Determinants of adolescent nutritional status and practices in Burkina Faso: A pooled secondary analysis
By Deepali Godha, Maurice Zafimanjaka, Estelle Bambara, Nathalie Likhite and Manisha Tharaney.
Deepali Godha is an independent researcher with expertise in health and population analysis of large datasets using Stata. Working as a lead analyst for almost 14 years, she has used a range of econometric techniques including multivariate regression analysis, multi-level modelling, difference-in-difference analysis, positive deviance analysis and equity analysis for research on a range of topics (adolescents, child marriage, nutrition, child health, health systems, sexual and reproductive health and women’s issues).
Maurice Gerald Zafimanjaka is an economist and public health specialist and the Director of Alive & Thrive’s Project in Burkina Faso. He has over 20 years’ international experience in designing, implementing and monitoring and evaluating, health, nutrition and food security programmes.
Estelle Aïssa Bambara is a nutritionist by training and has been the Director of the Nutrition Division of the Ministry of Health of Burkina Faso since 2019. Prior to that, she led the team responsible for the surveillance and management of malnutrition for five years. She joined the Nutrition Division in 2009.
Nathalie Likhite is Alive & Thrive’s regional social and behavioural change advisor for West Africa. Nathalie has over 20 years’ experience working with international organisations in the research, design and implementation of social and behaviour change programmes in Africa, Asia and Europe.
Manisha Tharaney is the West Africa Programme Director at Alive & Thrive. She has 20 years of experience in Asia and in Africa in nutrition and health systems strengthening. She currently supports Alive &Thrive’s portfolio in West Africa with capacity building, research and policy dialogue for breastfeeding and supporting countries to operationalise the national maternal and young child nutrition programme at scale.
Location: Burkina Faso
What this article is about: This article applies pooled survey data to investigate the levels of malnutrition and associated dietary diversity in adolescents across different regions and socioeconomic strata within Burkina Faso.
Key messages:
- The study found suboptimal dietary diversity and a high consumption of processed and sugary foods. The strong association between dietary diversity and unhealthy food intake/consumption of added sugars is an important consideration for policymakers to reduce the burden of double malnutrition in the country.
- Prevalence of severe malnutrition based on the World Health Organization mid-upper-arm circumference cut-off <16cm was high, especially among younger adolescents.
Introduction
Adolescence, from 10-19 years of age, is a period of rapid physical growth and significant psychosocial and cognitive development during which behaviours around food and physical activity are established. Consequently, adolescence is a critical period for establishing the future health trajectory of adolescents themselves and, in some cases, their children (ENN, 2021). Globally, many low- and middle-income countries are facing a double burden of malnutrition amongst adolescents linked to increased ultra-processed food consumption (Li et al, 2020).
Assessment of nutritional status among adolescents differs from that of children under five years of age and is less well defined globally. Adolescents represent 23.1% of the total population in Burkina Faso (World Health Organization Regional Office for Africa, 2018) and there is increasing interest from the Ministry of Health’s Nutrition Division to better understand the nutrition status and practices of this group. This article analyses the available nutrition data for the adolescent age group using surveys conducted in 2017 and 2018 in Burkina Faso in order to fill this data gap.
Available data
The study used pooled data from the Performance Monitoring and Accountability (PMA, 2020) nutrition surveys which were collected among women 10-49 years of age in Burkina Faso in 2017 (PMA2017/Burkina Faso-R4-HQFQ, 2017) and 2018 (PMA2018/Burkina Faso-R5-HQFQ, 2018). The final sample for all analyses included 2,432 non-pregnant adolescent girls. The PMA 2020 surveys used a multi-cluster design and mobile technology to support low-cost, rapid-turnaround, nationally representative surveys to monitor key health indicators in nine countries in Africa and Asia. The PMA2020 Nutrition Survey aimed to generate actionable data on nutrition interventions at the national level in Burkina Faso (PMA Data, n.d.).
It provided information on three nutritional outcomes:
- Dietary diversity: Minimum dietary diversity was defined as having eaten at least five out of 10 food groups on the previous day (grains, pulses, nuts and seeds, eggs, meat, green leafy vegetables, vitamin A-rich fruits and vegetables, other fruits, other vegetables and dairy).
- Consumption of added sugars: Indicates whether the respondent had consumed any sugary foods (including jiggery, donuts, mandaazi, sweet biscuits, cake or candies) and/or sugary beverages (sweet fruit drinks, sweet tea, fizzy drinks or sugar-sweetened milk tea) on the previous day.
- Mid-upper-arm circumference (MUAC) <16cm: A proxy indicator for assessing nutrition status where a cut-off of 16cm indicates severe malnutrition among adolescents as defined by the World Health Organization (WHO) Integrated Management of Adolescent and Adult Illness (IMAI) guidelines (WHO, 2011). This cut-off was used in the absence of normative WHO guidelines on anthropometric definitions for undernutrition in adolescents.
Independent variables were selected based on a literature review and data availability. They included place of residence, household wealth tertile, age group, ever attended school, living with elders, marital status, employment, household size and unhealthy food habits (yes if respondent had consumed fried and savoury snacks, sugary foods and/or sugary beverages the day before survey).
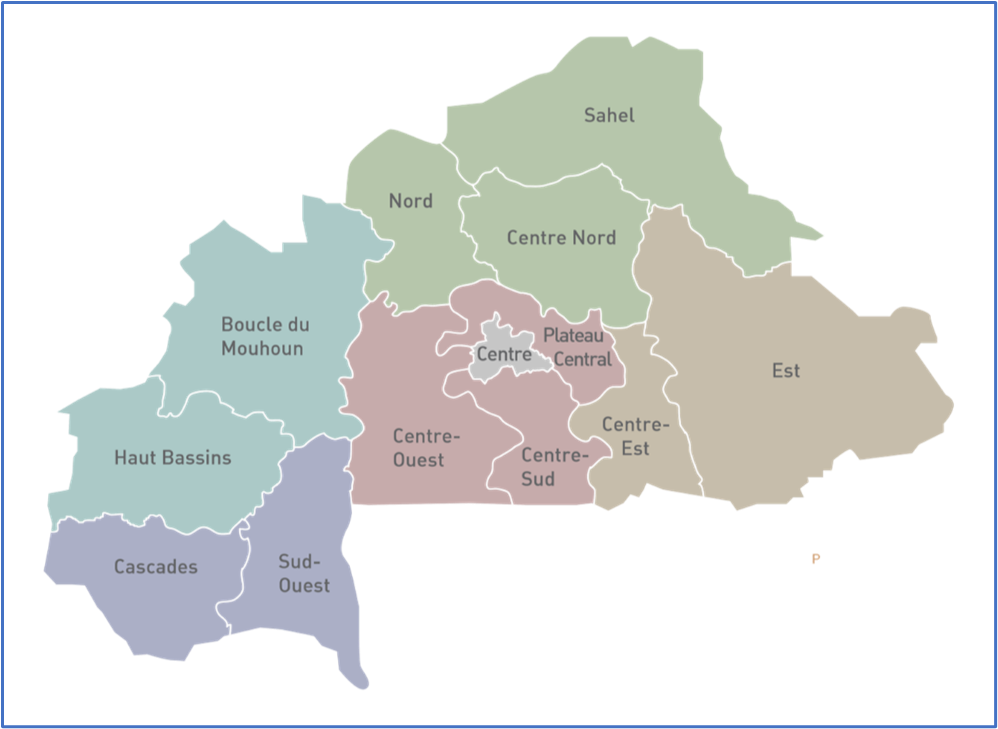
Households were asked about eight aspects of food insecurity in the past 12 months from the date of the survey including ‘worry of not having enough food’, quality, variety, frequency, quantity, availability, hunger level and not eating for an entire day. Household food insecurity was categorised as low/none if less than three aspects were true, moderate if four to six were true or severe if more than six were true. Regions were clustered to form six groups based on geography, feeding practices and cultural proximities (Figure 1).
Figure 1: Six regional clusters of Burkina Faso
Methods
We cross tabulated the outcomes with chi-square tests for selected characteristics to understand the distribution of outcomes in the study sample. In addition, we assessed logistic regression models with multiple variables using a stepwise procedure while screening for confounders. All analyses were conducted using Stata 15.1.
Results
Dietary diversity
Minimum dietary diversity was observed in 24.9% of the adolescents in Burkina Faso with dietary diversity differing by geography, especially between urban (35.3%) and rural areas (22.2%) (Table 1). Dietary diversity amongst adolescents was highest in the Centre region (43.5%) and lowest in the regional group of Sahel, Centre Nord and Nord (10.8%). Adolescents from the wealthiest households had higher dietary diversity (32.7%) than those with intermediate (22.1%) or poor (20.1%) household wealth. Dietary diversity was also higher amongst those who had consumed unhealthy food/drinks the previous day (38.1%) compared to those who had not (16.4%). No significant difference was found by age group, attending school and household food security.
Compared to the reference group (Centre region), adolescents residing in the Sahel, Centre Nord or Nord cluster had 84% reduced odds of achieving minimum dietary diversity (OR 0.16) while those residing in the Est and Centre Est cluster had 71% reduced odds (OR 0.29) (Table 2). The probability of achieving minimum dietary diversity was almost three times higher for those who had an unhealthy food or drink during the previous day compared to the reference group of those who had not (OR 2.90).
Table 1. Prevalence of the three outcomes by various parameters
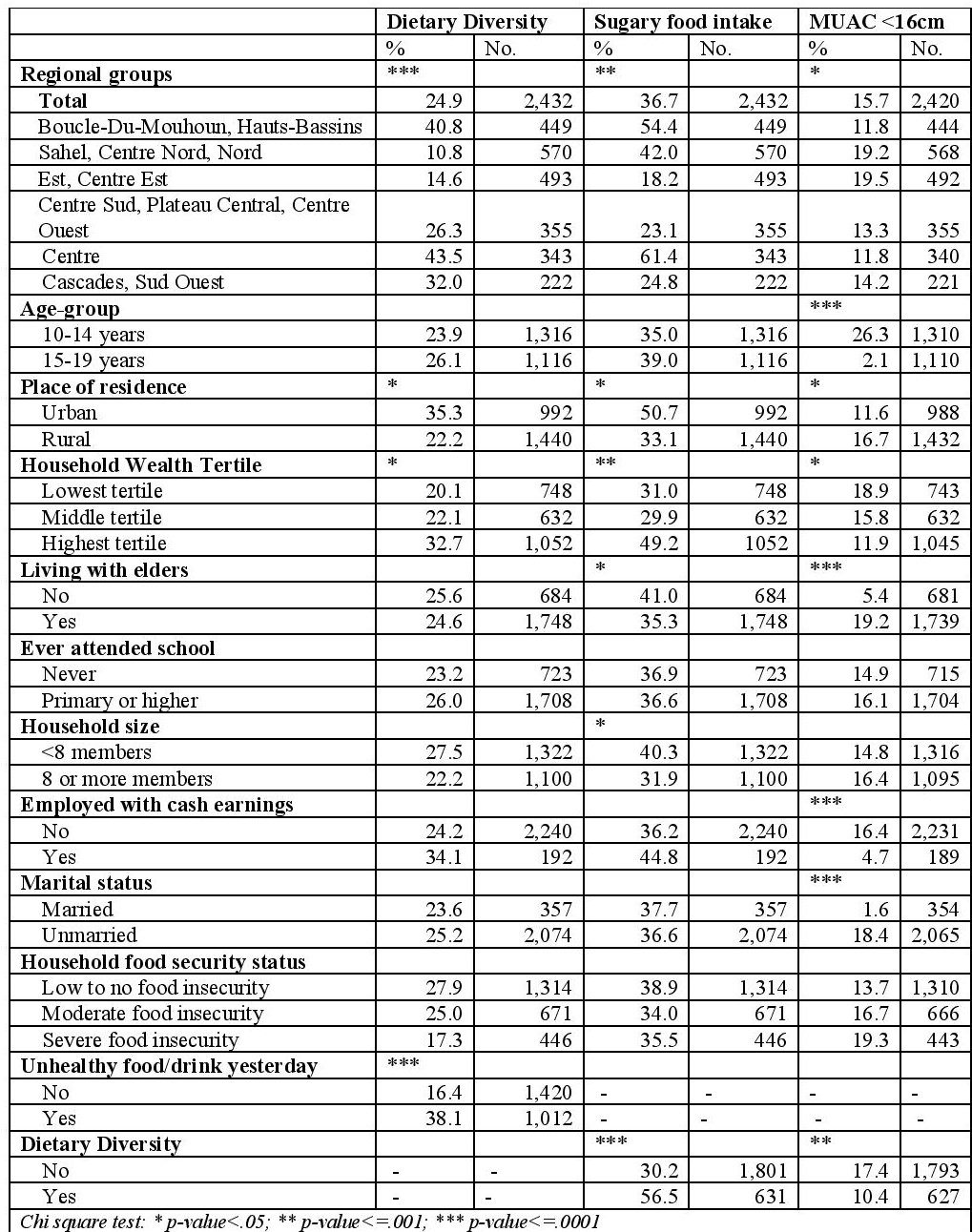
Table 2. Results from multivariate models
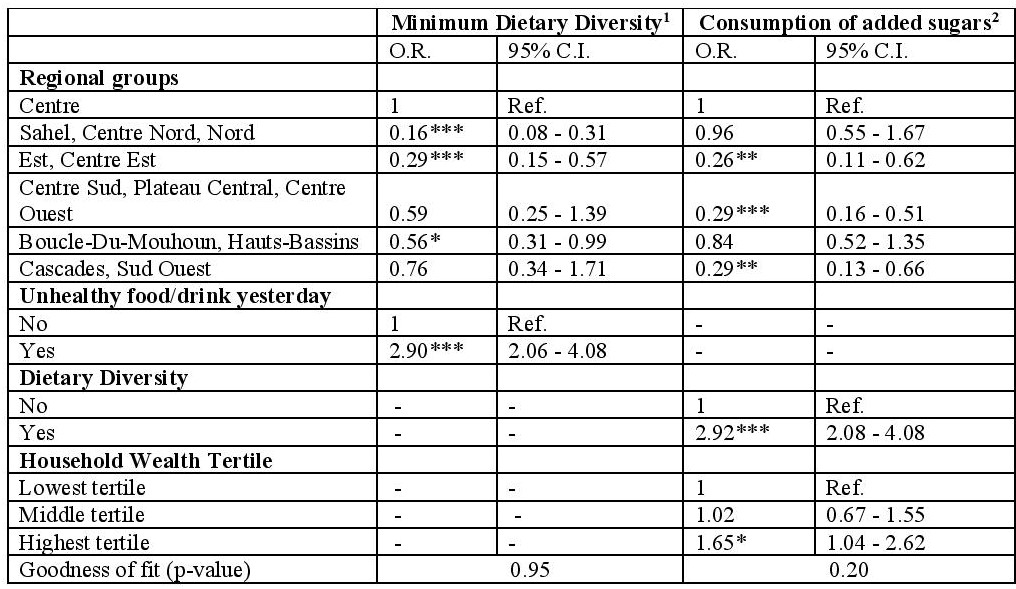
1Adjusted for regional groups and consumption of unhealthy food/drink
2Adjusted for regional groups, dietary diversity and household wealth tertile
Consumption of added sugars
A large proportion of adolescents (36.7%) reported consuming added sugars the previous day with the prevalence of added sugar consumption differing between regional clusters, especially between urban (50.7%) and rural areas (33.1%) (Table 1). The consumption of added sugars was highest in the Centre region (61.4%) and lowest in the Est and Centre Est cluster (18.2%). Adolescents from the wealthiest households had a higher consumption of added sugars (49.2%) compared to those with intermediate (29.9%) or poor (31%) household wealth. Adolescents who achieved minimum dietary diversity reported higher added sugar consumption (56.5%) compared to those who did not (30.2%). The consumption of added sugars was lower among adolescents living with elders (41%) and among those living in larger households with eight or more family members (40.3%).
Compared to the reference group (Centre region), adolescents residing in the Est and Centre Est cluster had 74% reduced odds of added sugar consumption (OR 0.26). Those residing in the Centre Sud, Plateau Central and Centre Ouest cluster and those residing in the Cascades and Sud Ouest cluster had 71% reduced odds (OR 0.29) as compared to the Central region. The probability of added sugar consumption was almost three times higher for adolescents who had achieved minimum dietary diversity compared to those who did not (OR 2.92). Adolescents from the wealthiest households had 65% increased odds of added sugar consumption (OR 1.65) compared to the lowest income household group.
MUAC less than 16 cm
The prevalence of MUAC <16cm (a proxy for severe malnutrition) was estimated to be 15.7% among adolescents but was different across age groups (26.3% in the 10-14 years age group as compared to 2.1% in the 15-19 years age group). Differences in prevalence were noted by geography with higher prevalence in rural areas as compared to urban areas (16.7% and 11.6% respectively) and highest in the regional group of Est and Centre Est at 19.5%. Prevalence was lower in adolescents from wealthy households (11.9%) compared to middle-income households (15.8%) and poorer households (18.9%). Prevalence of MUAC <16cm was higher among adolescents living with elders, as well as adolescents who were not employed or had no cash earnings, or who were unmarried. Similarly, adolescents with higher diet diversity scores had a lower prevalence of MUAC <16cm (10.4% versus 17.4%). No significant difference was found by attending school, household size, household food security and the consumption of unhealthy foods or drink the previous day.
Figure 2 shows that the total prevalence of unhealthy food intake was higher in urban areas and significantly different by household wealth as compared to rural areas. The high prevalence of unhealthy food intake in urban areas may be as a result of greater access to these foods although different behaviours or cultural norms may also play a role. In rural areas, dietary diversity did not appear to vary much by household wealth. This was also the case for the consumption of unhealthy foods albeit the source (homemade, vendor/restaurant, processed) differed. In urban areas, the consumption of vendor and processed foods varied among the upper two wealth quintiles. Adolescents from the poorest households consumed mostly homemade unhealthy foods, those from the middle class mainly consumed unhealthy foods from a vendor or restaurant while those from the richest households tended to buy processed foods. These relationships require further investigation.
Figure 2. Prevalence of unhealthy food and source of unhealthy food by household wealth and area of residence among adolescents, 2018
Discussion
Our findings show an association between high dietary diversity and added sugar consumption. This reflects findings in previous research and can potentially be explained by typical food habits in this age group (Moreno et al, 2010) as well as affordability (Zhang et al, 2019) and the accessibility of unhealthy foods (Stok et al, 2018).
The prevalence of severe malnutrition based on our MUAC definition was high, especially in the younger adolescents. The rate is very high compared to rates of severe malnutrition in children under five but, without standard definitions for adolescents, we are unable to know how this compares to other contexts. The fact that the prevalence of MUAC <16cm was found to be mostly restricted to the younger adolescents suggests that nutrition programmes for adolescents should be tailored to age.
Strategies to improve nutrition outcomes in adolescents
Reducing malnutrition and improving dietary quality among adolescents in Burkina Faso will require strategies and interventions to reduce the consumption of added sugars and other unhealthy foods, particularly in urban areas. The Determinants of Nutrition and Eating framework (Stok et al, 2018) outlines some strategies that have proven or have the potential to be effective:
- Increased taxation can reduce consumption and motivate healthier food choices. Several countries have implemented this strategy although with limited success (Haque et al, 2020).
- National policies to control the sale and marketing of unhealthy foods, curb aggressive advertisements and ensure strict monitoring and enforcement have also shown impact (Haque et al, 2020).
- Tailored health education and nutrition counselling to increase adolescents’ awareness, particularly on ‘hidden’ ingredients and on the long-term adverse health effects of added sugars, can be an effective strategy (Haque et al, 2020).
- Similarly, national nutritional guidelines and regulations on harmful ingredients have shown promise. Dietary recommendations should promote the adequate consumption of plant foods, low-fat dairy products, vegetable oils, nuts, poultry and fish and limit the consumption of red meat, sweets and sugary drinks.
- Limits on the sale of processed and sugary foods in school canteens and other environments have been effective to a lesser extent (von Philipsborn et al, 2019).
In summary, a multi-pronged approach is needed to address nutrition amongst adolescents in Burkina Faso.
The study has some limitations and the findings should be interpreted with caution. 1) Data availability constrained outcome selection and the parameters used in multivariate modelling. 2) Distribution of household wealth was almost dissociated by area of residence with most of the poorest households in rural areas and vice versa (correlation: 0.62). 3) There was insufficient evidence that the multivariate model for dietary diversity was a good fit for the data. 4) Although MUAC has been used to define severe malnutrition, its effectiveness is still largely unknown. Lower MUAC measurements in younger adolescents may be due to differential growth spurts across the adolescent age spectrum that usually occur towards later adolescence. If true, there is a high probability of misclassification among the older age group of 15-19 years resulting in missing malnourished children. Nonetheless, the results provide useful insights.
Conclusion
This study provides an understanding of the nutritional health of adolescents in Burkina Faso using recent national nutrition surveys. The study found suboptimal dietary diversity and a high consumption of processed and sugary foods. The prevalence of severe malnutrition based on the WHO MUAC cut-off <16 cm was high, especially among younger adolescents. The strong association between dietary diversity and unhealthy food intake/consumption of added sugars is an important consideration for policymakers to reduce the burden of double malnutrition in the country. Given that nutrition behaviours and habits are developed by early adolescence, designing nutrition interventions for school-age children should be promoted as a public health strategy. In addition, wherever possible, food systems should be regulated and national policies that tax unhealthy foods, regulate marketing and increase public awareness are needed.
References
Emergency Nutrition Network (ENN) (February 2021) Adolescent Nutrition Meeting Report 2021.
Haque, M, McKimm, J, Sartelli, M, Samad, N, Haque, SZ and Bakar, MA (2020) A narrative review of the effects of sugar-sweetened beverages on human health: A key global health issue. Journal of Population Therapeutics and Clinical Pharmacology, 27(1), e76–e103. https://doi.org/10.15586/jptcp.v27i1.666
Li, L, Sun, N, Zhang, L, Xu, G, Liu, J, Hu, J, Zhang, Z, Lou, J, Deng, H, Shen, Z and Han, L (2020) Fast food consumption among young adolescents aged 12–15 years in 54 low- and middle-income countries. Global Health Action. https://doi.org/10.1080/16549716.2020.1795438
Moreno, LA, Rodríguez, G, Fleta, J, Bueno-Lozano, M, Lázaro, A and Bueno, G (2010) Trends of dietary habits in adolescents. Critical Reviews in Food Science and Nutrition. https://doi.org/10.1080/10408390903467480
Performance Monitoring and Accountability 2020 (PMA2020) Household and Female Survey Round 4, PMA2017/Burkina Faso-R4-HQFQ. (2017).
Performance Monitoring and Accountability 2020 (PMA2020) Household and Female Survey Round 5, PMA2018/Burkina Faso-R5-HQFQ. (2018).
PMA Data. Retrieved July 21, 2021, from https://www.pmadata.org
Stok, FM, Renner, B, Clarys, P, Lien, N, Lakerveld, J and Deliens, T (2018) Understanding eating behavior during the transition from adolescence to young adulthood: A literature review and perspective on future research directions. Nutrients, 10(6), 1–16. https://doi.org/10.3390/nu10060667
von Philipsborn, P, Stratil, JM, Burns, J, Busert, LK, Pfadenhauer, LM, Polus, S, Holzapfel, C, Hauner, H.and Rehfuess, E (2019) Environmental interventions to reduce the consumption of sugar-sweetened beverages and their effects on health. In Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD012292.pub2
WHO Regional Office for Africa (2018) Adolescent health in Burkina Faso. https://www.afro.who.int/sites/default/files/2019-08/28 Burkina Faso AH24022019.pdf
WHO (2011) Integrated Management of Adolescent and Adult Illness district clinician manual: Hospital care for adolescents and adults – Guidelines for the management of illnesses with limited resources.
Zhang, CQ, Wong, MCY, Zhang, R, Hamilton, K and Hagger, MS (2019) Adolescent sugar-sweetened beverage consumption: An extended Health Action Process Approach. Appetite. https://doi.org/10.1016/j.appet.2019.104332


