Weekly iron and folic acid supplementation and nutrition education for adolescent girls in Africa and Asia
By Anjali Bhardwaj, Lucy Murage, Shibani Sharma, Dhian Dipo, Christine Makena, Marion Roche and Mandana Arabi
Anjali Bhardwaj is the Regional Manager for Adolescents and Women’s Health and Nutrition for Asia at Nutrition International. She is an anthropologist and public health professional.
Lucy Murage is the Regional Advisor for Adolescents and Women’s Health and Nutrition for Africa at Nutrition International. She is a public health and nutrition specialist with over 16 years of expertise in health systems strengthening and health and nutrition technical assistance.
Shibani Sharma is a Junior Technical Officer for the Adolescents and Women’s Health and Nutrition programme at Nutrition International’s headquarters in Ottawa. She previously worked in India for over five years supporting nutrition programmes at national and sub-national level.
Dhian Dipo is Director of Public Health Nutrition at the Directorate General of Public Health, Ministry of Health (MoH), Republic of Indonesia. Dhian is a public health nutritionist with over 20 years of experience as a civil servant with the MoH.
Christine Makena is a Senior Programme Officer in charge of the Kenya Adolescent Health and Nutrition programme at Nutrition International, Kenya Office. Christine has over 10 years of experience working in integrated food and nutrition programmes in development contexts.
Marion Roche is the Senior Technical Advisor for Adolescents and Women’s Health and Nutrition at Nutrition International where she leads the design, introduction, scale-up and evaluation of adolescent nutrition interventions. She has over 15 years of experience in public health nutrition programme implementation and research.
Mandana Arabi is Vice President and Chief Technical Advisor for Global Technical Services at Nutrition International headquarters. She has over two decades of experience in the nutrition and health sector during which she held leadership positions at UNICEF, WHO, GAIN, the New York Academy of Sciences, Cornell University and the Iranian MoH.
The authors thank the many people who supported the preparation of this article and adolescent nutrition programme. The authors also acknowledge the immense support from the national and sub-national governments and health and education staff in Nutrition International’s supported areas in Ethiopia, Kenya, Senegal, Tanzania, Bangladesh, India and Indonesia. Nutrition International’s adolescent nutrition programmes are financially supported by Global Affairs Canada, the Government of Canada and the Department of Foreign Affairs and Trade of the Government of Australia.
Location: Asia & Africa
What this article is about: This article outlines the activities carried out by Nutrition International since 2015, providing weekly iron and folic acid (IFA) supplementation to adolescents residing in six separate high-risk countries.Key messages:
- Despite regional supply chain challenges and the complications due to the COVID-19 pandemic, weekly programmes were successful in supporting governments to increase IFA supplementation coverage.
- There remains a paucity of data on adolescent health outcomes which makes the design, implementation and monitoring of adolescent health projects particularly difficult.
- Although school-based delivery models are effective at the population level, reaching adolescents who do not attend school – who are often at higher risk –remains a significant challenge. Governments should prioritise reaching these isolated groups in order to meet public health policy objectives.
Background
Iron deficiency anaemia is the number one cause of lost disability-adjusted life years in adolescent girls and is estimated as the largest cause of morbidity and mortality for this group globally (WHO, 2017). Over 30% of adolescent girls in low-and-middle-income countries (LMICs) have anaemia which is associated with reduced cognitive development, academic and productive potential, decreased wellbeing and increased morbidity and mortality (WHO, 2011).
The World Health Organization (WHO) recommends weekly iron and folic acid (IFA) supplementation (WIFAS) to reduce anaemia in adolescent girls 10-19 years of age and women 15-49 years of age in regions where more than 20% of women of reproductive age (15-49 years) are anaemic (WHO, 2011).
Since 2015, Nutrition International (NI) has built upon previous work in Chhattisgarh, India and begun to work with national and subnational governments in six African and Asian countries to implement adolescent nutrition programmes under the ‘Right Start’ initiative (2015-2020) which includes WIFAS and nutrition education to reduce anaemia. While all programmes are based on WHO recommendations, each one is tailored to fit national nutrition and anaemia reduction strategies so no two are identical. This article shares diverse learning experiences from programme implementation over the past several years.
Programme description
NI consulted with the government in each country to prioritise programme areas in six Asian and African countries where the prevalence of anaemia was high among women of reproductive age, i.e., India, Indonesia, Kenya, Senegal, Ethiopia and Tanzania (Table 1).
Table 1: Anaemia rates among pregnant women and women of reproductive age (15-49 years) in NI-supported countries
| Anaemia rates among age group | Ethiopia | Kenya | Senegal | Tanzania | India | Indonesia |
| Pregnant women | 29% | 41.6% | 61%a | - | 50.4 %a | 48.9%a |
| Women of reproductive age (15-49 years) | 24% | 21.9% | 54.1%b | 28.8% | 53.2 % a | 26%b |
| Source | Ethiopia Demographic and Health Survey (EDHS), 2016 | Kenya National Micronutrient Survey (KNMS), 2011 | a. Demographic and Health Survey – Multiple Indicator Cluster Survey (DHS-MICS 2010-11) b. Senegal Demographic and Health Survey DHS, 2017 | Tanzania National Nutrition Survey NNS, 2018 | National Family Health Survey (NFHS 4) 2015-16
| a. RISKESDAS: The National Institute of Health Research and Development, Ministry of Health, Republic of Indonesia (2018) b. RISKESDAS (2013) |
In each country, NI consulted with the government to develop optimal strategies for the implementation of WIFAS and nutrition education programmes. This was done in accordance with WHO guidelines and through adapting dosage recommendations to take into consideration access to and availability of supplies. NI provided technical assistance and operational support to the government health and education departments, securing multi-sector government commitment towards the WIFAS project.
The operational models differed between countries according to specific contexts and geographic coverage. NI collaborated with the government and non-governmental organisations to deliver adolescent nutrition programming as summarised in Table 2.
Table 2: Programme operational arrangements according to country
| Country | Programme governance | Programme implementation |
| India | NI in close collaboration with the Ministries of Health and Family Welfare and Women and Child Development | Local non-governmental organisations: Gorakhpur Environmental Action Group, Child in Need Institute and TRIOs Programme areas: Uttar Pradesh, Gujarat, Madhya Pradesh, Chhattisgarh and West Bengal |
| Indonesia | NI in close collaboration with the Ministry of Education and Culture, Ministry of Health (MoH), the Ministry of Religious Affairs and the Ministry of Home Affairs | Direct implementation model with all field-level programme personnel directly engaged by NI. Programme areas: West Java, Banten, East Nusa Tengarra and East Java
|
| Kenya | NI in close collaboration with MoH and the Ministry of Education (MoE) | Population Services International (pilot phase); County government programme managers in five counties (Busia, Nakuru, Nandi, Vihiga and Makueni) (scale-up) |
| Senegal | NI in close collaboration with MoH and MoE | Cellule de Lutte contre la Malnutrition (CLM) at national level and in Dakar, Thies, St Louis, Kaolack, Ziguinchor, Kolda and Sedhiou regions |
| Ethiopia | NI in close collaboration with MoH and MoE | MoH and MoE at national level and in Amhara, Oromia, Sidama and SNNP regions |
| Tanzania | NI in close collaboration with MoH and MoE | Amref Health Africa (pilot phase) and regional governments and TFNC (scale-up). |
When NI expanded its earlier adolescent nutrition work from Chattisgargh in India to additional states in India and five additional countries across Asia and Africa in 2015, WIFAS programmes were either not in place or were in nascent stages. In some countries, adolescent nutrition was prioritised in national policies but relevant operational guidelines, health management information system (HMIS), supply chains and implementation channels had not been set up and finances were not allocated for programmes.
In the initial years of programming, demonstration projects were implemented to garner support for multi-sector engagement, highlight best practices and generate data on the feasibility and cost-efficiency of platforms and partnerships for reaching adolescents. Collaborative efforts were made between partners to identify effective delivery channels and platforms for both WIFAS and nutrition education for girls in- and out-of-school. Support from NI included developing supplementation guidelines and costed subnational implementation plans, procuring IFA tablets from local manufacturers, facilitating training, conducting supervision and setting up monitoring systems. The initial focus was on the design and implementation of the WIFAS component, complemented by nutrition education related to anaemia and WIFAS. Later, a broader gender-responsive approach was implemented in most countries.
Delivery platforms and partnerships
For adolescent health and nutrition interventions, in-school platforms are both labour- and cost-efficient as they allow access to the largest groups of adolescents (Bundy, 2011). Schools are also connected to the health system, often through frontline workers from local health facilities facilitating referrals. Thus, in most countries, government-funded schools were the preferred primary delivery platforms.
However, in some countries, access to education is not universal1 so the poorest and most isolated girls may be excluded if programmes are exclusively implemented in schools. In India, WIFAS programmes reached out-of-school adolescent girls through community-based outreach centres as per national policy. In the early phases, Kenya and Ethiopia tested approaches for reaching girls in the community through the health system; however, adolescents were not commonly accessing the health system for preventative nutrition and health services. Ethiopia is now reaching out-of-school girls via community platforms that use ‘motivator’ girls who are trained to provide information on nutrition and anaemia to their peers who are not attending school, encouraging them to attend the health facility for supplementation. This model is not yet at scale but there are plans to expand to high burden areas.
IFA supplies
The provision of IFA tablets through robust supply chains is a key element within adolescent nutrition programmes. Adolescent girls require WIFAS using a distinct formulation of folic acid as per the WHO guideline. Although IFA tablets for weekly supplementation became available in the UNICEF supply catalogue in late 2019, this formulation is still not part of the WHO Essential Medicine List (EML), meaning that governments are constrained from purchasing them (Roche et al, 2021). NI therefore supports the supply chain for the respective government-endorsed product which is currently the formulation used for pregnant women.
NI has provided financial, technical and operational support to governments to strengthen the supply of commodities through improving health staff’s forecasting, procurement and supply capacity, strengthening supply chain management systems and providing training for teachers, health staff and other district officials. NI supported efforts to harmonise joint forecasting and procurement to ensure supply for both maternal and adolescent nutrition programmes.
Nutrition education
Adolescent nutrition programmes have included robust evidence-based behaviour change interventions (BCI) that were developed following rigorous formative research with adolescent girls and boys, parents, health staff, teachers, community influencers and religious leaders. The BCI strategy was critical to obtaining acceptance from the adolescent girls and their families with a focus on the benefits of WIFAS and anaemia reduction for school performance and the wellbeing of adolescent girls rather than on maternal and infant health outcomes.
Gender mainstreaming
NI recognises that it is essential to work through a gender-responsive approach to successfully engage women, girls, men and boys in adolescent programmes that strive to promote gender equality and overcome the inequities faced by adolescent girls. Anaemia disproportionately impacts adolescent girls, thus girls were prioritised for WIFAS but both adolescent girls and boys were reached with nutrition education. Men’s buy-in to the programme was crucial to reaching adolescent girls and achieving scale-up, for example in cases where fathers or brothers are unwilling to enrol adolescent girls into interventions, success will not be possible. Gender barriers leading to reduced access to school for adolescent girls were identified in all settings and included menstrual hygiene management, early marriage and adolescent pregnancy, poverty and stigma.
WIFAS and nutrition education service providers
The training and capacity-building of service providers from health and education departments was undertaken at scale through formal and on-the-job training. This aimed to build knowledge of adolescent nutrition and strengthen capacity on operational issues such as procurement planning. Programme managers from the MoH, MoE and the Ministry of Agriculture were selected and trained to be trainers. They then cascaded the trainings to other subnational frontline health workers, community health volunteers, teachers and peer educators.
In most contexts, teachers were responsible for managing all aspects of the programme within the schools, i.e., conducting nutrition education, ensuring effective supplementation,2 managing IFA supplies and reporting on activities. Peer educators were also trained to support supplementation and, at times, to help teachers during the nutrition education sessions. Health workers collaborated with teachers, ensuring IFA supplies reached schools and connecting schools and health facilities. Since all WIFAS programmes were government-led, all duties carried out by teachers and health workers were incorporated into their work tasks by default in government schools.
Generating evidence and measuring progress
When possible, coverage of weekly IFA supplementation programmes was reported through the governments’ HMIS. When HMIS did not include IFA supplementation indicators, for example in most African countries, parallel systems using paper-based forms were used. Data was recorded by teachers and consolidated by NI programme managers.
NI also conducted quantitative and qualitative surveys to measure the progress of country-level programmes and identify areas of improvement. Baseline assessments were conducted at the start of each programme with midline surveys conducted after two to three years of implementation and endline surveys conducted in year five. Within NI’s global Nutrition Intervention Monitoring System, a set of uniform survey tools and data collection methodologies that were easily adaptable to different national contexts was developed. Surveys using these modules have been implemented in all countries since 2017 with the exception of India where there was already a reliable HMIS system for programme monitoring.
Programme adaptations to the COVID-19 pandemic
After school closures disrupted the WIFAS programmes, alternative models of programming emerged in different countries and NI advocated for and supported the delivery of WIFAS through community outreach wherever possible. Adaptations included providing additional IFA tablets to cover the period of school closures, delivering IFA tablets to homes, sending IFA tablets with remote school curriculum packages, using new channels of communication or adapting digital platforms to continue counselling, nutrition education, data collection and monitoring of IFA supplies.
Results/outcomes
Over the years of programme implementation, an increasing number of adolescent girls have been reached with WIFAS and nutrition education across the six programme countries with more success seen in countries in Asia rather than Africa (Figure 1).
Figure 1: Additional3 adolescent girls who consumed the recommended weekly IFA supplements by country from 2016 to 20194
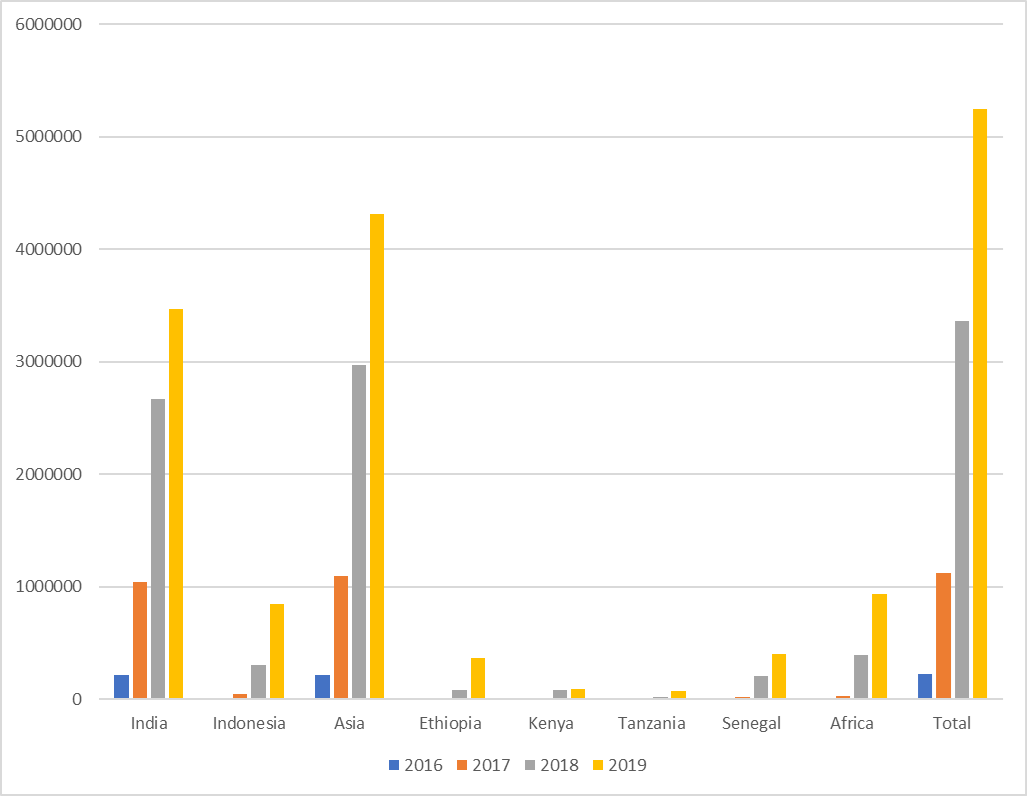
In total, through the scale-up of the programme, an estimated 1.2 million cases of anaemia have been averted5. NI’s programme evaluation survey results clearly show increases in receipt and adherence to WIFAS over time, indicating the successful implementation of the programmes and BCI strategies.
Nearly 3.7 million adolescents, including almost one million boys, were reached with nutrition education over two years which includes the increased use of social media to reach this group such as in Senegal (Box 1).
Box 1: Use of social media for increased nutrition messaging in Senegal
During the COVID-19 pandemic, the use of digital communication led to an increase in adolescents reached with nutrition messaging in Senegal where the project's Facebook page reached 7,682 subscribers. Messages on sexual and reproductive health and nutrition reached 44,269 people and generated thousands of interactions (likes, comments etc.). More than 71% of the people reached were male. Adolescents and youth (13 to 24 years of age) represent approximately 65% of the readers and users of the Facebook page. Young adults (25-34 years of age) and adults (over 34 years of age) represent 22% and 13% of the page's readers and followers, respectively.
In addition, more than 195,000 frontline workers were trained to deliver and support the implementation of the adolescent nutrition programme.
Successes, challenges and lessons learned
WIFAS programmes were successful in progressively supporting governments to create enabling environments and to develop capacity for delivering adolescent nutrition programmes which resulted in substantial increases in IFA supplementation and nutrition education coverage.
Lack of adolescent specific data
National HMIS do not capture certain indicators related to adolescents in many countries. In population surveys, older adolescents’ data is combined with women of reproductive age (15-49 years of age) and data for younger adolescents, even for important indicators such as anaemia, illness and disease, is not captured at all. This paucity of data poses a significant challenge in programme development. NI addressed this by conducting formative research at the beginning of each programme to understand the aspects specific to adolescent nutrition in each context. These were integral to designing the programme, particularly the BCI strategy.
Considerations around IFA supplies
Shortages in IFA tablets are common in many LMICs where nutrition programmes are not prioritised. Regular stockouts, as well as the irregular and inequitable distribution of IFA supplements, pose immense challenges. To remedy this, NI identified supply chain management as a priority activity and provided the necessary technical assistance and operational support. This resulted in governments taking increasing responsibility for procuring IFA supplements during the scale-up period even if NI still provided financial support to cover the cost of the supplements.
The WHO-recommended formulation of weekly IFA supplements for adolescent girls is 60 mg iron and 2.8 mg folic acid. As this specific formulation was not available for purchase when NI began programming, maternal daily IFA supplements, which provide 60 mg iron and 0.4 mg folic acid, were used. To address this issue, NI collaborated with UNICEF to conduct market scoping to develop an appropriate product. This included conducting a user preference survey with adolescent girls from six countries in 2017. As previously mentioned, the adolescent-specific IFA formulation became available in late 2019 but is not yet available in any of the NI programme countries due to the cost and absence from the WHO EML.
COVID-19 related challenges and successes
Adolescent nutrition programming consistently evolved during the COVID-19 pandemic where innovative approaches successfully supported the continuation of programming. Digital technology and virtual platforms emerged as the most reliable medium for nutrition education.
Through programme adaptations, coverage of WIFAS increased after an initial drop, with more girls being reached via community platforms. This was made possible by collaboration with local champions such as village midwives, teachers, health workers and youth groups.
Enhancing adolescent participation
NI’s programmes have ensured that adolescents led the key activities and provided crucial support to ensure the continuation of the programmes. Examples of adolescents’ engagement include acting as ‘motivator’ girls in Ethiopia, designing BCI campaign slogans in Kenya and participating in a content creation workshop as adolescent champions in Indonesia. These activities have contributed to programme acceptance.
Reaching out-of-school girls
Coverage among out-of-school adolescent girls remains low. This group is harder to reach as they are geographically scattered, often marginalised from the health system and likely to be in resource-poor settings yet they experience a higher risk of malnutrition. National governments need to make additional targeted investments to reach out-of-school adolescent girls with WIFAS and nutrition education. Lessons learned from India’s experience in reaching both in- and out-of-school-adolescent-girls in five states are important and show that designating pre-existing, functional platforms at the community level for adolescent health and nutrition interventions could be effective in other countries.
Leading advancements in adolescent nutrition programming and training
Globally, efforts were made to advance the state of knowledge and good practice in policy and programme delivery for adolescent nutrition and specifically for WIFAS6. NI’s efforts contributed to IFA supplements becoming available in their recommended dosages for weekly supplementation. NI worked with academic research partners to understand the efficacy of WIFAS for optimising blood and plasma folate levels for neural tube defect prevention (Samson, 2020). This addressed a critical gap to having weekly IFA supplements eligible for consideration for the EML for anaemia or neural tube defects (Roche, 2021).
NI is currently leading the development of key technical resources to support capacity building for programme staff, partners and interested stakeholders. The Adolescent Nutrition and Anaemia Online Course6 with 15 modules was developed and launched by NI to overcome gaps in the availability of global adolescent nutrition training. Other resources include Frequently Asked Questions (FAQs) for WIFAS7, case studies from different countries and tools to support the gender mainstreaming process.
Conclusion
NI’s experiences demonstrate the successful establishment and scale-up of WIFAS across several countries in Asia and Africa with the prioritisation of supply chain management, the enhanced engagement of adolescents themselves and the adaptations to reach girls out-of-school being key attributes. The programmes have also focused on highlighting the gender inequities in girls’ access to school, including menstrual hygiene management, early marriage, adolescent pregnancy, poverty and stigma. Since 2019, as adolescent nutrition programmes have matured, greater focus is being given to nutrition education for both adolescent girls and boys.
The COVID-19 pandemic highlighted the shortfalls of a complete reliance on school platforms for health and nutrition service delivery while also highlighting the importance of access to education for overall adolescent wellbeing. There is an urgent need among all partners to develop more resilient and adaptable programmes that feature active engagement and participation from adolescents and their communities with, in addition, the engagement of government needed to improve the responsiveness of health systems and services.
For more information, please contact Anjali Bhardwaj at abhardwaj@nutritionintl.org.
To find out more about Nutrition International’s adolescent programmes, please visit here.
1 According to UNESCO data, 62 million adolescents of lower secondary school age (10-14 years) and 138 million adolescents of upper secondary age (15-17 years) are out-of-school. http://uis.unesco.org/sites/default/files/documents/new-methodology-shows-258-million-children-adolescents-and-youth-are-out-school.pdf
2 Directly Observed Therapy is a method of medicine administration where the health care provider (in this case the teacher) watches a person take their medication.
3 This means the additional girls that were reached due to NI's support for the programme. With the exception of India, in all other countries the baseline was zero when the adolescent nutrition programmes were initiated in 2015.
4 Source of data: Additional adolescent girls who consumed the recommended scheme of WIFA (12 tablets in last six months) as reported on governments’ HMIS portals. In case HMIS data is not available for any particular year, annual sample surveys were undertaken to estimate additional coverage.
5 Calculated as per impact-based modelling through the Outcome Modelling for Nutrition Impact tool (https://www.nutritionintl.org/learning-resource/omni/)
6 Nutrition International, adolescent nutrition and anaemia (ANA) course https://global.learning.nutritionintl.org/index.The ANA course was developed to build the capacity of individuals and organisations to better understand adolescent nutrition from a biological and social perspective, as well as learn from programme experiences from multiple sectors. The ANA course is increasingly being used as a key reference material in a variety of countries for adolescent nutrition.
7 Nutrition International, Frequently Asked Questions. https://www.nutritionintl.org/wp-content/uploads/2019/04/WIFAS_for_Adolescents_FAQs_2019.pdf
References
Agence Nationale de la Statistique et de la Démographie - ANSD/Sénégal and ICF International (2012) Enquête Démographique et de Santé à Indicateurs Multiples Sénégal (EDS-MICS) 2010-2011. Claverton, Maryland, USA: ANSD and ICF International. http://dhsprogram.com/pubs/pdf/FR258/FR258.pdf.
Agence Nationale de la Statistique et de la Démographie - ANSD/Sénégal and ICF (2018) Senegal: Enquête Démoggraphique et de Santé Continue (EDS-Continue) 2017. Dakar, Sénégal: ANSD and ICF. http://dhsprogram.com/pubs/pdf/FR345/FR345.pdf
Bundy, D, de Silva, N, Horton, S, Patton, G, Schultz, L and Jamison, D (2017) Child and Adolescent Health and Development: Realizing Neglected Potential. Worldbank.org. https://elibrary.worldbank.org/doi/abs/10.1596/978-1-4648-0423-6_ch1
Central Statistical Agency (CSA) [Ethiopia] and ICF (2016) Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF.
International Institute for Population Sciences (IIPS) and ICF. 2017. National Family Health Survey (NFHS-4), 2015-16: India. Mumbai: IIPS.
Ministry of Health, Community Development, Gender, Elderly and Children (MoHCDGEC) [Tanzania Mainland], Ministry of Health (MoH) [Zanzibar], Tanzania Food and Nutrition Centre (TFNC), National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS) [Zanzibar] and UNICEF (2018) Tanzania National Nutrition Survey using SMART Methodology (TNNS) 2018. Dar es Salaam, Tanzania: MoHCDGEC, MoH, TFNC, NBS, OCGS, and UNICEF
Ministry of Health and Family Welfare (MoHFW), Government of India, UNICEF and Population Council (2019) Comprehensive National Nutrition Survey (CNNS) National Report. New Delhi.
National Institute of Population Studies (NIPS) [Pakistan] and ICF (2019) Pakistan Demographic and Health Survey 2017-18. Islamabad, Pakistan, and Rockville, Maryland, USA: NIPS and ICF
National Institute of Population Research and Training (NIPORT), Mitra and Associates, and ICF International (2013) Bangladesh Demographic and Health Survey 2011. Dhaka, Bangladesh and Calverton, Maryland, USA: NIPORT, Mitra and Associates, and ICF International.
Roche, M, Bury, L, Yusadiredja, I, Asri, E, Purwant,i T, Kusumiati, S et al (2018) Adolescent girls’ nutrition and prevention of anaemia: a school-based multisectoral collaboration in Indonesia. BMJ 2018; 363 doi: https://doi.org/10.1136/bmj.k4541
Roche, M, Samson, K, Green, T, Karakochuk, C and Martinez, H (2021) Weekly iron and folic acid supplementation (WIFAS): a critical review and rationale for inclusion in the essential medicines list to accelerate anemia and NTD reduction. Advances in Nutrition. 12(2), 334-342. https://doi.org/10.1093/advances/nmaa169
Samson, K, Loh, S, Lee, S, Sulistyoningrum, D, Khor, G, Shariff, Z, Ismai, I, Yelland, L, Leemaqz, S, Makrides, M, Hutcheon, J, Roche, M, Karakochuk, C and Green, T (2020) Weekly iron-folic acid supplements containing 2.8 mg folic acid are associated with a lower risk of neural tube defects than the current practice of 0.4 mg: a randomised controlled trial in Malaysia. BMJ global health, 5(12), e003897. https://doi.org/10.1136/bmjgh-2020-003897
UNESCO (2021) One year into COVID-19 education disruption: Where do we stand? United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2019 https://en.unesco.org/news/one-year-covid-19-education-disruption-where-do-we-stand
World Health Organization (2017) Global Accelerated Action for the Health of Adolescents (AA-HA!): guidance to support country implementation. Geneva: World Health Organization http://www. who.int/maternal_child_adolescent/documents/ adolescents-health/en/
World Health Organization (2011) Guideline: Intermittent iron and folic acid supplementation in menstruating women. World Health Organization, 2011. whqlibdoc.who.int/ publications/2011/9789241502023_eng.pdf


