How best to predict child mortality using different anthropometric indices?
This is a summary of the following article: Briend A, Myatt M, Berkley JA et al (2023) Prognostic value of different anthropometric indices over different measurement intervals to predict mortality in 6–59-month-old children. Public Health Nutrition, 1–12. Advance online publication. https://doi.org/10.1017/S1368980023000149
This pooled analysis of 12 prospective studies compared the prognostic value of mid-upper arm circumference (MUAC), weight-for-height Z-score (WHZ) and weight-for-age Z-score (WAZ) for predicting death in children aged 6–59 months. Sensitivity (the proportion of children below the threshold of case definition who died during follow-up) and false positive (children below the threshold of case definition who survived) ratios to predict death – within one, three and six months after the anthropometric measurement was made – were compared for the three individual anthropometric indices and their combinations. The analysis utilised community-based, prospective studies from 12 countries across Africa and Asia.
Sensitivity was higher for death within one month of follow-up as compared to follow-up at six months, by 49% for MUAC < 115 mm (P < 0.001), 48% for WHZ < -3 (P < 0.01) and 28% for WAZ < -3 (P < 0.005). This was accompanied by an increase in false positives of only 3% or less. Frequent anthropometric measurements therefore significantly improved the identification of malnourished children with a high risk of death without markedly increasing false positives.
Combining indices resulted in an increase in sensitivity, but also in false positives, among children meeting case definitions. The Venn diagram (Figure 1) shows the number of children who died within one month of assessment with at least one severe anthropometric deficit detected with WAZ < -3, WHZ < -3 and MUAC < 115 mm (a), and also with MUAC < 120 mm (b) and MUAC < 125 mm (c). WAZ < -3 was the most sensitive criterion, as it identified a total of 51 children among those with severe anthropometric deficits at assessment who subsequently died (n 170). MUAC < 115 mm identified 33 children, and WHZ < -3 identified 20.
Figure 1: Venn diagram showing the overlap of children identified by different anthropometric indices among children who died within one month of nutritional assessment
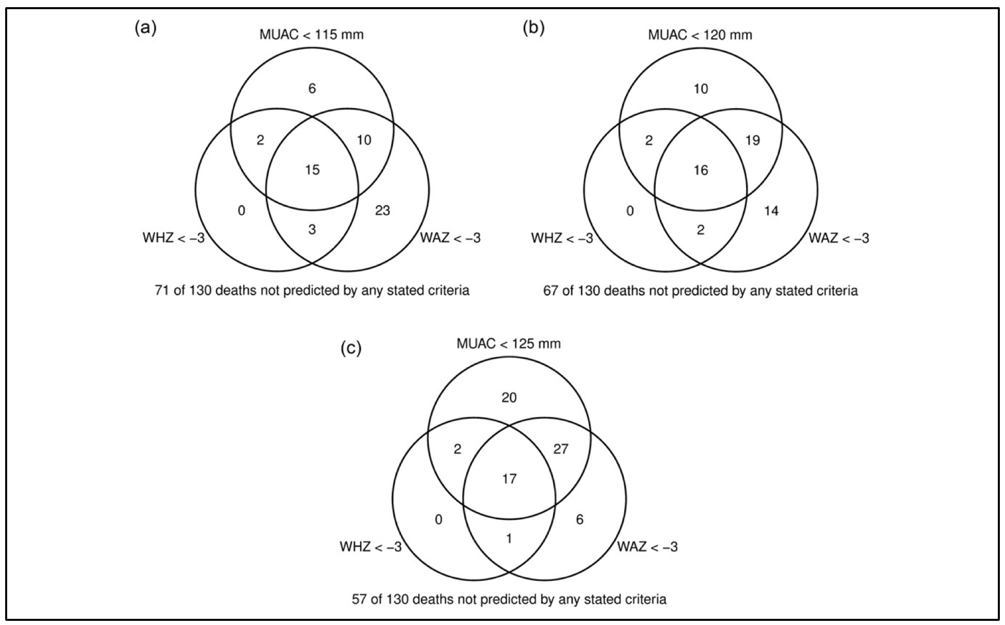
(a) MUAC < 115 mm. (b) MUAC < 120 mm. (c) MUAC < 125 mm.
This study showed that, even when used frequently, the combination of MUAC < 115 mm and WHZ < -3 failed to identify quite a few children with WAZ < -3 who died during follow-up. Some children with WAZ < -3 who died during follow-up were also missed when the MUAC cut-off was increased to 120 mm, and even to 125 mm. No child who died during follow-up was identified by WHZ < -3 when MUAC < 115 mm or WAZ < -3 were used as the selection criterion. This suggests that the combination of WAZ < -3 and MUAC < 115 mm would eliminate the need for the use of WHZ.
Increasing MUAC cut-off as the sole criterion for admission – as is commonly the case with simplified protocols – increased the number of detected deaths, but also increased the proportions of false positives.
The authors also found that, for identifying high-risk children, there was a greater and more important overlap between the MUAC and WHZ indices than suggested by population surveys and analyses of programme data. Concerns about missing many high-risk children when using MUAC < 115 mm alone seem to be less relevant for monthly screening than for longer intervals between screenings.
In conclusion, the prognostic value of different anthropometric indices to predict death decreases over time. To optimise the detection of high-risk children, monthly screening is preferable where resources allow. Increasing the proportion of detected high-risk children who would die in the absence of treatment can also be achieved by using several indices simultaneously. The most sensitive scheme is MUAC combined with WAZ. The addition of WHZ does not capture any additional children with a high risk of death when compared to the combination of MUAC < 115 mm and WAZ < -3. However, combining MUAC and WAZ results in an increase in false positives – that is, of children who will survive in the absence of treatment – as compared with using MUAC only, with important implications in terms of the number of children treated and the consequent programme costs.


