Early lessons from Swabhimaan, a multi-sector integrated health and nutrition programme for women and girls in India
By Monica Shrivastav, Abhishek Saraswat, Neha Abraham, R.S. Reshmi, Sarita Anand, Apolenarius Purty, Rika Shalima Xaxa, Jagjit Minj, Babita Mohapatra and Vani Sethi
Monica Shrivastav is a consultant with the UNICEF supported ROSHNI-Centre of Women Collectives led Social Action, Lady Irwin College, New Delhi, India, supporting evidence generation and technical assistance to the National Rural Livelihoods Mission, Ministry of Rural Development.
Dr. Abhishek Saraswat is a demographer, currently affiliated with the International Institute for Population Sciences, Mumbai, India, working as a data analyst for the Swabhimaan project.
Neha Abraham is a Knowledge Management Consultant at the ROSHNI-Centre of Women Collectives led Social Action.
Dr. R.S. Reshmi is an Assistant Professor at the Department of Migration and Urban Studies at the International Institute for Population Sciences, Mumbai and is the coordinator of the Swabhimaan project.
Dr. Sarita Anand is an Associate Professor at the Department of Development Communication and Extension, Lady Irwin College and is Centre Lead for the ROSHNI-Centre of Women Collectives led Social Action.
Apolenarius Purty is State Programme Manager, Health and Nutrition, Bihar Rural Livelihoods Promotion Society (JEEViKA), Government of Bihar, Patna, India.
Rika Shalima Xaxa is the State Programme Manager - Social Inclusion and Social Development at Chhattisgarh State Rural Livelihoods Mission ‘BIHAN’, under the Department of Panchayat and Rural Development, Raipur, Chhattisgarh, India
Jagjit Minj is Programme Executive of the Social Inclusion and Social Development at Chhattisgarh State Rural Livelihoods Mission ‘BIHAN’, under the Department of Panchayat and Rural Development, Raipur, Chhattisgarh, India
Dr. Babita Mahapatra is the Additional Chief Executive Officer at the Odisha Livelihoods Mission (OLM) under the Panchayati Raj and Drinking Water Department of Government of Odisha.
Dr. Vani Sethi is a Nutrition Specialist at the Nutrition Division of UNICEF India, working on advancing adolescent and women’s nutrition through Ministry of Health and Family Welfare and the National Rural Livelihoods Mission platforms.
The authors acknowledge the support of Deendayal Antyodaya Yojana-National Rural Livelihoods Mission (DAY-NRLM), DAY-NRLM’s women collectives’ leaders and representatives from Kasba, Jalalgarh, Bastar, Koraput Sadar and Pallahara Blocks, the State Rural Livelihoods Missions of Bihar, Chhattisgarh and Odisha and the UNICEF State Office Bihar, Chhattisgarh and Odisha.
The impact evaluation partner for this work is the International Institute of Population Sciences, Mumbai, India. The authors also acknowledge the contribution of the Swabhimaan consortium: Rabi N Parhi, Sandip Ghosh and Parimal Chandra (Nutrition Section, UNICEF Bihar, Patna, India), Mahendra Prajapati (Nutrition Section, UNICEF Chhattisgarh, Raipur, India), Bharati Sahu (ROSHNI-CWCSA, New Delhi, India), Sourav Bhattacharjee, Sonali Sinha (Nutrition Section, UNICEF Odisha, Bhubaneshwar, India), Sayeed Unisa (International Institute for Population Sciences, Mumbai, India) Arjan De Wagt (Child Development and Nutrition, UNICEF India, New Delhi, India)
Location: India
What we know: Poor nutrition status before and during pregnancy is a serious problem in India and a key driver of low birth weight and child undernutrition.
What this article adds: Swabhimaan is a five-year initiative (2016-2021) integrated within the Government of India’s flagship poverty alleviation programme, Deendayal Antyodaya Yojana-National Rural Livelihoods Mission (DAY-NRLM), across three states in India, carried out in partnership with UNICEF. The programme aims to mobilise women via village-level women’s collectives to develop and implement integrated nutrition microplans and strengthen local government services in order to improve the nutrition outcomes of women and adolescent girls. The results are presented of a midline evaluation carried out in 2018-2019 covering villages in five different sites across the three states (including 3,171 adolescent girls, 1,856 pregnant women and 3,277 mothers of children under two years of age). The results reveal strong progress in implementation with 336 village-level microplans developed, 77,000 females screened and 15,122 identified as being at nutritional risk and referred for nutrition, agriculture and social protection support. Midline results show a reduction in thinness in adolescent girls (13.8% versus 18.5% at baseline) and mothers with children under two years of age (44.6% versus 48.4% at baseline) and an increase in the average mid-upper arm circumference of pregnant women (24.0cm versus 23.5cm at baseline). Evidence also shows improved household food security and improved uptake of government health, water, sanitation and hygiene and social protection services. Results suggest that utilising and funding women’s collectives to respond to nutrition needs in their communities with integrated responses are feasible. The results of the endline evaluation and an impact evaluation will be forthcoming.
Background
The poor nutritional status of a woman before and during pregnancy is a major cause of foetal stunting and low birth weight (LBW). In India, stunting affects around 47 million (38%) children aged under five years (NFHS-4, 2015–16). An estimated five million Indian children (19%) are born with LBW, around 4.4 million of whom are born small for gestational age (NFHS-4, 2015-16). Most Indian women enter pregnancy with poor nutrition – 23% of women of reproductive age are too thin for their height (body mass index (BMI) less than 18.5 kg/m2) and 53 % of women are anaemic (increasing to 58% among pregnant women). Additionally, 8% of pregnant women (around 4.5 million) are adolescents (NFHS-4, 2015–2016). Despite national and state level policies and programmes to deliver maternal care services in India, high quality coverage remains low.
The Indian Government’s flagship poverty alleviation programme, Deendayal Antyodaya Yojana-National Rural Livelihoods Mission (DAY-NRLM), implemented under the Ministry of Rural Development, aims to break the intergenerational cycle of poverty through the economic empowerment of vulnerable women and families. DAY-NRLM’s women’s collectives provide an opportunity to strengthen the delivery and promotion of women’s nutrition services at community-level, linking livelihood promotion, women’s nutrition promotion and women’s empowerment, and harnessing the ability of women to plan and implement context-specific programme activities. A 2016 scoping study suggested that DAY-NRLM village organisations have the potential to manage grants for improving the last mile delivery of essential nutrition services for women provided they are enabled, supervised and incentivised (Sethi et al, 2017).
On the basis of these findings, Swabhimaan was set up as a five-year initiative launched in 2016 by DAY-NRLM in partnership with UNICEF India across three states in India (Bihar, Chhattisgarh and Odisha). The programme aims to improve the nutrition outcomes of women and adolescent girls using DAY-NRLM women’s collectives as the key mode of delivery focusing on four primary target groups: adolescent girls, newlywed women, pregnant women and mothers of children under two years of age (secondary target groups include husbands, mothers-in-law and farmer producer groups). Community-led actions are delivered by DAY-NRLM. Systems strengthening activities also take place in convergence with four government departments to increase access to government services: the Department of Women and Child Development to increase the reach and quality of Integrated Child Development Services (ICDS), the Department of Health and Family Welfare for Village Health, Sanitation and Nutrition Days (VHSND), the Department of Water and Sanitation to improve water quality and achieve open defecation free villages and the Department of Food and Civil Supplies to increase the coverage of food subsidy schemes. The programme is funded by UNICEF India in Bihar, which serves as a demonstration and learning site, while the programme is led by the State Rural Livelihoods Mission (SRLM) in Chhattisgarh and Odisha with UNICEF providing a portion of the support costs. Built into this programme are baseline, midline and endline studies. The results of the midline study are presented here to help to fill the evidence gap on maternal nutrition interventions delivered via women’s collectives in India.
Intervention
Swabhimaan provides a comprehensive package of 18 nutrition-specific and nutrition-sensitive interventions spanning the health, nutrition, agriculture and livelihoods sectors targeted at women at preconception, during pregnancy and after birth (Table 1). These interventions are delivered through a combination of community-led and systems strengthening actions (Table 2).
Table 1: Swabhimaan package of nutrition-specific and nutrition-sensitive interventions
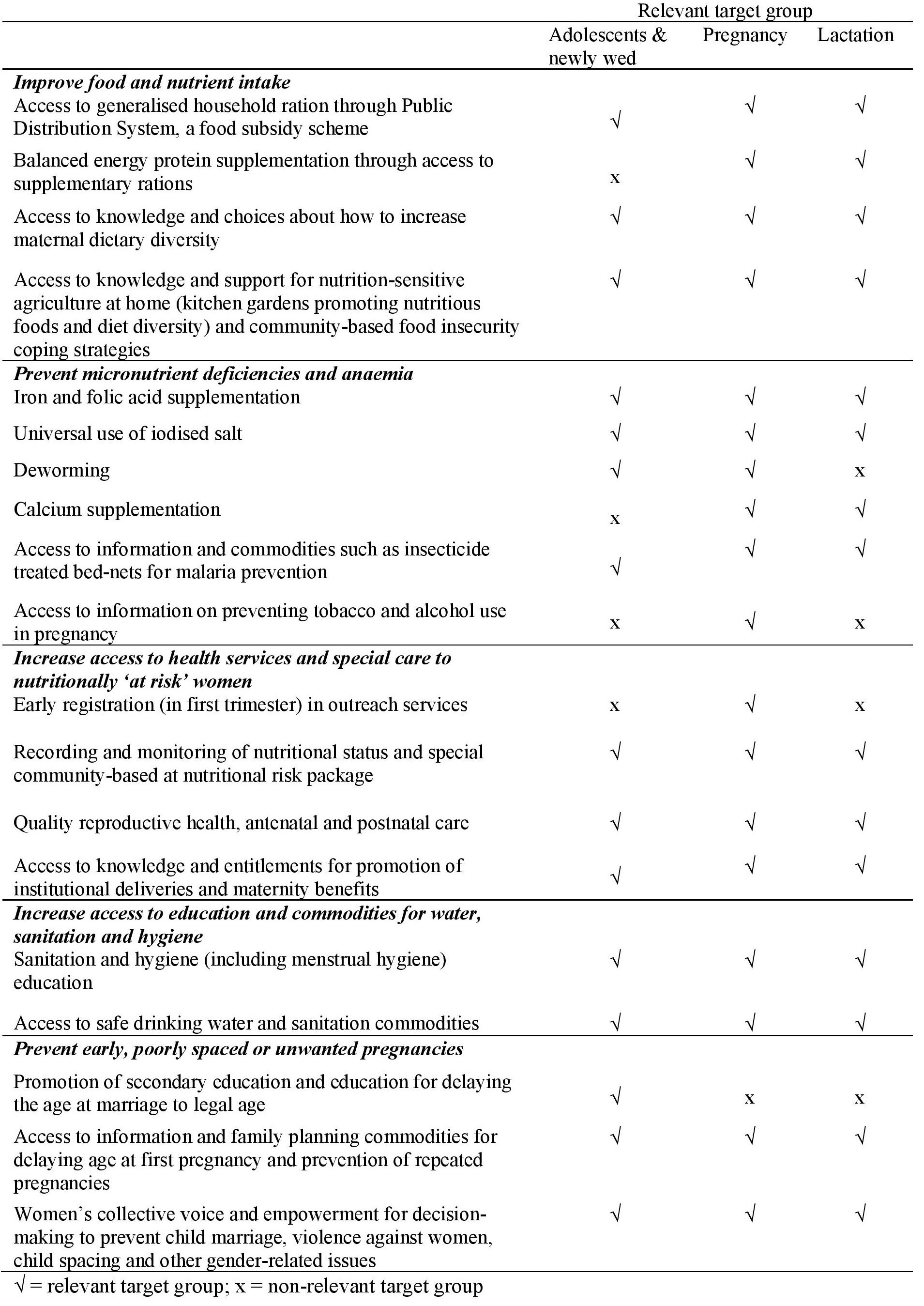
Table 2: Community-led and systems strengthening actions under Swabhimaan
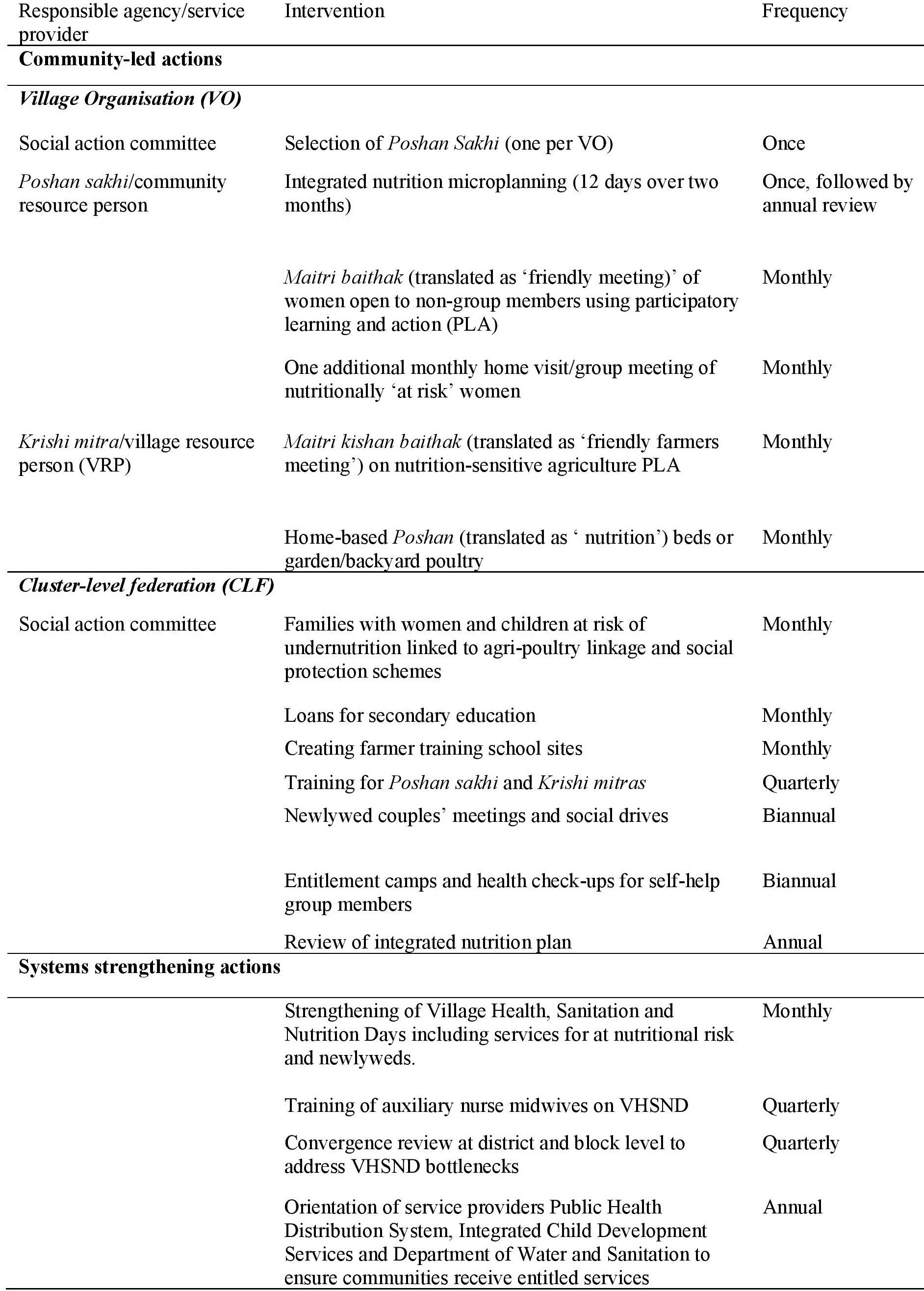
For the delivery of community-led actions, communities are engaged to customise a maternal nutrition delivery package responsive to local needs and to manage grants to implement the interventions. The community comes together under women’s collectives promoted under DAY-NRLM made up of female representatives from self-help groups (SHGs) and their federations (Village Organisations (VOs) and Cluster Level Federations (CLFs)). Each federation develops an integrated nutrition microplan that identifies and prioritises nutrition and related problems among target groups in their village/s, an annual plan of activities and a budget. These budgets are collated at block level, reviewed and approved by DAY-NRLM and submitted to the SRLM, an autonomous body under the state government, which then provides the annual grant to each VO accordingly.
The development of nutrition microplans is facilitated by a social action committee (SAC) for each VO. The SAC nominates an active SHG member to be the Community Resource Person (CRP). Women are eligible for nomination who are literate, effective communicators and who have graduated out of poverty. CRPs, known locally as Poshan Sakhis and Kishori Sakhis, undergo three days of pre-service training on integrated nutrition microplanning, the use of mid-upper arm circumference (MUAC) tapes and measurements for screening nutritionally ‘at risk’ adolescent girls and women (MUAC <19 cm and <23 cm, respectively) (Bulliyyag, 2007; Tang, 2013) and participatory learning and action (PLA) techniques to facilitate monthly meetings for women and adolescent girls. Following their training, CRPs facilitate the development of integrated nutrition microplans, supervised by the SRLM, and also provide home-based counselling for target groups, food demonstrations and support for the development of household nutrition gardens (gardens growing fruits and vegetables for household consumption).
The CRPs receive INR450 (USD$7) to develop an integrated nutrition microplan and thereafter a similar monthly incentive for facilitating the implementation of planned activities. CLFs receive grants including INR500 (~USD$7) for meetings with newlywed couples, INR500 (~USD$7) for each ‘welcome kit’ given to newlywed couples with essential items (iron-folic acid (IFA) supplements, contraceptives, sanitary napkins), INR1500 (~USD$22) to review each VO’s integrated nutrition microplan and INR5000 (~USD$77) to develop farmer training school sites. Community-led interventions are monitored through the collation and analysis of monthly reports submitted by CRPs for each VO that are then reviewed by CLFs and block-level supervisors.
The system strengthening interventions include quarterly training of government accredited social health activists (ASHA) and auxiliary nurse midwives (ANM) to strengthen the delivery of the fixed monthly health camps (VHSND) for the provision of antenatal care (ANC) check-ups, counselling, micronutrient supplementation, take-home rations under the supplementary nutrition programme, immunisation, weight monitoring, family planning and the identification and care of groups at nutritional risk. Training is also provided to strengthen Adolescent Health Days to improve access to adolescent health and nutrition services. In addition, health service providers (ASHA, ANM, Anganwadi workers (AWW) and lady supervisors of ICDS and the Public Distribution System (PDS) fair price shop owners are regularly engaged with to improve the delivery of the service package and entitlements. Regular review and convergence meetings are conducted with the departments involved in service delivery. Reporting on system strengthening is activity-based (monthly for VHSNDs and biannually for trainings/refresher trainings) and overall programme reports are reviewed annually by the national government.
Evaluation methodology
To test the delivery and impact of the Swabhimaan programme, baseline, midline and endline cross-sectional surveys were undertaken between 2016 and 2021 in three selected Indian states covering villages across five different sites. The baseline survey was conducted between October 2016 and January 2017 and included 6,352 adolescent girls, 2,573 pregnant women and 8,755 mothers of children under two years of age. The midline survey was conducted between September 2018 and June 2019 with 3,171 adolescent girls, 1,856 pregnant women and 3,277 mothers of children under two years. The endline survey will be conducted in 2021. Sample size calculations were conducted for each state that accounted for a 5% refusal rate and a design effect of 1.5. Respondents were recruited using a simple random sampling technique.
A standardised, bilingual quantitative questionnaire (in English and the local language) was administered to all target groups. Information obtained from the surveys included sociodemographic and household characteristics, educational attainment, diet diversity, household food security, the availability of a homestead kitchen garden and access to health, ICDS and SRLM services and decision-making practices. Anthropometric measurements (weight, height and MUAC) were taken using standard techniques. Quantitative data collected was entered using the Census and Survey Processing System and analysed using STATA 15.1. A midline process evaluation was also undertaken using a mixed-method approach comprised of a cross-sectional survey and qualitative data collection. The impact evaluation has been registered with the Registry for International Development Impact Evaluations (RIDIE-STUDY-ID-58261b2f46876) and the Indian Council of Medical Research National Clinical Trials Registry of India (CTRI/2016/11/007482). The impact evaluation’s endline survey and programme evaluation of Swabhimaan will be conducted in 2021.
Results
Progress of implementation
Programme monitoring of Swabhimaan shows all 336 VOs across the three states developed integrated nutrition microplans that identified community priorities and actions. By the end of 2019, VOs had screened over 77,000 adolescent girls, pregnant women, mothers of children under two years of age and newlywed women using MUAC, identifying nearly 15,122 individuals at nutritional risk for customised counselling, home visits, food demonstrations, the development of a nutrition garden or backyard poultry and, for some, links with government social protection schemes. By the end of 2019, CRPs had facilitated a total of 37,079 monthly meetings (maitri baithaks) across the intervention areas. Newlyweds had been oriented to maternal health issues in special biannual camps, provided with ‘welcome kits’ (contraceptives, IFA, sanitary pads, soap), inducted into SHGs and were mobilised to attend maitri baithaks. Over 1,000 adolescent groups have also been formed and are currently active across the three states.
VOs and CLFs have successfully collaborated with agriculture universities/training centres to design nutrition-sensitive farms and backyard gardens. Households with target individuals at nutritional risk have been prioritised to develop nutrition gardens in backyards and/or initiate poultry activities through small loans provide by the SHGs. By the end of 2019, over 5,000 nutrition gardens had been developed across the three states.
Swabhimaan has also successfully strengthened the supply side of health services by supporting a change in government policy that means that women are now screened for nutritional risk within VHSNDs, with those identified as being at risk then linked to the appropriate services. This has led to a significant increase in the participation of target groups in VHSND from 29.5% across the three states at the start of the programme to 85% by 2019.
Changes in maternal and adolescent health and nutrition outcomes and practices
Table 3 presents comparison results between the baseline and midline evaluations. Pre-intervention, the proportion of thin adolescent girls (BMI <-2SD) was 18.5% which reduced significantly to 13.8% (p<0.001) in 2019 after programme implementation. The proportion of thin mothers of children under two years (BMI <18.5 kg/m2) was 48.4% in 2016-17 (compared to the national average of 23%) and, by 2019, the proportion of thin mothers reduced to 44.6%. The mean MUAC among pregnant women was 23.5cm which increased to 24.0cm by 2019. Severe thinness among mothers of children under two years of age was 7.0% in 2016 which reduced to 6.5% by 2019 (Government of India cut-off for thinness in adults is <23 cm) (IIPS,2016a; IIPS,2016b; IIPS 2016c; Ministry of Health and Family Welfare, 2017).
In comparison to the baseline, a higher proportion of pregnant women (baseline 43.5%, midline 51.5%) and mothers (baseline 37.0%, midline 52.1%) achieved minimum dietary diversity scores than adolescent girls (baseline 41.3%, midline 48.0%) (p<0.001). At midline, all target groups showed significant improvement in IFA compliance as compared to baseline. The highest improvement was recorded among adolescent girls whose IFA consumption increased by 25.5% (p<0.001). At midline, a 5% increment in IFA compliance was registered among pregnant women and mothers, however, the overall consumption still remains low at 29.4% and 23.2%, respectively (p<0.001).
Data shows an 8-12% improvement in the proportion of women living in food secure households (p<0.001) from baseline to midline, however over 60% of women still lived in food insecure households. By midline, 71.9% of mothers’ households had access to PDS entitlement as compared to only 60.7% at the baseline (p<0.001). At midline, about 40-43% of the target groups’ households had improved toilets, with a 27%, 24% and 19% increase in adolescent girls’, pregnant women’s and mothers’ households having an improved toilet (p<0.001). At baseline, only 31.6% of the adolescent girls used sanitary pads which had significantly increased to 57.3% (p<0.001) by the midline.
At midline, 51.2% of pregnant women and 34.1% of mothers had received an ANC in the first trimester and at least four ANCs in their last pregnancy respectively which corresponds to a 16-17% (p<0.001) improvement as compared to the baseline. The proportion of pregnant women who had their weight monitored during their current pregnancy (baseline 66.0%, midline 86.2%) and mothers whose weight was monitored at least four times during the last pregnancy (baseline 24.1%, midline 29.4%) increased (p<0.001). Pregnant women and mothers who received one dose of albendazole in their second trimester increased by 8-11% (p<0.001) by the midline. A drastic improvement was recorded in the proportion of mothers (baseline 29.7%, midline 60.4%) and pregnant women (baseline 23.8%, midline 55.4%) who took calcium tablets in their second trimester (p<0.001).
The use of modern family planning methods among women was extremely low at baseline (pregnant women 7.1%, mothers 16.3%). However, modest improvements were recorded in the use of modern family planning methods by both pregnant women and mothers (4-6%, p<0.001) at midline. A slightly higher proportion of mothers attended at least three VHSNDs by midline (26.7%, p<0.05) than at baseline (24.4%). ICDS entitlements were better utilised and significant improvements were recorded in the utilisation of ICDS services by pregnant women (baseline 34.7%, midline 55.8%) and mothers (baseline 44.5%, midline 77.0%) (p<0.001). Mothers who opted for institutional delivery increased from 73.3% in 2016 to 76.4% by the baseline (p<0.001).
Midline qualitative results revealed that CRPs (Poshan Sakhis) conducted regular meetings, counselling and follow-ups with the target groups. Responses suggested that adolescent girls and pregnant women have adopted appropriate behaviours related to dietary intake and Water, sanitation and hygiene (WASH) practices and have increased the number of visits to health service points, such as Anganwadi Centres and VHSNDs, to access health and nutrition services. CRPs observed an increased awareness about the entitlements and services available and a visible change in the practice and knowledge of the community on food and WASH behaviours. They also shared their experience of improved coordination with health service providers (AWW, ASHA and ANM) which supported access to services by the target groups. However, they reported challenges in mobilising target groups regularly for meetings and observed gender-related issues in the target groups, such as women eating least and last, a skewed division of labour in the household, domestic violence and low decision-making power as barriers to ensuring improved health and nutrition outcomes of women and girls.
Table 3: Coverage of health and nutrition services for adolescent girls, pregnant women and mothers of children under two in intervention areas in Swabhimaan in baseline (2016-17) and midline (2018-19) surveys
Lessons learned for scale up
The results between the baseline and midline evaluations indicate improvement in the coverage of health and nutrition services among all target groups in the intervention areas including adolescent girls, pregnant women and mothers of children under two years of age across the three states of Bihar, Chhattisgarh and Odisha. The results also demonstrate statistically significant improvement in dietary diversity scores in all target groups, BMI in adolescents and mothers of children under two years of age and some improvement (although not statistically significant) in MUAC scores in pregnant women. Access to maternal nutrition services have also improved, although uptake remains low for some services including IFA supplementation for pregnant women and mothers, attendance at a minimum of four ANC sessions and the participation of mothers in VHSNDs. Access to toilets still remains low with over half of the participants still not having access to a toilet despite focused programmes implemented by the Department of Water and Sanitation.
Lessons from programme implementation provide evidence that VOs and CLFs can develop microplans and manage grants to strengthen the provision of a maternal nutrition service package for women and girls at nutritional risk in underserved areas. This is a shift from the earlier approach of last mile delivery of health services being a voluntary task that required much investment from the health volunteers themselves. Early results also show that CRPs can successfully mobilise women and adolescent girls and organise monthly discussions on priority nutrition issues using a PLA approach despite societal resistance and challenges in mobilisation. The microplanning process is a critical initiator of collective thinking, consensus on nutrition problems and resolute action. The context where Swabhimaan operates is marked by stark social and gender inequities (Reshmi, 2019). CRPs have been able to overcome these resistances and have made women’s health important for the communities through regular monthly meetings. VOs and CLFs are also able to collaborate with agriculture universities/training centres to design nutrition-sensitive farms and backyard gardens and enable access to grants to facilitate this. VO and CLF activities under Swabhimaan can be scaled up at INR90000 (~USD$13,000) in a resource block. The initiative in the three states has resulted in the creation of learning and implementation resources and trained CRPs and VRPs, such that the scale-up cost is mainly funding the training of new CRPs/VRPs and incentives for service delivery. Gradually, it is possible to build these costs into the annual plans of the SRLMs.
In addition to community-led activities, nutrition outcomes are dependent on the availability and access to timely health and nutrition services. This requires effective interventions that target supplies. The second strategy of this programme focuses on systems strengthening, supported by technical assistance from the UNICEF State Offices of Bihar, Chhattisgarh and Odisha. The coordination of government departments is critical to ensure that essential women’s nutrition interventions are available. Convergence under the POSHAN Abhiyaan promotes coordinated, multi-sector efforts involving all line departments that contribute towards nutrition such as health and family welfare, water and sanitation and rural development. This is possible through the joint planning and review of activities and quarterly convergence meetings at block and district level are used as a platform to undertake this. This is critical as this process enables the regular review of nutrition indicators based on the village microplans with all the line departments supporting in addressing implementation gaps in service delivery. To improve the quality and reach of health and nutrition services of Health and ICDS departments, the Swabhimaan programme facilitated the revision of the VHSND guidelines and integrated maternal calcium supplementation, deworming and the screening of women at nutritional risk using maternal MUAC into the guidelines for all three states (Bihar, Chhattisgarh and Odisha). It also expanded the target base by including newlywed and adolescent girls in the target group. The training of service providers on the revised VHSND guidelines at state, district and block levels ensured quality implementation. This effective integration of a systems strengthening intervention, which includes regular follow-up, review and monitoring, and the training of service providers for improvement of service delivery led to improvements on the supply side.
Limitations and challenges
As in most programmes that operate in real settings, systemic challenges exist. These are related to delays in the flow of funds for government schemes on which the delivery of maternal nutrition services hinge, delays in the procurement and/or distribution of supplies (medicines/supplements and rations) and health worker strikes. Secondly, the SHG-VO-CLF platform has varying maturity and stability across and within states, with some groups well established while some are fairly new. Consequently, the pace of implementation is non-uniform. In order to reduce this bias, Swabhimaan has retained the originally identified collectives (SHG-VO-CLF) in the research despite the emergence of newer collectives in its implementation sites. As new collectives are mobilised at the same implementation sites, they will also be included in the programme with the support of the existing structure. Furthermore, as these are essentially savings groups, layering on nutrition interventions is a slow and cautious process. DAY-NRLM has mentors in its operational structure to provide handholding support on the thrift and credit activities who could also be trained in programme planning and grant management for the provision of the maternal nutrition service package. Regular handholding and supervision support to the CLFs and VOs is critical to ensure their activities are nutrition-sensitive and responsive. These community institutions can be strengthened and capacitated through investments in integrated training and capacity-building to respond to the health and nutrition needs of the community.
Way forward
DAY-NRLM, in partnership with UNICEF, will scale up Swabhimaan’s maternal nutrition approach through NRLM platforms in alignment with its POSHAN Abhiyaan mandate. The nested impact evaluation showed promising results, informing the SRLMs of the three states to initiate scale-up with the horizontal expansion of these interventions while retaining the impact evaluation sites and protecting them from contamination until the endline evaluation.
Within two years of programme implementation, each of the SRLMs has initiated the scale-up of the programme. In Chhattisgarh, based on the success of Swabhimaan in the pilot block of Bastar, the SRLM has approved the scaling up of Swabhimaan in 16 blocks across 12 districts. This is being done in a phased manner with eight blocks across six districts in 2018 and the remaining eight blocks in the subsequent years. Forty CRPs have been chosen from the pilot block as resource persons/master trainers to roll out training in the scale-up blocks. In Odisha, the Odisha Livelihoods Mission (OLM)1 plans to saturate 12 blocks across both intervention districts by 2020. These will then serve as incubation blocks and learning from these locations will be taken up across the state. The mission intends to develop 700 community resource persons to support the scale-up of interventions in 14 blocks of three districts. The OLM has also chosen to set up vertical nutrition programmes to provide support for capacity-building of state and district level programme staff. Similarly, in Bihar, scale-up was initiated in 2019 and will see the intensification of interventions and the saturation of each implementation block by 2021. Existing cadres of staff will act as resource persons in the remaining clusters. Further, phase II will also focus specifically on addressing gender norms and social issues that impact upon women’s nutrition and access to entitlements. Phase II will also focus on replicating the nutrition-sensitive integrated farming systems (NSIFS), a nutrition-based livelihood option, in the scale-up areas. This is in keeping with the Bihar SRLM’s health, nutrition and sanitation strategy to address undernutrition in marginalised communities.
Conclusion
Over the three years of implementation of the Swabhimaan programme, the findings suggest that both the community-led and systems strengthening components of the programme have significant impact on increasing the coverage of essential nutrition-specific and nutrition-sensitive interventions for women and girls. A key component is the development of integrated nutrition microplans developed by the community, utilising the funds provided by the SRLMs. The results of the midline evaluation demonstrate that this is a feasible approach and that women’s collective institutions are able to use cash grants to respond to community-based needs and are able to implement actions to address health and nutrition problems in their community. The results of the endline and impact evaluations are forthcoming and will provide further evidence to inform maternal and preconception nutrition policy at national and state level in support of the scale-up of mechanisms that integrate nutrition interventions into large-scale poverty alleviation programmes delivered via women’s collectives.
For more information, please contact Dr. Vani Sethi at vsethi@unicef.org
Watch a video about this programme at https://www.youtube.com/watch?v=bqnqV2V4tiw
1 Odisha Livelihoods Mission (OLM) is Odisha’s SRLM, an autonomous society under Department of Panchayati Raj, Government of Odisha, implementing National Rural Livelihoods Mission, India’s large-scale poverty alleviation programme.
References
Bulliyya, G, Mallik, G, Sethy, G S, Kar, S K (2007) Hemoglobin Status of Non-School Going Adolescent Girls in Three Districts of Orissa, India. International Journal of Adolescent Medicine & Health. 2007.19; (4):395–406
Butta, Z, Das, J K, Rizvi, A, Gaffey, M F, Walker, N, Horton, S et al (2013) Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. 2013; 382: 452–477. https://doi.org/10.1016/S0140-6736(13)60996-4 PMID: 23746776
Goudet, S, Murari, Z, Torlesse, H, Hatchard, J, Busch-Hallen, J (2018) Effectiveness of programmeme approaches to improve the coverage of maternal nutrition interventions in South Asia. Matern Child Nutr. 2018;14(S4):e12699.
International Institute for Population Sciences (IIPS) and Macro International 2015-16
National Family Health Survey (NFHS-4), 2015–16: India Factsheet
IIPS. Swabhimaan baseline factsheet: Bihar 2016
IIPS. Swabhimaan baseline factsheet: Chhattisgarh 2016
IIPS. Swabhimaan baseline factsheet: Odisha 2016
Ministry of Health and Family Welfare, Government of India and WHO (2017) Guidance document: Nutritional care and support for patients with tuberculosis in India. 2017
Reshmi RS et al Context for layering women’s nutrition interventions on a large scale poverty alleviation programme: Evidence from three eastern Indian states. PLoS ONE 2019. 14(1): e0210836. https://doi.org/10.1371/journal.pone.0210836
Sethi V, Bhanot A, Bhalla S, Bhattacharjee S, Daniel A, Sharma DM, et al: Partnering with women collectives for delivering essential women’s nutrition interventions in tribal areas of eastern India: a scoping study. J Health Popul Nutr. 2017; 36 (20).
Tang AM, Dong K, Deitchler M, Chun M, Maalouf-Manasseh Z, Tumilowicz A, Wanke C. Use of Cutoffs for Mid-Upper Arm Circumference (MUAC) as an Indicator or Predictor of Nutritional and Health Related Outcomes in Adolescents and Adults: A Systematic Review. 2013. Washington, DC: FHI 360/FANTA



