Use of educational videos to improve maternal breastfeeding knowledge and practices in Ethiopia
By Ritu Rana, Hatty Barthorp, Liya Assefa, Alemayhu Beri and Mary T Murphy
Ritu Rana is a GOAL Nutrition Research Advisor (Management of At-risk Mothers and Infants under six months (MAMI)). She has a PhD in nutrition (India), a second Master’s Degree in Nutrition for Global Health (UK) and nine years’ experience working in nutrition research.
Hatty Barthorp is a GOAL Global Nutrition Advisor. She has worked on emergency, transitional and development programmes for 18 years.
Liya Assefa is a Senior Nutrition Research Officer (MAMI). She has a Bachelor's Degree in Public Health, a Master's Degree in Project Management and is currently pursuing a Master’s Degree in Reproductive Health. She has around five years’ experience in nutrition and research.
Alemayhu Beri is a supervisor for MAMI and Senior Community Management of Acute Malnutrition (CMAM) Programme Officer at GOAL Ethiopia. He has around nine years’ experience in humanitarian programming.
Mary T Murphy is a Refugee Programme Manager at GOAL Ethiopia. She has over 20 years’ experience in nutrition and humanitarian programming.
The authors would like to thank the Global Health Media Project (GHMP) for supporting the translation and narration of selected GHMP videos in Nuer language and Nächstenliebe Weltweit for supporting the implementation.
Location: Ethiopia
What we know: The use of educational videos is emerging as an effective mode of health education including to support optimal infant and young child feeding.
What this article adds: GOAL has begun using breastfeeding educational videos within its Maternal, Infant and Young Child Feeding (MIYCF) and Management of ‘at risk’ Mothers and Infants (MAMI) programme in Gambella refugee camps in Ethiopia. Eight Global Health Media Project (GHMP) breastfeeding education videos were translated into the local language and shown to mothers with infants under six months of age attending MIYCF/MAMI clinics over the course of eight weeks between August and December 2020. Changes in maternal breastfeeding knowledge and practice were assessed to determine the feasibility of the approach through semi-structured interviews at baseline and endline and, at endline, through focus group discussions with mothers and key informant interviews with health workers. A total of 93 mothers were included in the study. At baseline, 100% of the mothers practiced breastfeeding and 92.5% practiced early initiation of breastfeeding (EIBF). At endline, analysis of primary outcomes demonstrated a statistically significant difference in knowledge about introduction to complementary feeding (increased by 8.7 percentage points) but no significant differences in other primary breastfeeding practice and knowledge outcomes. Analysis of secondary outcomes showed a substantial change in knowledge, including improvement in knowledge about the advantages of EIBF, attachment and positions during breastfeeding and signs to identify that the baby is hungry. Qualitative results showed that mothers and health workers found the videos acceptable, useful and effective. GOAL now plan to implement this video-assisted counselling in both MIYCF and MAMI programmes in the Gambella programme with increased frequency and on bigger screens. In addition, community health workers will show the videos on tablets to family members and key influencers to address wider barriers to optimal breastfeeding practices.
Background
Optimal breastfeeding practices are associated with reduced morbidity and mortality in young children (Sankar et al., 2015). For infants under six months, exclusive breastfeeding (EBF) is recommended by the World Health Organization (WHO) as the optimum diet. However, breastfeeding women may experience challenges to maintaining EBF for the first six months. A review documented various barriers to EBF in low- and middle-income countries (LMICs), including maternal perceptions of insufficient breastmilk, breastfeeding problems and lack of counselling (Kavle et al., 2017). These barriers are often not adequately addressed through infant and young child feeding (IYCF) counselling programmes.
GOAL has been implementing nutrition programmes, including maternal infant and young child feeding (MIYCF) and management of at-risk mothers and infants under six months (MAMI) in Kule and Tierkidi refugee camps in Gambella since 2014. As part of these support services, counselling on infant feeding is provided to mothers or caregivers. Currently, MIYCF counselling services are mainly didactic and include group education sessions using counselling cards while the MAMI service is focused on one-on-one counselling, predominantly using MAMI counselling cards.
The use of educational videos is emerging as an effective mode of health education (Tuong, Larsen & Armstrong, 2014). Studies from Uganda, Rwanda and Malaysia have shown that educational videos are effective in improving knowledge and practices around breastfeeding (Monoto & Alwi, 2018; Mukarubayiza & Gowan, 2019; Mutanda, Waiswa & Namutamba, 2016). Thus, to address the barriers faced by breastfeeding women during the first six months of a child’s life, GOAL has started using breastfeeding educational videos within its MIYCF and MAMI programme. To pilot the approach, GOAL translated eight Global Health Media Project (GHMP)1 breastfeeding educational videos to Nuer language, the local language of the South Sudanese refugees in Kule and Tierkidi camps. To document the learnings, this study was designed to assess the changes in maternal breastfeeding knowledge and practice and to determine the feasibility (acceptability and utility) of the videos.
Methods
Design and setting
We used an adequacy design with pre (baseline) and post (endline) assessments. From August to December 2020, GOAL piloted the GHMP breastfeeding educational video intervention in all four refugee camp sites – Kule 1, Kule 2, Tierkidi 1 and Tierkidi 2, Gambella, Ethiopia (Figure 1).
Figure 1: Study flow diagram
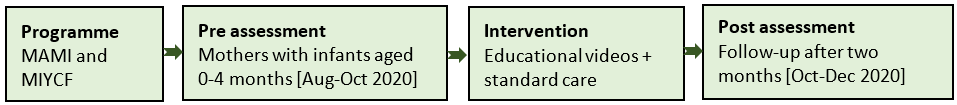
Study population and intervention delivery
The study population included mothers of infants under six months. At pre assessment, i.e., baseline, mothers with infants under four months residing in Kule and Tierkidi refugee camps who attended the MIYCF and/or MAMI programme and received breastfeeding counselling (based on MAMI and UNICEF IYCF counselling cards) were invited to participate in the study. Mothers were shown breastfeeding videos over a period of two months (eight weeks) (ENN et al., 2018; UNICEF, 2012). Thereafter, the same mothers were followed up for post assessment.
Using a multimedia platform (tablet), a total of eight videos of average length of seven to eight minutes were shown on a one-to-one basis. Subjects of the videos included i) attaching your baby at the breast, ii) positions for breastfeeding, iii) is your baby getting enough milk? iv) increasing your milk supply, v) how to express breastmilk, vi) storing breastmilk safely, vii) what to do about nipple pain, and viii) what to do about breast pain. Based on the mothers’ breastfeeding challenges or preference, counsellors decided on the sequence of the videos (most pertinent followed by others) and, if needed, the videos were repeated as required. Each participant was shown at least two videos at one contact point (weekly visit at MAMI/MIYCF programme clinic) and, over a period of eight weeks, the participants were shown all eight videos, repeated at least twice. Exposure to the intervention for participants was also recorded.
Sample size and data collection
Sample size was determined to assess the effect of the intervention over time using a comparison of paired proportions. We considered the following assumptions: 2% success-failure proportion, 45% failure-success proportion, 5% level of significance, 80% power and 20% non-response rate. We estimated that a total sample size of 96 (24 per camp site) was sufficient to compare paired proportions from baseline to endline. Data was collected at two time points – pre (baseline) and post (endline) assessments between August and December 2020. We used both quantitative and qualitative tools. A semi-structured tool, adapted from the WHO indicators for assessing IYCF practices (measurements), with questions on participant characteristics, breastfeeding knowledge and practices was administered to mothers at baseline and endline (WHO, 2010). Additionally, we also conducted focus group discussions (FGDs) with mothers (two FGDs/site, total eight) and key informant interviews (KIIs) with health workers – MIYCF/MAMI counsellors (two staff/site, total eight) at endline. Topics included in the FGD/KII guides are shown in Box 1.
Box 1: Topics for FGD/KII guides
- What do you think of the breastfeeding videos?
- What have you learnt from these videos/how do you find them as an educational tool?
- What do you like about the videos/what do you like about using the videos?
- Anything you did not like about the videos?
- How did you find this new method of IYCF support compared to how you were being supported before (mothers)/how did you find this new method of IYCF support compared to how you were supporting before (health workers)?
- After watching the videos, have you made any changes in the way you breastfeed the child (mothers)/after showing the videos, have you observed any changes in the mothers’ breastfeeding knowledge and practices (health workers)?
- What other support do you think would help you to maintain good breastfeeding practices (mothers)/what other support do you think would help you to provide adequate IYCF services (health workers)?
- Who influences feeding practices for babies and young children at home or in your community?
- Is there anyone else you think should be watching these videos in your community?
The health workers (counsellors, Diploma in General Nursing and Midwifery (DGNM)) interviewed the mothers while the research staff (Master of Public Health) conducted FGDs with the mothers and KIIs with the health workers. All data was collected using pen and paper.
Intervention delivery and data collection adaptation in the context of COVID-19
The tablets used for showing videos were sanitised with disinfectant after each use. For interviews, a minimum distance of one metre was maintained between the data collector and study participant. For FGDs, a maximum number of five participants was decided and the discussions were conducted in an open space, maintaining at least one metre distance between individuals (Figure 2).
Figure 2: Data collection adaptations to prevent COVID-19 infection

Left, FGD and right, KII
Data analysis and presentation
Data was first entered and cleaned in Microsoft Excel spreadsheets (pre-post sheet, FGD sheet and KII sheet). The sheet with pre-post data was imported in STATA and this data was analysed to calculate frequencies of participant characteristics and changes in proportions of breastfeeding knowledge and practice outcomes.
Five primary outcomes were defined: i) exclusive breastfeeding, ii) bottle feeding, iii) cup feeding, iv) knowledge of early initiation and v) knowledge of complementary feeding. Three secondary outcomes were also defined related to knowledge about: i) advantages of early initiation of breastfeeding (EIBF) (1: healthy start to the baby, 2: skin-to-skin contact, 3: colostrum, 4: suckling will speed up contraction of uterus and delivery of placenta and 5: help bond with the baby), ii) attachment and positions (1: hold baby close, towards mother, 2: head and body inline/straight, 3: nipple opposite nose, 4: fingers away from nipple, 5: mouth wide open, 6: chin against breast and 7: lip turned out) and iii) signs that baby is hungry (1: moving lips/tongue, 2: hand to mouth, 3: opening mouth; 4: turning head side to side and 5: crying/irritable/restless). Qualitative data was coded in Excel and themes identified. Results are presented according to themes.
Ethical considerations
We followed the ‘ethical standards for research during public health emergencies’ guidelines by WHO (WHO, 2020). We ensured that the research work did not impede the emergency response efforts and all participants were treated with equal respect. All data was collected after obtaining informed consent from the participants.
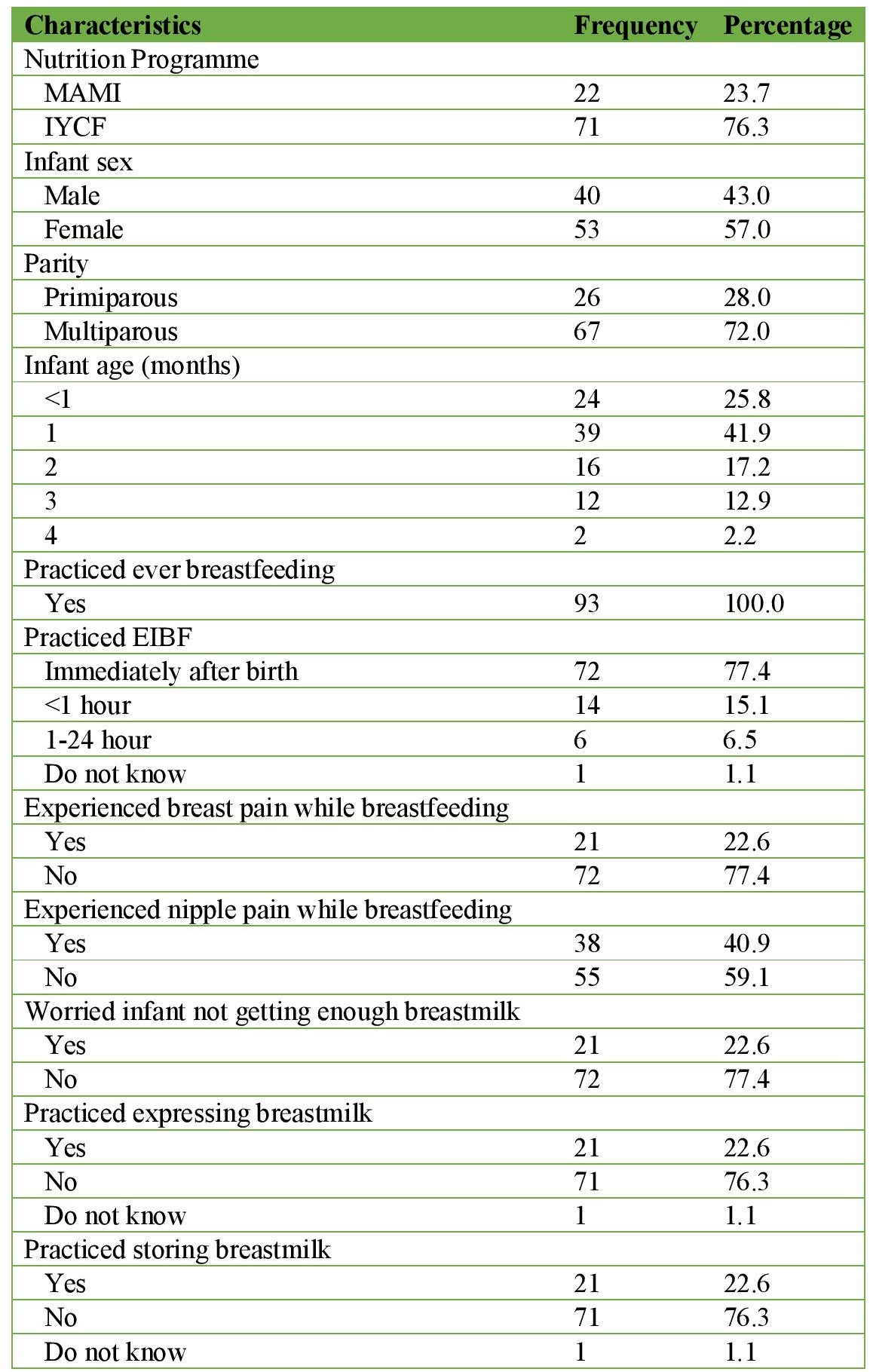
Results
Of the 96 participants, three did not complete the study (moved to host community) and hence the final analysis is based on 93 participants. Characteristics of participants at baseline are presented in Table 1. More than three-quarters of the mothers were attending the MIYCF programme. The majority (67.7%) had infants ≤1 month of age. All mothers practiced breastfeeding and the vast majority (92.5%) also practiced EIBF (immediately after birth to less than an hour). Just under a quarter of mothers practiced expressing and storing breastmilk and 22.6% of mothers were worried about their infant not getting enough milk. The proportion of mothers who experienced nipple pain specifically was 40.9% while 22.6% reported more generalised breast pain.
Table 1: Characteristics of study population at baseline
Effect of videos on maternal breastfeeding knowledge and practices
Each mother watched the eight videos at least twice. After watching the videos, analysis of the primary outcomes demonstrated a statistically significant difference in the knowledge about introduction to complementary feeding – increased by 8.7 percentage points (Table 2). However, no significant differences were observed in other primary breastfeeding practice and knowledge outcomes. It is important to note that, at baseline, all mothers were already practicing EBF and only a small proportion were practicing bottle or cup feeding using expressed breastmilk. Similarly, the vast majority of mothers at baseline already had correct knowledge about EIBF.
Table 2: Change in primary outcomes related to knowledge and practice
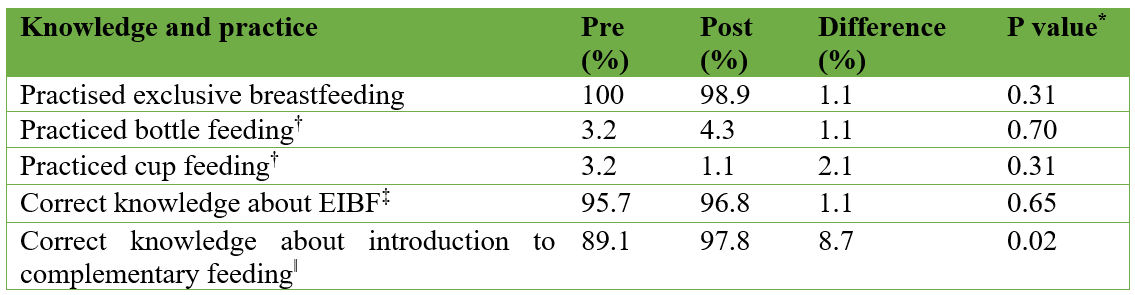
Figure 3 presents the changes in secondary outcomes related to mothers’ breastfeeding knowledge. Unlike the primary outcomes, these illustrate a substantial change in knowledge. Overall, there was an improvement in knowledge about the advantages of EIBF, attachment and positions during breastfeeding and signs to identify that baby is hungry. Before watching the videos, most mothers only knew about ‘a healthy start to the baby’ and ‘colostrum’ as advantages of EIBF. However, after watching the videos, they also knew about ‘skin-to-skin contact’ and ‘bonding with the baby’. Similarly, regarding attachment and positions, most mothers only knew about ‘holding baby close’ and ‘mouth wide open’ while, after watching the videos, they also knew about ‘head and body in line/straight’. Mothers’ knowledge about identifying signs that baby is hungry also improved – initially they could only identify ‘moving tongue/lips’ and ‘crying/irritable/restless’. After exposure to the intervention, they were also looking for signs such as ‘opening mouth’ and the baby putting ‘hand to mouth’.
Figure 3: Change in secondary outcomes related to breastfeeding knowledge
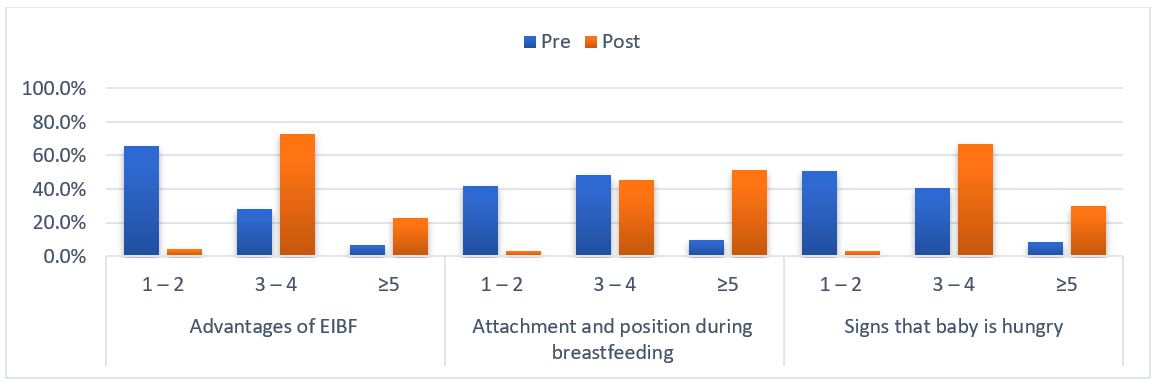
Numbers on x axis represent number of knowledge items
Feasibility of the videos
Five themes emerged from the qualitative findings: utility, appropriateness, acceptability, effectiveness, challenges and suggestions.
Utility
All mothers found the videos useful. Health workers also found them useful – they mentioned that mothers like watching the videos. One of the health workers highlighted that using only counselling it is difficult to demonstrate [“we don’t demonstrate everything because it’s hard to show our private body parts”]. Another health worker mentioned it could reduce their workload [“The counselling used to take us around 40 minutes. Now we can undertake other activities while they are watching the video”].
Appropriateness
Mothers stated they learnt about attachment and positioning, expressing and storing breastmilk, managing breast pain and identifying signs of baby getting enough milk. Health workers said they liked the length and pace of the videos. They also highlighted that the videos are comprehensive and self-explanatory and appreciated the local language translation.
Acceptability
When asked about likes or dislikes, both mothers and health workers said there was nothing that they did not like about the videos. Mothers shared various examples of what they liked about the videos such as – they can practice while watching the videos, they liked how real the videos are [“I came from rural area in South Sudan I did not know breastfeeding had to follow a certain way. The video elaborates that one by one. The mothers do not get humiliated when they show their breast, I like how real the videos are”], appreciated the videos are in their local language [“I like how it was done in our language”] and found them easy to follow and remember [“the videos are not playing fast, so, we can attentively follow”]. Similar to the mothers’ responses, health workers also mentioned that mothers can practice side by side while watching. One of the health workers said “The videos give time for the mothers to practice while watching the video. The mothers can follow the flow of the video and practice side by side. And the animators are humans which make the videos more acceptable”.
Effectiveness
Comparing the digital version of IYCF support with standard counselling support, mothers mentioned the advantages of the videos over standard support. Mothers said the videos were comprehensive and the practices are demonstrated while with standard counselling they only received messages thus must translate these into practical actions. They also highlighted that, when they watch the videos, it is easier to remember messages while with standard counselling they sometimes forget. On the other side of the fence, health workers said that convincing mothers to participate in counselling requires effort. However, with videos, they are happy to focus on behaviour change. One of the health workers said – “counselling takes more time and sometimes beneficiaries get bored, however, with videos they are happy to learn”. Mothers said after watching the videos, they had started practicing expressing and storing breastmilk, observing signs that baby is getting enough milk and observing attachment to nipple. Health workers confirmed these changes in practices. The most commonly cited reasons for practising expressing and storing breastmilk were mothers’ other household responsibilities, such as going to market and fetching firewood. One of the mothers said – “I learnt how to express the milk from my breast. This is a new thing. We have so many responsibilities as a woman. Knowing this method has helped me reducing my burden”.
Challenges
Acceptance of expressing and storing breastmilk was found to be a challenge by the community. Some mothers said their family members do not support them as they find these practices to be against their culture and religion. Mothers said that elderly people in the family influence their feeding practices; a mother shared, “the influence is high from our fathers and mothers. They want to raise our children the way we grew up. They refuse us to practice some of the practices we learn here. For example: removing the milk from the breast is not accepted well by the community”.
Suggestions
Mothers suggested these videos should also be shown to young girls, pregnant women and one additional caregiver (husband). Mothers mentioned similar videos can be prepared for pregnant women while health workers suggested continuing such videos beyond the first six months of life. Other suggestions included a request for increasing the frequency and a bigger screen for watching the videos.
Discussion
This study found that the majority of the mothers were already practicing exclusive breastfeeding before exposure to the intervention, however, their knowledge about the various advantages of early initiation of breastfeeding, attachment and positioning, and identifying signs that baby is hungry was limited. Post exposure, after watching the videos, exclusive breastfeeding was sustained and there were considerable improvements in more detailed breastfeeding knowledge. Both mothers and health workers found the videos acceptable, useful and effective. Other benefits recorded were improved ability of the videos to convey ideas and physically demonstrate specific practices that not usually achieved through didactic counselling, allowing mothers to trial various practices whilst being shown them, improving engagement and memory retention by mothers/carers and providing a marked reduction in workload for health workers.
Although EIBF and EBF are two core IYCF indicators and are most commonly measured to assess the IYCF practices for infants under six months, other qualitative indicators, such as attachment and positioning, are also important. Effective breastfeeding is a function of both the correct positioning of mother and baby and the correct attachment of the child to the mother's breast. It is essential to support early growth and development as it is associated with long-term health.
The GHMP breastfeeding videos have also been tested in other settings. A study from Malaysia found these videos to be a suitable educational and training tool in helping breastfeeding mothers (Monoto & Alwi, 2018). Another study from Rwanda found the GHMP videos were effective in improving parental knowledge in caring for their pre-term infant (Mukarubayiza & Gowan, 2019). Other studies have also found that video-assisted counselling is effective in sustaining healthcare behaviors (Kellams et al., 2016; Aditya, Tiwari & Mishra, 2020). Baseline EBF rates were not assessed in these studies however.
Due to the COVID-19 pandemic, we used an adequacy evaluation design with longitudinal data collection. As there was no control group, it may be difficult to infer any observed changes were due to the intervention and that these changes would not have happened anyway. The observed changes may have been caused by other factors such as women can become more knowledgeable about breastfeeding as they continue their breastfeeding journey – i.e., as their infant grows and they overcome various challenges.
The data we collected was brief and investigations were not as detailed as would have been planned under normal circumstances. To save health workers’ time, who were overburdened, we only collected post-assessment information on selected indicators. The FGDs and KIIs were also minimised to be completed under 20-30 minutes and 10-15 minutes, respectively. The study results should be interpreted in line with these limitations. Since our study population at baseline was already practicing EBF, it would be interesting to conduct a similar study in a population where breastfeeding practices are not as optimal at baseline and compare the results.
We plan to implement this video-assisted counselling in both MIYCF and MAMI programmes in Gambella, Ethiopia. However, as suggested by mothers and health workers, we would consider increasing the frequency and introducing bigger screens – displaying videos on a television so that the mothers can watch them together, practice side by side and discuss with or support each other. Through video-assisted counselling, we would also be addressing the challenges faced by the mothers due to local traditions, elaborating on when these practices can be used to maximise positive outcomes for the infant. In addition to displaying breastfeeding videos on bigger screens as part of clinic-based counselling services, we also plan for the community health workers to use tablets to show the videos to family members or key influencers to address any challenges faced by the mothers due to cultural or religious belief.
For more information, please contact Hatty Barthorp at hbarthorp@goal.ie
1 https://globalhealthmedia.org/
References
Aditya, V, Tiwari H C and Mishra R (2020) A study on effectiveness of video assisted counselling in establishing and sustaining appropriate breast feeding practices, Journal of Family Medicine and Primary Care, 9: 4680.
ENN, GOAL, LSHTM and Save the Children (2018) C-MAMI Tool, Version 2 (2018)', Emergency Nutrition Network (ENN), Accessed 27 February 2021. https://www.ennonline.net/c-mami.
Kavle, J A, LaCroix E, Dau H and Engmann, C (2017) Addressing barriers to exclusive breast-feeding in low-and middle-income countries: a systematic review and programmatic implications, Public Health Nutrition, 20: pp. 3120-34.
Kellams, A L, Kelly, K G, Hornsby, P P, Drake, E, Riffon, M, Gellerson, D, Gulati, G and Coleman V (2016) The impact of a prenatal education video on rates of breastfeeding initiation and exclusivity during the newborn hospital stay in a low-income population, Journal of Human Lactation, 32: pp. 152-59.
Monoto, E M M and Alwi, N K M (2018) Breastfeeding videos as a new training tool for Malaysian breastfeeding peer counsellor program in empowering breastfeeding communities, IIUM Medical Journal Malaysia, 17.
Mukarubayiza, M R and Gowan, M (2019) Educational intervention to increase parental care of preterm neonates at district hospital in Kigali, Rwanda Journal of Medicine and Health Sciences, 2: pp. 105-11.
Mutanda, J N, Waiswa, P and Namutamba, S (2016) Community-made mobile videos as a mechanism for maternal, newborn and child health education in rural Uganda; a qualitative evaluation, African health sciences, 16: pp. 923-28.
Sankar, M J, Bireshwar, S, Chowdhury, R, Bhandari, N, Taneja, S, Martines, J and Bahl, R (2015) Optimal breastfeeding practices and infant and child mortality: a systematic review and meta-analysis, Acta paediatrica, 104: pp. 3-13.
Tuong, W, Larsen E R and Armstrong A W (2014) Videos to influence: a systematic review of effectiveness of video-based education in modifying health behaviors, Journal of behavioral medicine, 37: pp. 218-33.
UNICEF (2012) Infant and Young Child Feeding: Counselling Cards for Community Workers, Accessed 27 February 2021. https://sites.unicef.org/nutrition/files/counseling_cards_Oct._2012small.pdf.
WHO ( 2010) Indicators for assessing infant and young child feeding practices: part 2: measurement.
WHO (2020) Ethical standards for research during public health emergencies: Distilling existing guidance to support COVID-19 R&D Geneva: WHO, 2020.