Adapting the MAMI Care Pathway Package in India: Progress and direction
Praveen Kumar is Director Professor at Lady Hardinge Medical College and associated Kalawati Saran Children’s Hospital, New Delhi, India, and Deputy Lead cum Coordinator of the National Centre of Excellence for Children with Severe Acute Malnutrition (NCoE-SAM).
Rajesh Kumar Sinha is Senior Programme Manager at NCoE-SAM.
Srishti Arora is Senior Consultant for the NCoE-SAM.
Abner Daniel is Nutrition Specialist with UNICEF India.
Sanjay Prabhu is Senior Consultant Paediatrics, BJ Wadia Hospital for Children, Parel, Mumbai, India.
Anil Kumar Jaiswal is Head of the Department of Paediatrics, Patna Medical College and Hospital, India.
Simin Irani is a neonatologist currently working with UNICEF and the Government of Maharashtra in areas of Early Childhood Development, Nutrition and Newborn health.
Anil Kumar Tiwari is Assistant Professor, Department of Paediatrics, Patna Medical College and Hospital, India.
Ashok Kumar Rawat is the Chairperson of the Pediatric and Adolescent Nutrition Society, and Senior Technical Advisor with NCoE-SAM.
Arjan de Wagt is Chief of Nutrition with UNICEF India.
Key messages:
- A series of consultations in India between 2018 and 2021 has guided the adaptation of the MAMI Care Pathway Package (an integrated care model) to the Indian context, to strengthen policy provision and frontline care of infants under the age of six months with early growth failure.
- Adaptation has involved integrating key components within existing community and facility-based programmes.
- Further steps identified in a 2021 consultation on pilots in Maharashtra, Bihar and West Bengal include to increase coverage and utilisation of existing health and nutrition services; to strengthen community-level support during the first six months of life; to improve the counselling skills of frontline workers; to strengthen growth promotion activities; and to build the capacity of nutrition rehabilitation centres (NRCs).
Introduction
Small and nutritionally at-risk infants under the age of six months includes infants who are born too small or who become so in early life. In India, this is considered early growth failure (Box 1). Infants may be low birth weight (including premature), wasted, underweight and/or have growth or feeding difficulties. Infants may also be clinically unwell. In India, 27% of infants under the age of six months are wasted/acutely malnourished (weight-for-length (WLZ) <-2 and 13% severely wasted (WLZ <-3)), while 32% are underweight (weight-for-age (WAZ) <-2) and 10.6% are severely underweight (WAZ <-3) (Government of India, 2021). The prevalence of babies born with a low birth weight is very high (18%), and many of them are or become wasted. Only 41.8% of children are breastfed within the first hour of birth and only 63.7% of infants under the age of six months are exclusively breastfed (Randev, 2020).
A variety of programmes and platforms exist in India to identify and manage early growth failure (Kumar et al, 2020a) (Figure 1). However, the uptake of services tends to fall short of expectations. For example, only 58.1% of pregnant women have at least four antenatal check-ups and only 40% of children receive their health check-ups under the national Integrated Child Development Services (ICDS) programme (Government of India, 2021). Although India has done remarkably well in increasing the survival of high-risk newborns and infants by identifying and managing sickness within dedicated facilities and targeted programmes (Kumar et al, 2020b), community-based interventions that address infant and mother health and nutrition need further strengthening. Services for pregnant women centre on physical illness, with little support for maternal mental health (for example). Regional variations, poor service integration and gaps in referral systems further hinder the continuity of quality care. Practical constraints include poor availability of appropriate equipment (digital weighing scales and infantometers) and differing skill levels of community health workers. Furthermore, there remains a paucity of evidence and a lack of initiatives in India on how best to address the prevention, identification and management of acute malnutrition in children under six months of age (Chowdhury et al, 2021).
The MAMI Care Pathway Package, co-created by members of the MAMI Global Network,1 is a set of resources and materials to help practitioners identify, assess and manage small and nutritionally at-risk infants under six months of age and their mothers. It applies an integrated care pathway approach, modelled and building on integrated management of childhood illness and linking maternal and infant health and nutrition services, and requires contextualisation. While there are limitations, existing platforms in India offer rich potential for integrated management of early growth failure in India. This article shares experiences to maximise on these within existing services based on the adaptation of the MAMI Care Pathway Package to the Indian context.
Box 1: Criteria for early growth failure in infants under the age of six months
Any of the following criteria:
- Low birth weight
- Not regaining birth weight by day 14 of life
- Poor weight gain (<150g/week) after the second week of life
- Static weight or weight loss on two consecutive visits
- WAZ less than -2SD
- WLZ less than -2SD
Figure 1: Delivery platforms for care for infants under the age of six months with growth failure in India
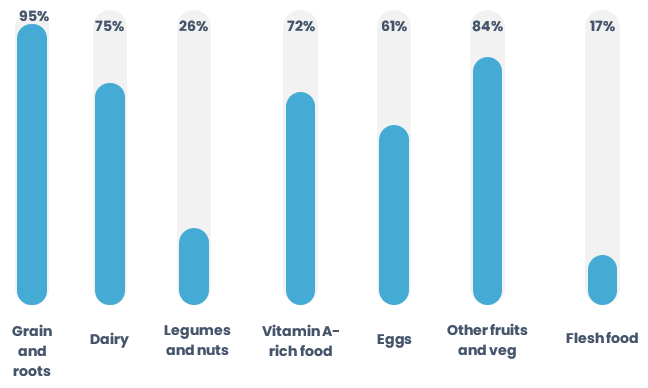
* MAA is a nationwide programme of the Ministry of Health and Family Welfare, Government of India, in an attempt to bring undiluted focus to the promotion of breastfeeding and to the provision of counselling services for supporting breastfeeding through health systems.
Policy development
To facilitate adaptation of the MAMI Care Pathway to the Indian context, policy makers, national and international experts, academia, and technical and development organisations were convened as part of three expert consultations2 guided by an expert panel.3 These consultations, which took place between 2018 and 2021, aimed to facilitate experience exchange and learning, to develop consensus and to identify next steps on how to leverage and maximise existing services for early growth failure management (Figure 2).
Figure 2: Timeline for the adaptation of the MAMI Care Pathway Package in India
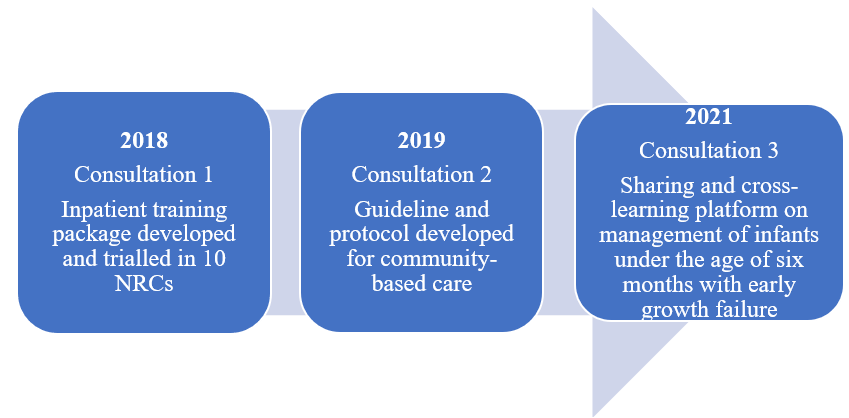
An inpatient care training package was developed following the 2018 consultation and piloted in 10 NRCs (Kumar et al, 2020a). As a result of the 2019 consultation, the National Centre of Excellence for Management of Severe Acute Malnutrition (NCoE-SAM) at Kalawati Saran Children’s Hospital led the development of a national guideline and protocol for the community-based management of early growth failure in infants under the age of six months, based on the MAMI Care Pathway Package. The MAMI Care Pathway Package was contextualised by integrating its different components into existing community-based programmes managed by the government-appointed community health workers (Figure 3). This national guideline was the reference for developing operational guidelines piloted in three states. A third national consultation was held in 2021 to discuss key developments and experiences to date and are summarised here.
Figure 3: Algorithm of an adapted MAMI Care Pathway in India
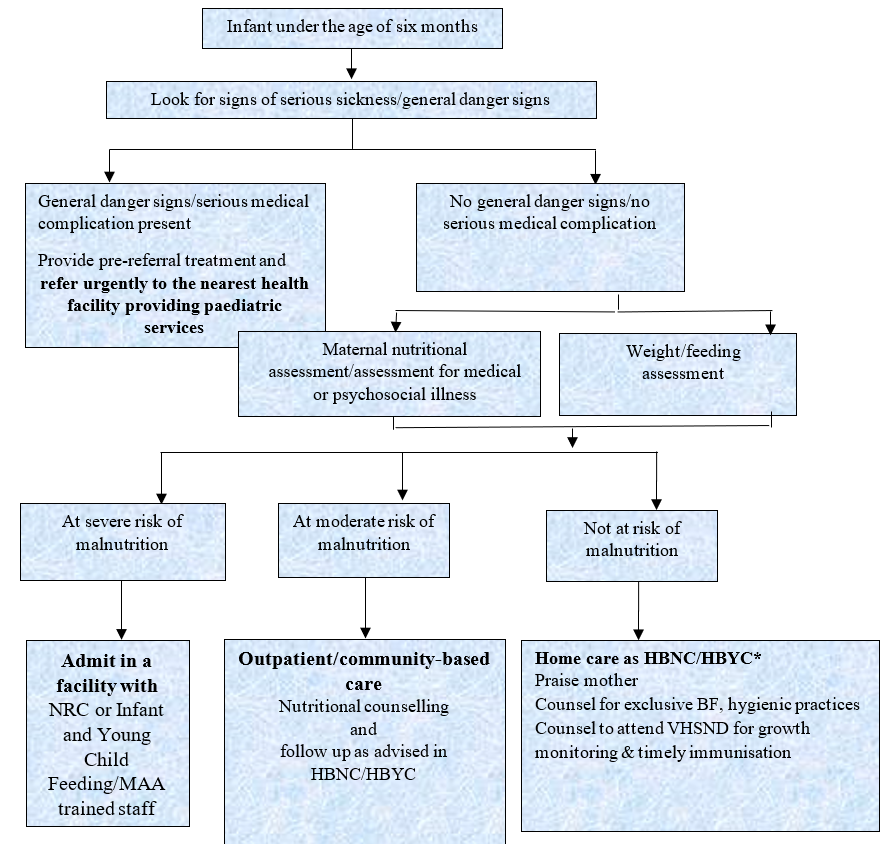
* Home-based newborn care (HBNC); home-based care for the young child (HBYC); village health, sanitation and nutrition days (VHSND)
National consultation 2021
The 2021 consultation focused on the burden of wasting and associated risk factors in infants under the age of six months. Experiences of adapting the MAMI Care Pathway Package to the Indian context from the states of Maharashtra, Bihar and West Bengal were shared. Key considerations that emerged for both facility-based and community-based management of infants under the age of six months with growth failure were discussed4 as follows.
Criteria for identification
The World Health Organization (WHO) (2013) recommends a WLZ z-score of <-3 or the presence of bilateral pitting oedema to identify severe wasting in infants under the age of six months. However, WAZ is increasingly being recognised as the best predictor of mortality among infants under the age of six months and is gaining more traction (Chowdhury et al, 2021). Monthly growth monitoring of children in India uses WAZ growth charts under the ICDS programme (Ramachandran & Gopalan, 2011) and could be further expanded as a way of identifying at-risk infants under the age of six months. Measuring the length of infants under the age of six months can be cumbersome, especially outside facilities, and length boards are not consistently available. While there is emerging evidence on the use of mid-upper arm circumference (MUAC) in this age group, more research is needed in the India context.
Using F-75 versus diluted F-100 for therapeutic purposes
Infants without prospects of breastfeeding are currently managed with F-75 or diluted F-100 in inpatient facilities. Experiences from Maharashtra using F-75 demonstrated good weight gain in infants admitted to tertiary care facilities. The use of F-75 has a practical advantage, as it avoids potential errors in preparing diluted feeds from F-100.
Growth charts used for identification of risk in low birth weight infants
Intergrowth 215 postnatal growth charts take account of gestational age and prematurity and therefore enable more accurate identification of growth faltering in low birth weight infants. WHO standard growth charts6 and Fenton growth charts (Fenton & Kim, 2013) do not account for prematurity or gestational age and may therefore overestimate the prevalence of growth problems in these infants. In India, more evidence is needed on the most appropriate and feasible growth chart for the identification of nutritional risk among low birth weight infants, noting that accurate gestational age is often not available.
Opportunities for further adaptations to existing services
The presentations from Maharashtra, Bihar and West Bengal raised the potential benefit of upgrading the community-based individual cards – prompt cards for health professionals to use during consultations – to include additional content. Potential additions include:
- Maternal anthropometry (weight and MUAC) during home visits
- Feeding assessments
- Breast examination of mothers to assess sore/engorged nipples or suspected mastitis
- Observation of breastfeeding with respect to positioning, attachment and effective suckling
- Maternal mental health assessment
- Inclusion of the Integrated Management of Neonatal and Childhood Illness 0–2 months protocol
- Kangaroo Mother Care
- Documenting if the infant is referred to another service and the reason for referral
Importance of sensory stimulation and play therapy
The panellists discussed how sensory stimulation and play therapy should be a part of the routine management of at-risk infants under the age of six months, as they have led to improvements in various domains of development including motor, language, cognitive, social-emotional and self-help development – as highlighted in Field Exchange issue 68 (Kamble et al, 2022).
The presentations and panel discussion from the third consultation concluded with some consensus on guiding principles and next steps that have the potential to strengthen the care of infants under the age of six months with early growth failure.
Increase coverage and utilisation of services
Leveraging existing health and nutrition services for infants and children and for pregnant and lactating women is integral to increasing coverage and service utilisation. Efforts should be made to enhance convergence between different government departments to establish linkages between existing services for infants and children and services for pregnant and lactating women. This will enable a continuum of care so that mothers and infants receive the entire package of services from pregnancy through six months of age, rather than fragmented service provision. The framework and guidance from the MAMI Care Pathway Package can help identify useful linkages across facility-based and community-based service providers. Further, a more targeted approach to reach the most vulnerable and underserved populations, especially those residing in hard-to-reach areas or in predominantly tribal areas, would be valuable.
Strengthen support in the first six months of life
A high-quality, comprehensive, community-based package of care for at-risk infants in the first six months of life and their mothers is needed in India. This needs to include lactation support, improved growth monitoring coverage, nutritional classification (severe/moderate/not at risk), medical assessment, appropriate action and referral services.
Enhance the counselling skills of frontline workers
There is an urgent need to enhance the counselling skills of frontline workers, especially on skilled lactational management and in the provision of psychological support to mothers. Counselling sessions should be conducted using appropriate counselling aids and job aids (although these exist, translation into local languages is needed). Knowledge and skills of community health workers can be improved through continuous training and supervision. Counselling materials should be made available to all community health workers.
Develop growth monitoring and promotion (GMP) activities
There is potential to further develop GMP activities. Currently, GMP is institutionalised through ICDS and mostly conducted as a standalone activity. GMP activities can be strengthened and connected to other services by ensuring the availability of functional equipment at all health points; by improving the knowledge and skills of community health workers to take correct anthropometric measurements and correctly classify nutritional status; by ensuring the use of ‘Mother and Child Protection’ cards for growth monitoring by community health workers; by enhancing the involvement of community members in GMP activities; by conducting children’s medical assessments; and by creating linkages with referral services based on their nutritional and medical assessments. In many places, ‘Accredited Social Health Activist’ kits7 are often unavailable. Strengthened supply chain mechanisms for timely supply of commodities and equipment and improved data quality and data completion are also critical for quality care.
Build capacity of NRCs
Lastly, there is a need to build the capacity of NRCs to manage high-risk infants under the age of six months with early growth failure, especially if they have co-morbidities. Resident doctors and other medical staff should be sensitised on the management of these cases and on how such case management differs from that of older children.
Conclusion
In India, early growth failure in its various forms is most prevalent among infants under six months of age and is associated with higher risks of morbidity and mortality. Early identification and intervention is therefore critical. Most cases can be treated at outpatient/community level. Experiences from three states in India reflect both progress and the potential to apply the MAMI Care Pathway approach to the Indian context by
strengthening and connecting existing community and facility-based programmes, as well as by implementing the recommendations made during the consultation. India is on a pathway towards a scalable approach to continuity of care.
For more information, please contact Praveen Kumar at pkpaed@gmail.com.
References
Choudhary T, Srivastava A, Chowdhury R et al (2019) Severe wasting among Indian infants <6 months: Findings from the National Family Health Survey 4. Maternal & Child Nutrition, 15, 4, e12866.
Chowdhury R, Nitika, Choudhary T et al (2021) Diagnostic measures for severe acute malnutrition in Indian infants under 6 months of age: A secondary data analysis. BMC Pediatrics, 21, 158.
ENN, LSHTM & collaborators (2021) MAMI Care Pathway Package, Version 3 (2021). www.ennonline.net/mamicarepathway
Fenton T & Kim J (2013) A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatrics, 13, 59.
Government of India (2021) National Family Health Survey (NFHS-5) 2019–2021. Ministry of Health and Family Welfare. http://rchiips.org/nfhs/factsheet_NFHS-5.shtml
Kamble N, Mathur R, Gavali V et al (2022) Sensory stimulation and play therapy: Benefits in the treatment of severe wasting in India? Field Exchange, 68, November, 10. www.ennonline.net/sensorystimulationandplaytherapycombatseverewastinginindia
Kumar P, Deb S, de Wagt A et al (2020a) Managing at risk mothers and infants under six months in India – No time to waste. Field Exchange, 63. https://www.ennonline.net/fex/63/mamiindia
Kumar P, Meiyappan Y, Rogers E et al (2020b) Outcomes of hospitalized infants aged one to six months in relation to different anthropometric indices – An observational cohort study. The Indian Journal of Pediatrics, 87, 9, 699–705.
Ramachandran P & Gopalan H (2011) Assessment of nutritional status in Indian preschool children using WHO growth standards. Indian Journal of Medical Research, 134, 1, 47–53.
Randev S (2020) Malnutrition in infants under 6 months: Is it time to change recommendations? The Indian Journal of Pediatrics, 87, 9, 684–685.
World Health Organization (2013) Guideline: Updates on the Management of Severe Acute Malnutrition in Infants and Children. https://www.who.int/publications/i/item/9789241506328
1 https://www.ennonline.net/ourwork/research/mami.
2 National Consultation of Addressing Acute Malnutrition: http://coesamnetwork.org/Reports.aspx?flag=4.
3 The expert panel comprised Dr Satinder Aneja, Professor and Head, Department of Pediatrics, Sharda University; Dr Ashok Kumar Rawat, Chairperson of the Pediatric and Adolescent Nutrition Society and Senior Technical Advisor, NCoE-SAM, KSCH, New Delhi; Dr Ritu Rana, Assistant Professor, IIPHG, Gujarat; and Marie McGrath, Technical Director, Emergency Nutrition Network, MAMI Global Network Co-chair, United Kingdom.
4 Inpatient care was also discussed, but is not elaborated on in this article.
7 Under the National Health Mission, each Accredited Social Health Activist is provided with two kits: 1) a drug kit, which mainly contains drugs for minor ailments, and 2) an equipment kit, which contains a weighing scale, digital watch, thermometer, communication materials, etc.


