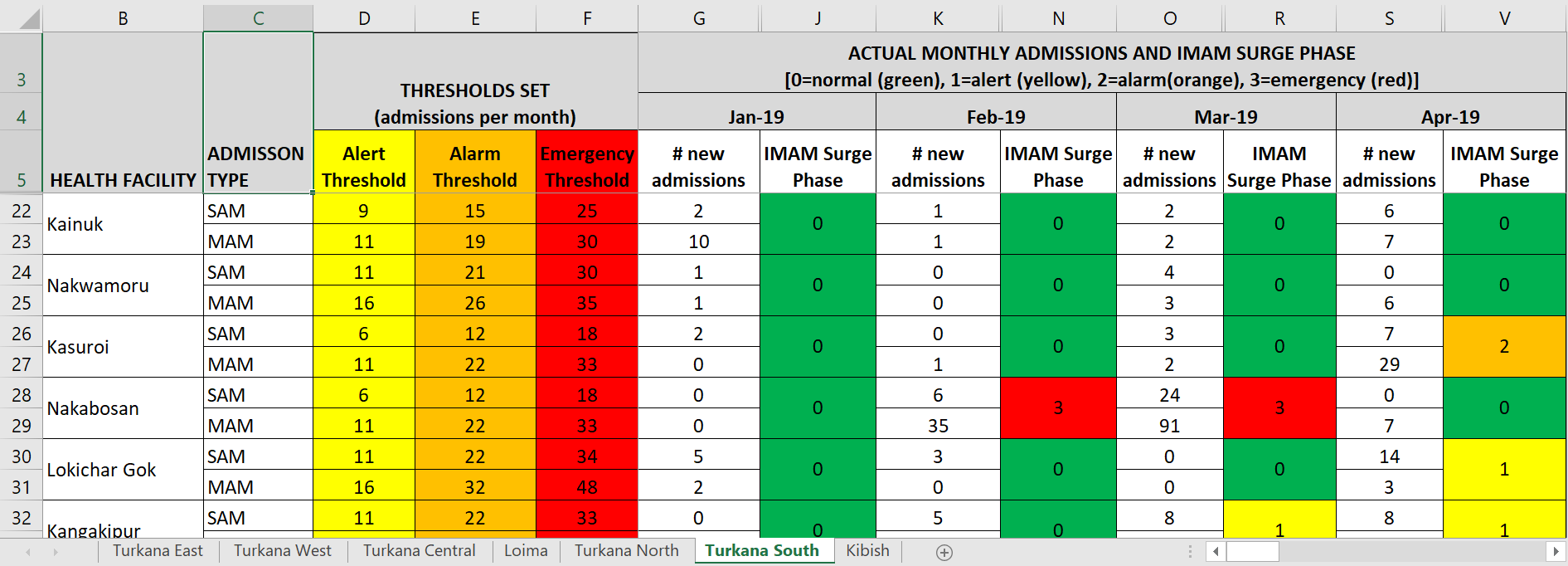
After summarising facility-level information, data on admissions and any thresholds crossed are shared with the sub-county Records Officer who enters the data into the online health information system. This data is used to update the IMAM Surge dashboard, a key monitoring tool of the Sub-County Health Management Team (SCHMT) (Figure 3) that uses colour codes to clearly show the proportion of health facilities that have passed their alert, alarm or emergency threshold. This provides a clear and quick overview of the nutrition situation across all the health facilities implementing IMAM Surge to support a timely response to increases in wasting levels. In general, more moderate acute malnutrition (MAM) cases than severe acute malnutrition (SAM) cases are observed across the sub-counties and MAM cases rise before SAM cases (although this is not always consistent and depends on the level at which thresholds have been set).
During the IMAM Surge scale-up in the ASALs, partners such as Concern scheduled regular joint follow-up visits to health facilities with the SCHMT followed by review meetings to support the real-time monitoring and analysis of data. Partners supporting rollout paid frequent visits to health facility teams during the initial stages to ensure that all the steps were well understood and correctly taken, particularly around the setting of thresholds. This has been essential to motivate and empower staff to understand when and why caseloads are increasing and to trigger action and communication on additional support needed.
Figure 3: IMAM Surge dashboard, example from Turkana South sub-county
Key successes
IMAM Surge is now in roughly two-thirds of health facilities in 10 priority ASAL counties
Within the 10 high-burden ASAL counties targeted for IMAM Surge scale-up, a total of 750 health facilities provide IMAM services. Of those, 469 facilities (63%) were implementing IMAM Surge as of June 2020.4 All facilities implementing IMAM Surge in the 10 counties monitor the nutrition situation through monthly wall charts while 29 sub-counties out of the total 45 located in seven of the 10 counties have active IMAM Surge dashboards. This high level of scale-up is largely due to the cascading of training from national to county level and health facility levels which enabled wide reach of health staff at multiple levels.
Increased demand for and use of local nutrition data in decision making
The IMAM Surge training and mentoring component has been effective in creating a culture of real-time analysis at facility, sub-county and county levels. It has developed an appetite for both data and the skills to use them for decision making. This has helped to improve, for example, the forecasting of therapeutic and supplementary feeding products and medical supplies needed monthly – as a result the majority of facilities reported zero stock-outs of ready-to-use therapeutic foods by 2018, aside from those resulting from national level supply chain gaps (MoHK, 2018). Health facility staff also use facility data to plan leave days during periods of low caseloads and in some cases to prompt CHWs to increase nutrition screening when data shows lower than expected caseloads.
Use of the dashboard by sub-county and county health teams has supported timely decision making and more evidence-based response planning. For example, the dashboard has been used to identify malnutrition ‘hotspots’ and direct appropriate monitoring and supervision. Surge data has also been used to advocate for the recruitment of additional staff for health facilities with higher caseloads, improving their ability to manage essential services during peak periods (MoHK, 2019). For example, when the Laisamis sub-county dashboard indicated health facilities were becoming overwhelmed, the county and sub-county allocated additional resources with support from partners to increase mass screening and referral (including paying for allowances for CHVs to work extra hours), expand service delivery through outreach services and increase monitoring and supervision to health facilities. At facility-level, health staff used the data to restructure their leave plans, recall staff on leave and provide direct support to CHVs for screening. The case study on Turkana provides a more detailed example of this (Box 1).
Box 1: Case study: Predicting nutritional emergencies: the case of Turkana County
Since the IMAM Surge scale-up began, Kenya has experienced two drought episodes, in 2017 and 2019. Turkana County, one of the most vulnerable counties in Kenya, was particularly affected. Data from SMART survey reports revealed global acute malnutrition (GAM) prevalence rates across the sub-counties of Turkana from 32% to 37% in 2017 and 20% to 31% in 2019. These were similar GAM prevalence rates to those of the 2011 crisis, however, unlike in 2011, IMAM Surge had been scaled up to the majority of health facilities and by 2018 IMAM Surge dashboards were in place for most sub-counties.
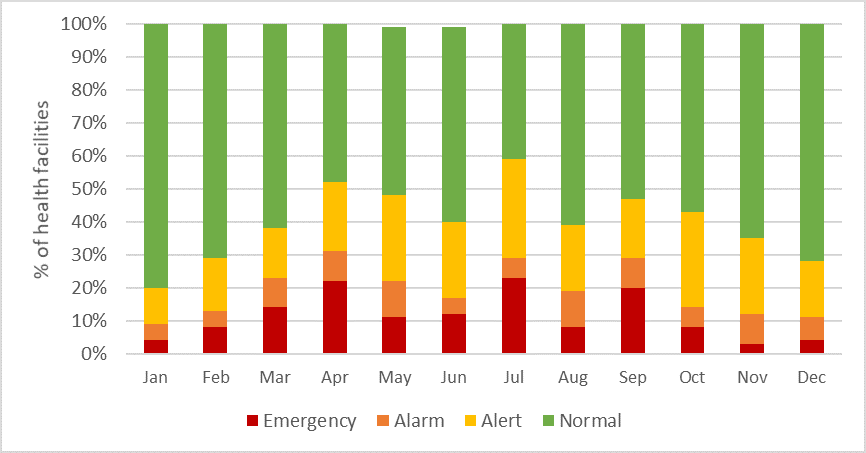
By March 2019, county stakeholders were detecting a deterioration of the nutrition situation via IMAM Surge dashboards. This raised an early alarm at different levels – even as other early warning indicators such as the Vegetation Condition Index (VCI) and prices of livestock and crops remained relatively normal or inconclusive (NDMA, 2019). Figure 3 shows the percentage of health facilities at ‘normal’, alert, alarm and emergency caseloads based on new admissions per month for 2019. The blue line marks the point at which 50% or more of health facilities are above their ‘normal’ thresholds – a warning to the County Health Management Team that health facilities are becoming critically overloaded by cases of child wasting. This state of alert for Turkana County mirrors very closely the VCI warning that the county was ‘moderately below normal vegetation’ for April, May and June. It also provided a sign of trouble as early as February and March while the VCI was still reported as ‘normal vegetation’.5
Figure 4: Percentage of health facilities in Turkana County above Surge thresholds 2019
The IMAM Surge early warning allowed Turkana County to put in place preparedness actions to manage increasing caseloads. Guided by IMAM Surge data and tools, the county developed an emergency response plan that included the mapping of outreach sites as well as budgeting for emergency actions and heightened coordination.
By July/August 2019 – normally the peak period for malnutrition –Turkana County was managing caseloads of child wasting better than during previous droughts. The IMAM Surge dashboards not only detected the emergency but helped to activate timely surge support packages from the County and Sub-county Health Management Teams and partners to prevent further deterioration. Some of the actions initiated by the county to address the situation included the scale-up of outreaches, mass screening, scale-up of household visits and active case finding. These activities were initiated earlier compared to previous emergencies.
Mentoring and technical support
During the rollout process, MoHK, UNICEF and Concern have continued to provide close technical support for monitoring and technical backstopping through field visits, remote technical discussions and annual reviews. The ASAL counties implementing IMAM Surge share their dashboards with the emergency focal person at the national MoHK monthly for review and to inform an update to the ENAC. This enables close engagement between national and regional government and the initiation of timely technical support when needed, including field visits for mentoring and monitoring. Periodically, the core team conduct monitoring support at county level on behalf of ENAC to ensure that the approach is implemented as per national guidelines and to provide any additional technical support needed.
Annual IMAM Surge reviews are conducted both at county and national level to generate and share learning. County level review meetings enable local stakeholders to share specific learning to help to refine the approach in context and national level review meetings draw participation from all 10 high-burden ASAL counties for broader learning and to inform guideline updates. For example, it was noted that the IMAM Surge dashboard automatically classified the nutrition situation using the number of new admissions (as per national guidelines) but this was not moving swiftly enough back to a ‘normal’ classification once the situation had stabilised. Based on this feedback, national IMAM Surge guidelines were revised so the dashboards use total enrolled cases (not new admissions) when deciding if/when a facility should return to a normal classification. This allows more resources to be more efficiently allocated to where they are most needed.
Lessons learned
Early and continued government leadership of the process, with support from other stakeholders familiar with IMAM Surge, was critical for the sustainability of the approach, supported by the joint development of a national IMAM Surge guideline, toolkit and roadmap to guide the initial rollout at each level. The engagement of decision makers at county and sub-county levels in the development of the roadmap was crucial in driving implementation forward. Integration of IMAM Surge into key strategic planning documents, including the Kenya National and County Nutrition Action Plans and County Integrated Development Plans, resulted in the allocation of resources and further strengthened government ownership and leadership by key decision-makers. Ownership of the approach has been clearly demonstrated at all levels of health service delivery and management (CHMT, SCHMT, health staff, CHVs, Health Facility Management Committee (HFMC)) and is one of the key drivers of the success of the approach.
Another important lesson was the effectiveness of OJT and ongoing mentoring to support IMAM Surge at health facility level. Classroom-based trainings were less effective, largely because it was not possible to use local data from the participants’ own facility and due to a lag time between training and actual set-up.
A final key to the success of the approach was the use of IMAM Surge dashboards at county level. This enabled the aggregation of child wasting admission data set against context-specific caseload thresholds to enable the rapid identification of deteriorating nutrition. This was critical for initiating early action and preventing the situation from worsening and the dashboards seem to have functioned at least as well as, if not better, than some standard early warning indicators used in Kenya. IMAM Surge, and particularly the dashboards, have clear potential to be leveraged further and linked more formally to wider early warning/early action mechanisms at county and national level.
Challenges
While IMAM Surge implementation has been largely successful in Kenya, some challenges have arisen that hinder full scale-up. Firstly, frequent drought episodes in the ASALs have affected scale-up plans. This has resulted in counties shifting focus to immediate drought response and away from longer-term health system strengthening approaches. It is essential that IMAM Surge set-up is prioritised before drought periods become acute.
Secondly, weak community-facility linkage in areas with non-functional community units (where CHVs are not actively involved in preventive activities or screening and referral) meant that a deteriorating nutrition situation could not be detected early at health facility level as children were not being referred or seeking treatment, resulting in low coverage of services. Strengthening of community units and linking them more firmly into the IMAM Surge process could help to trigger more effective active case finding and referrals of children with acute malnutrition. The national government recently released its Community Health Policy (2020-2030) and the county governments are at different stages of adopting legislation to support this.6
Lastly, resource constraints have affected the ability of health facilities to trigger IMAM Surge actions when a threshold is breached with Surge support largely coming from partners. The planning and costing of Surge actions should be further streamlined into sub-county/county planning and budgeting processes with a greater focus on the actual utilisation. Inclusion of Surge actions in the local government’s disaster risk financing mechanisms will ensure early action is not constrained.
What next for IMAM Surge in Kenya?
IMAM Surge is already an important approach for monitoring and responding to the nutrition situation in Kenya’s ASALs. The next steps are to further scale up the approach in the 10 counties and beyond with support from UNICEF and Concern. Integration of IMAM Surge processes, tools and outcomes into MoHK and sub-county/county mechanisms will further improve its relevance, effectiveness and sustainability. Another important next step is the linking of IMAM Surge dashboards with early warning systems. This is especially important in vulnerable counties such as Turkana. UNICEF is currently exploring possible linkages, particularly the linking of IMAM Surge with the National Drought Management Authority (NDMA).
Under the leadership of the MoHK, UNICEF and Concern in Kenya are already innovating and adapting the IMAM Surge approach to further improve its effectiveness. Moving forward, research and learning processes are crucial for supporting the future refinement, development and adaptation of the IMAM Surge approach in this country. In 2021, Concern will examine and document and barriers (including cost) across CMAM Surge programmes where thresholds have been exceeded but where surge was not triggered. Concern are also planning to trial two new IMAM Surge components in Kenya, including the expansion of the IMAM Surge approach to improve management of critical child illnesses alongside wasting management (Health Surge)7 and the use of facility-level IMAM Surge data to identify and trigger seasonal actions at community level to prevent spikes in wasting and related morbidities in critical months.
For more information, please contact Weldon Ngetich.
Subscribe freely to receive Field Exchange content to your mailbox or front door.
Endnotes
1 Global Conference on Primary Health Care (October 2018). Declaration of Astana.
2 HINI package: High-Impact Nutrition Interventions (HiNi) include: 1. Promotion of exclusive breastfeeding in the first six months of age, 2. Promotion of complementary feeding after six months of age, 3. Promotion of improved hygiene practices, 4. Vitamin A supplementation, 5. Zinc supplementation for diarrhoea management, 6. Deworming for children, 7. Iron-folic acid supplementation for pregnant women, 8. Iron fortification of staple foods, 9. Salt iodization, 10. Multiple Micronutrient Supplementation for children under five years, 11. Prevention or treatment of moderate acute undernutrition and 12. Prevention and treatment of severe acute malnutrition.
3 The Facilitators’ Guide provides step-by-step guidance on how to lead training participants through the IMAM Surge Guide and Toolkit. It provides a draft training agenda, guides the trainer on how to prepare for the training, provides a training methodology for all the IMAM surge steps.
4 Data from the IMAM Surge dashboard, MoH Kenya (June 2020)
5 Vegetation Condition Index (VCI) is a measure of the state of plant health relative to the same period during the previous year. It is expressed as a % and gives an idea where the observed value is situated between the extreme values (minimum and maximum) in the previous years. Lower values (dark red, red and yellow) indicate bad and good vegetation state conditions, respectively.
6 https://nurturing-care.org/kenya-community-health-policy-2020-2030
7 See article in this special section of Field Exchange entitled ‘CMAM Health Surge’
References
Collins, S. (2004). Community-based therapeutic care; A new paradigm for selective feeding in nutritional crises, Network Paper. https://odihpn.org/wp-content/uploads/2004/12/networkpaper048.pdf
Hailey, P. and Daniel, T. (2010). Suggested New Design Framework for CMAM Programming. Field Exchange 39, September 2010. p41. www.ennonline.net/fex/39/suggested
Lupao, K. and Mogusu, E. (2019). Scale up of high-impact nutrition interventions in the informal settlements of Nairobi, Kenya. Field Exchange 59, January 2019. p2. www.ennonline.net/fex/59/informalsettlementsnairobi
Ministry of Health Kenya (2019). Surge Approach for Integrated Management of Acute Malnutrition. https://www.alnap.org/system/files/content/resource/files/main/IMAM%20-Surge_operational%20guide_Near%20final.pdf
Ministry of Health of Kenya (2019). Refocusing on quality of care and increasing demand for services; Essential elements in attaining universal health coverage in Kenya. http://www.health.go.ke/wp-content/uploads/2019/01/UHC-QI-Policy-Brief.pdf
MoH Kenya (2018). IMAM Surge review report. September 2018
MoH Kenya (2019) IMAM Surge review workshop report. October 2019.
National Disaster Management Authority (NDMA) Kenya (2019). The 2019 Long Rains Season Assessment report. https://www.ndma.go.ke/index.php/resource-center/category/68-2019
Newton-Lewis, T. et al (2020). Working Paper: What is a shock responsive health system?. June 2020. Accessed at: https://reliefweb.int/sites/reliefweb.int/files/resources/MaintainsSRHS-ConceptualModel_08062020_GK.pdf