The cost of delivering severe wasting treatment in East Nusa Tenggara, Indonesia
Lani Trenouth is a former consultant with the UNICEF Regional Office for South Asia
Blandina Rosalina Bait is a Nutrition Specialist with UNICEF Indonesia
Markus Harmiko is a former Nutrition Officer with UNICEF Indonesia
Julia Suryantan is a Nutrition Officer with UNICEF Indonesia
Sidayu Ariteja is a Planner at the Ministry of National Development Planning, Indonesia
Nida Rohmawati is the Chief Coordinator of the Task Force for Under Five and Preschool Children at the Ministry of Health, Indonesia
Ruth Laiskodat is the Head of Provincial Health Office, East Nusa Tenggara, Indonesia
The authors wish to thank the Indonesian Ministry of Health (MoH), the Ministry of National Development Planning (Bappenas), and the East Nusa Tenggara (NTT) Province, the Kupang District and the Kupang Municipality Health Offices for their support and valuable input into this costing exercise. We also thank Jee Hyun Rah (UNICEF Indonesia) and Mueni Mutunga (UNICEF East Asia and Pacific (EAPRO)) for their technical advice, and Hai Ragalawa, Astryd Maranda and Ida Liem (UNICEF Field Office Kupang) for supporting data collection. Special thanks also to Aminuddin Ramdan, Andi Yoga Tama, Arie Rukmantara, Henky Widjaya and Yudhistira Yewangoe (UNICEF Indonesia Field Offices) for their feedback on the study findings.
Key messages:
- This article outlines the first costing exercise of the integrated management of acute malnutrition (IMAM) programme in East Nusa Tenggara (NTT) province, Indonesia.
- It was estimated that USD4.8 million would be required annually to achieve the Government of Indonesia (GoI)’s 2024 targets of 90% treatment coverage in 60% of all primary healthcare centres in the province.
- Models also indicated that improving treatment coverage may dramatically increase the cost-efficiency of IMAM services, suggesting that scale-up efforts should prioritise increasing coverage in high-burden areas.
Background
In Indonesia, over two million children under the age of five are severely wasted – the fourth-highest burden in the world. GoI has committed to reducing the prevalence of child wasting from 10% to under 7% by 2024. In 2021, a Presidential Decree on child stunting was issued, setting an ambitious target to provide treatment to 90% of severely wasted children by 2024. To achieve this, the Ministry of Health (MoH) plans to ensure that at least 60% of all primary healthcare centres (puskesmas) provide IMAM services by 2024.
IMAM programming was initiated in all 34 provinces of Indonesia by June 2021, yet the number of outpatient facilities offering IMAM services remains limited. Lack of evidence on cost, cost-efficiency and cost-effectiveness is a key barrier to resource allocation for scaling up IMAM services, and therefore of improved treatment coverage. To support GoI in evidence-based resource allocation and implementation planning, UNICEF carried out a costing exercise using IMAM data collected from Kupang Municipality and Kupang District in NTT province in 2021. The IMAM programme was first introduced in Kupang District in 2015 and was replicated by Kupang Municipality in 2018.
The goal of this costing exercise was to estimate the cost and cost-efficiency1 of the IMAM programme (measured as the cost per child admitted for treatment of severe wasting) and to estimate the financial resources required to progressively achieve GoI’s coverage target for IMAM services.
The costing approach
Data on resource usage were collected from Kupang District and Kupang Municipality according to the national prevention and treatment of child wasting guidelines (MoH, 2019). This included data relevant to the cost of community mobilisation, to outpatient treatment for uncomplicated cases and inpatient treatment for complicated cases, and to infants below the age of six months, as well as costs for overall programme management and oversight.
Since this analysis was conducted from the government perspective, all costs carried by implementing institutions were included. Any costs to child caregivers were outside the scope of analysis. Primary and secondary data were collected through document review and key informant interviews, with most interviews conducted by telephone due to COVID-19-related restrictions.
The analysis used a bottom-up ‘ingredients approach’ whereby the resources used to implement the IMAM programme (the ‘ingredients’) were identified, the required number or volume of each resource was estimated and the unit cost of each resource was determined. The total cost of the IMAM programme at a given scale was then estimated by multiplying the total volume of resources required by the unit cost of each resource. For example, the total cost of treatment (personnel time per child) was calculated by multiplying the average time spent with a child at the outpatient care site by the cost of personnel time based on standard salary grids provided by the MoH.
A modified version of the Food and Nutrition Technical Assistance (FANTA) community-based management of acute malnutrition (CMAM) costing tool (FANTA, 2012) was used to categorise the resources (Table 1), as well as to guide data analysis.
Table 1. Resources required for community-based management of child wasting
|
Cost category* |
Resources |
|
Treatment supplies (medical) |
Medicines for infection treatment; diarrhoea; deworming; malaria; vitamin A supplementation; measles vaccinations; routine tests; intravenous kits; nasogastric tubes |
|
Treatment supplies (other) |
Ready-to-use therapeutic food (RUTF) therapeutic milk (F-75, F-100); non-consumable clinic supplies (scales; height boards; job aids; stationery; food preparation supplies; etc.) |
|
Supply logistics |
Transportation and warehousing for therapeutic food and treatment medicines (including fuel; loading/offloading; driver per diems; warehouse rental and maintenance; salaries and benefits of drivers and guards; etc.) |
|
Community outreach |
Salaries and benefits of outreach personnel or incentives for community workers/volunteers |
|
Training |
Time of trainees; venue hire; refreshments; trainer fees; per diems; transportation; accommodation; training materials |
|
Supervision |
Salaries and benefits of supervision personnel; transportation for supervision visits |
|
Treatment personnel |
Salaries and benefits of technical personnel at the treatment clinic |
|
Management |
Salaries and benefits of managerial personnel |
|
Intermediate and central level |
Training (time of trainees; venue hire; refreshments; trainer fees; per diems; transportation; accommodation; training materials); supply logistics (transportation and warehousing for therapeutic food and treatment medicines including fuel; loading/offloading; driver per diems; warehouse rental and maintenance; salaries and benefits of drivers and guards; etc.); salaries and benefits of managerial personnel |
* Categories were informed by the FANTA CMAM costing tool (FANTA, 2012)
The volume of resources used to implement each component of IMAM was estimated for a given year using 2019 as a reference, as service delivery was dramatically reduced during the peak of the COVID-19 pandemic.2 Costs were collected in Indonesian rupiah and converted to US dollars at an average exchange rate for 2021. No adjustment for inflation was made due to the one-year timeframe. The annual usage cost of capital items3 by inpatient and outpatient clinics was calculated based on the assumption that each item would be replaced every three to five years.
To ensure a high quality of analysis, any unexpected or atypical results were discussed within the costing team and data errors were identified and rectified. Uncertainty in the total costs required was handled by estimating a ‘most likely cost’ scenario, as well as plausible ‘low-cost’ and ‘high-cost’ scenarios. For example, the average total time spent by outpatient treatment personnel with each child was an estimated average of 53 minutes per child per visit to the care site. This was used to inform the ‘most likely cost scenario’. However, according to key informant interviewees, personnel time spent per child ranged between 24 minutes per visit (the ‘low-cost’ scenario) and 72 minutes per visit (the ‘high-cost’ scenario).
Findings
A total of 297 children were admitted for wasting treatment in Kupang District and Kupang Municipality, of whom 72 were admitted initially to inpatient care before being discharged to outpatient care to continue treatment. Inpatient care was provided in three hospitals, outpatient care was provided in 21 puskesmas and community outreach was conducted in 647 posyandu (community health posts). Inpatient care lasted an average of seven days for children aged 6–59 months, and 21 days for children below the age of six months. Outpatient care lasted an average of six weeks, with weekly follow-up visits. Outcome data from the inpatient care sites were unavailable, so for the purposes of estimating costs we assumed that 100% of children admitted were discharged to outpatient facilities and were not lost to follow-up. We also assumed that there was no defaulting during outpatient care.4 Data indicated that, on average, 14.6 kg of RUTF was used per child in outpatient care.
The aggregate staff time required in the outpatient care sites to care for all admitted children totalled 0.60 full-time equivalent (FTE)5 in Kupang Municipality and 0.68 FTE in Kupang District. Each admitted child received, on average, the equivalent of 1.1 days of aggregate staff time over the course of six weeks of treatment, or 1.5 hours at each clinic visit.
In the inpatient care sites, the aggregate staff time was 0.28 FTE in Kupang Municipality and 0.36 FTE in Kupang District. Each admitted child received an average of 1.9 days of aggregate staff time over 7–21 days while in care, or approximately 1.2 hours per day.
Cost-efficiency
The total cost of providing IMAM services for one year was estimated at USD96,725, with a low-cost estimate of USD71,350 and a high-cost estimate of USD135,171. The total cost was divided by the number of children admitted for treatment (N = 297) to derive a cost-efficiency estimate of USD326 per child admitted for treatment of severe wasting, with a low-cost estimate of USD240 per child and a high-cost estimate of USD455 per child. These are comparable to cost-efficiency results in other published studies (Chui et al, 2020).
Cost drivers
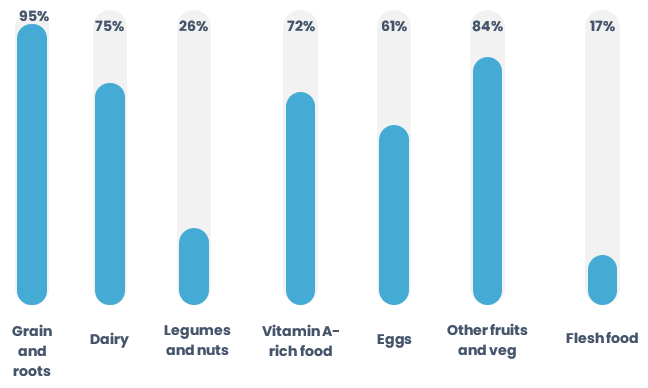
Personnel costs to conduct community outreach and screening was the largest driver (28%) of the overall cost of the IMAM programme, followed by the cost of RUTF (13%) and outpatient site supply logistics related to RUTF transportation and storage (8%) (Figure 1). Costs such as community outreach personnel, supervision or training were fixed based on the number of care sites, while costs such as RUTF and treatment personnel varied based on the number of children treated. With an increase in treatment coverage, variable costs will make up a larger proportion of the total, while fixed costs will decrease as a proportion of the total.
Figure 1. Top 10 cost drivers of delivering the IMAM programme
Cost modelling
To estimate the changes in costs relative to the scale-up of treatment services, a series of treatment coverage and geographic coverage scenarios were modelled, both independently and in conjunction with one another. Cost projections were conducted by identifying the cost categories that would vary with the caseload (such as RUTF or treatment staff time) and categories that would vary with the number of care sites (such as non-consumable clinic supplies or middle management supervision time).
Treatment coverage was calculated based on the total number of children admitted for treatment of severe wasting at the care sites in Kupang District and Kupang Municipality (N = 297), and as a percentage of the estimated district burden using reported prevalence of severe wasting in children under the age of five during the reference period (N = 9,357) (Isanaka et al., 2016; Laporan Nasional Riskedas, 2018). Geographic coverage of the IMAM programme was estimated at 13% based on the number of posyandu providing IMAM services (N = 647), divided by the total number of posyandu (N = 5,136).6 The modelled coverage percentages were based on the MoH progressive targets for IMAM services through to 2024 (MoH, 2020). At the time of analysis, the estimated IMAM treatment coverage was 3.2%.
The annual cost of achieving GoI’s 2024 targets of 90% treatment coverage in 60% of all puskesmas in NTT province was estimated at USD4.8 million (Table 2). To achieve global treatment coverage averages of 40% and geographic coverage of 43% (Rogers et al, 2015; UNICEF et al, 2012), an estimated USD1.8 million will be required. The projections from this costing exercise highlight that greater cost-efficiency (i.e., cost per child treated) could be achieved through improving treatment coverage within selected high-burden districts, rather than by increasing geographic coverage without improved treatment coverage.
Table 2: Cost and cost-efficiency projections based on treatment coverage and geographic coverage for NTT province*
|
|
|
Treatment coverage (of total burden) |
|||
|
|
|
3.2% |
20% |
40% |
90% |
|
Geographic coverage |
13% |
USD97,000 total USD326 per child |
USD264,000 total USD141 per child |
USD462,000 total USD124 per child |
USD959,000 total USD120 per child |
|
30% |
USD302,000 total USD411 per child |
USD715,000 total USD155 per child |
USD1,206,000 total USD130 per child |
USD2,433,000 total USD125 per child |
|
|
45% |
USD452,000 total USD410 per child |
USD1,071,000 total USD154 per child |
USD1,807,000 USD130 per child |
USD3,648,000 total USD125 per child |
|
|
60% |
USD601,000 total USD409 per child |
USD1,386,000 total USD150 per child |
USD2,368,000 total USD128 per child |
USD4,822,000 total USD124 per child |
|
* Cost estimates are rounded to the nearest USD1,000.
Discussion
To our knowledge, this is the first published costing study of IMAM in Indonesia. Given contextual and epidemiological variations in severe wasting across Indonesia – which comprises 17,000 islands – additional costing exercises in other provinces are necessary to better estimate national-level investment requirements. One of the main limitations of this study was that IMAM treatment has not yet reached maturity in Indonesia and, as such, the levels of treatment and geographic coverage were relatively low at the time of the investigation. However, this exercise provides valuable insight into the financial resources required to scale up IMAM services and achieve the GoI targets by 2024. The total GoI budget allocation for nutrition services in 2022, including the treatment and prevention of child wasting, was USD2.95 billion. Approximately 3% of children affected by severe wasting in Indonesia are found in NTT. Approximately 0.16% of the national budget for nutrition-specific and sensitive interventions would be required for the province to achieve 90% coverage.
While the average cost per child admitted for treatment of severe wasting (USD326) was similar to that found by other studies (Chui et al, 2020), comparison of costs across studies and contexts is hampered by a lack of transparency in terms of analytical choices made, particularly regarding included versus excluded costs and how to factor in joint costs. In this exercise, the formal structure and transparency of the methods using the FANTA CMAM costing tool allow for replication. The analytical choices and adjustments made to the calculations can also be traced by following the data entered into the tool, alongside the formulas used.
It was beyond the scope of this study to investigate the preferences of, or potential cost savings to, child caregivers. However, other studies have demonstrated the benefits of improved access to outpatient care for uncomplicated cases of severe wasting, including lower default rates and better recovery rates (Puett et al, 2013).
Findings from this exercise have also shown that the cost-efficiency of IMAM services increases as treatment coverage improves. This suggests that scale-up efforts should prioritise increasing treatment coverage in high-burden areas. Potential options for improving the cost-efficiency of IMAM interventions could be explored, such as ‘simplified approaches’7 to treating child wasting, particularly focusing on reducing RUTF dosage.
Future analysis could include an estimate of the cost of not treating children with wasting, the number of lives saved or the disability-adjusted life years averted. This would capture wider benefits of scaling up and improving the quality of IMAM services in Indonesia.
For more information, please contact Blandina Rosalina Bait at bbait@unicef.org
References
Chui J, Donnelly A, Cichon B et al (2020) The cost-efficiency and cost-effectiveness of the management of wasting in children: A review of the evidence, approaches, and lessons.
FANTA (2012) Food and Nutrition Technical Assistance (FANTA) Community-Based Management of Acute Malnutrition (CMAM) costing tool. https://www.fantaproject.org/tools/cmam-costing-tool
Government of Indonesia Ministry of Health (MoH) (2019) Guideline of Prevention and Treatment of Severe Wasted Children. http://appx.alus.co/direktoratgiziweb/katalog/pedoman-pencegahan-dan-tatalaksana-gizi-buruk-pada-balita-final-03.pdf
Government of Indonesia Ministry of Health (MoH) (2020) Ministry of Health Strategic Plan 2020–2024, p21.
Isanaka S, O’Neal Boundy E, Grais R et al (2016) Improving estimates of numbers of children with severe acute malnutrition using cohort and survey data. American Journal of Epidemiology, 184, 12.
Laporan Nasional Riskedas (2018) Laporan Nasional Riskedas. http://repository.litbang.kemkes.go.id/3514/
Puett C, Sadler K, Alderman H et al (2013) Cost-effectiveness of the community-based management of severe acute malnutrition by community health workers in southern Bangladesh. Health Policy and Planning, 28, 4. https://academic.oup.com/heapol/article/28/4/386/966295
Rogers E, Myatt M, Woodhead S et al (2015) Coverage of community-based management of severe acute malnutrition programmes in twenty-one countries, 2012–2013. PLoS One, 10, 6, e0128666.
UNICEF, Coverage Monitoring Network, and Action Against Hunger (2012) The State of Global SAM Management Coverage 2012. New York and London.
1 It was not possible to assess the cost-effectiveness (e.g., cost per child recovered from severe wasting) of the IMAM programme due to insufficient data on treatment outcomes.
2 In instances where there was insufficient quality primary or secondary data available on resource requirements, we relied on expert assumptions or norms built into the FANTA CMAM costing tool.
3 Capital items are durable goods with a life use spanning more than one year, such as vehicles, buildings, computers, refrigerators, etc. It is common in cost analyses to include the value of the actual time spent using the capital goods, not the full cost.
4 There were no empirical data that could be used to plausibly estimate potential loss or default rates. This is a limitation of the study.
5 One FTE is the working time of one person employed full time, assuming a working day is eight hours and there are 260 working days per year.
6 Note that, for the scale-up projections, geographic coverage refers to the provision of care at posyandu and puskesmas levels. For the base case calculations, the geographic coverage was estimated at 13% at posyandu level and 5% at puskesmas level.


