Coordination of a nutrition response in a conflict situation: Learnings from northern Ethiopia
Lisez cet article en français ici
Nakai Munikwa is a Nutrition Information Management Specialist for the Nutrition Cluster in Tigray, Ethiopia.
Kirathi Mungai is a Nutrition Cluster Coordinator in Tigray, Ethiopia.
Leela Zaizay is a Nutrition Specialist at UNICEF Tigray, Ethiopia.
Ines Lezama is a Nutrition Cluster Coordinator / Emergency Nutrition Coordination Unit (ENCU) Team Lead in Addis Ababa, Ethiopia.
Rashid Abdulai is a Nutrition Specialist at UNICEF Ethiopia.
Stanley Chitekwe is a Chief of Nutrition at UNICEF Ethiopia.
The authors would like to thank Daiana Albino Pena, Mikiale Abraha, Desalegn Yazew, Frezer Dulume, Ramadhani Noor, Ifeanyi Maduanusi, Anne-Sophie Donze, and Abiy Tefera from UNICEF in Ethiopia for their contribution to this work. The support of Faith Nzioka, Marie Cusick, and Rachel Lozano, from the Global Nutrition Cluster, is also greatly appreciated.
What we know: The nutrition response in the northern Ethiopia conflict – Afar, Amhara, and Tigray regions – was especially complex. It involved facing challenges that required nutrition partners to depend on each other’s technical and core capacities and to work collaboratively to reach those most in need.
What this adds: This article explores these challenges and highlights lessons learned in the design, coordination, and scale-up of the nutrition response as the situation evolved. Localisation of the response was instrumental in increasing the coverage of nutrition services.
Background
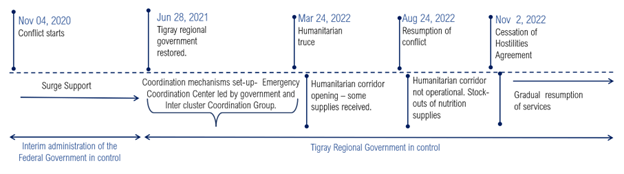
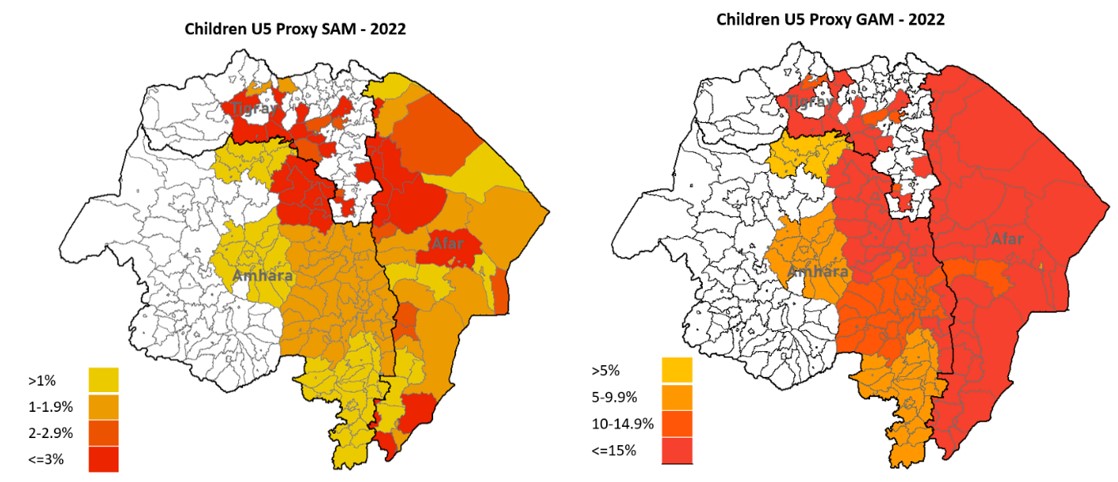
When the conflict started in Tigray in November 2020 (Figure 1) and then spread to the neighbouring regions of Afar and Amhara, it caused mass displacement, loss of livelihoods, compromised access to food, and disruption to health, water, and sanitation facilities. These problems were compounded by drought and flooding that occurred in some areas, all of which resulted in disruption of basic services and, ultimately, loss of life. Prior to the conflict breaking out in northern Ethiopia, the prevalences of global acute malnutrition (GAM)1 in Afar, Amhara, and Tigray regions were already above the national average (7.0%) at 13.9%, 7.6%, and 9.1% respectively (Ethiopian Public Health Institute and ICF, 2021). The nutrition response implementation was led by the Disaster Risk Management Commission (EDRMC) in government, with ENCU at the federal level coordinating the nutrition response using a hybrid coordination approach – led by both UNICEF and the government. The focus of the overall nutrition intervention was on reducing wasting and stunting levels, as well as strengthening systems for the delivery of nutrition services. There were few humanitarian partners at the time.
In June 2021, when Tigray became the epicentre of the conflict and the number of humanitarian partners increased, the humanitarian coordination team activated a subnational cluster coordination mechanism in Tigray.
As the emergency became protracted, humanitarian needs grew. Forecasts indicated that at least 1.3 million children would suffer from wasting in northern Ethiopia in 2022, growing to 1.5 million children in 2023. It was also estimated that 400,000 children would develop severe wasting, putting them at increased risk of disease and death (Office for the Coordination of Humanitarian Affairs (OCHA), 2022a).
While the conflict ended in November 2022, the social, structural, and systematic issues it has caused in the health system entail continued challenges in the delivery of nutrition services.
This article covers how the various challenges were addressed in the design, coordination, and scale-up of the nutrition response, as well as what useful lessons we can share with others who may need to set up similar emergency nutrition responses.
Figure 1: Timeline of the humanitarian response
A challenging response
Developing a comprehensive package of care
As part of the humanitarian response, the Nutrition Cluster aimed to deliver a comprehensive package of essential nutrition services to women and children affected by the emergency. These services were guided by the Ethiopia national guideline for management of wasting (Federal Ministry of Health, 2019) and coordinated by the federal ENCU. As the coordination unit of the Government of Ethiopia, the ENCU led the process of formulating the emergency response package in the three regions of Amhara, Afar, and Tigray in collaboration with United Nations agencies, donors, international non-government organisations (NGOs), and local partners.
UNICEF and its partners supported the implementation of, and supply chains for, the therapeutic feeding programme (screening and treatment of severe wasting cases), micronutrient supplementation and deworming, and the promotion of maternal, infant, and young child feeding. An emergency food ration (BP-5) – a compact, high-calorie, vitamin fortified, dry biscuit – was also provided temporarily to displaced people until the longer-term/comprehensive nutrition intervention became operational.
Considering the high prevalence of malnutrition, a blanket supplementary feeding programme would have been advised. However, the logistics and cost would have been excessive to cover the needs. The decision was made to target individuals most in need and the World Food Programme (WFP) and its partners coordinated targeted supplementary feeding programmes. Through its partners, WFP provided children under five with moderate wasting and pregnant and lactating women with wasting monthly rations of ready-to-use supplementary foods and fortified flours.2
The World Health Organization (WHO) provided technical support and medical supplies to manage undernourished children who were admitted to stabilisation centres whilst UNICEF provided therapeutic milk.
Rationalisation of service provision – focus on Tigray region
In Tigray, partners responded to immediate needs – including to displaced populations in camps – but there was a lack of coordination. A joint Northern Ethiopia Strategic Response Plan was developed in May 2021 with the formalisation of the cluster in Tigray (OCHA, 2021). By August 2022, led by the Nutrition Cluster, a review of the overall nutrition response was conducted. The review revealed that the nutrition service delivery package was not uniformly implemented and varied from partner to partner. The presence of partners was not aligned with the needs and the continuum of care was suboptimal. In some areas, there was duplication of efforts; in others, there were gaps. The decline in service availability and the functionality of health facilities and nutrition sites was further compounded by non-payment of health workers’ salaries since the start of the conflict.
The Tigray Nutrition Cluster and ENCU at federal level requested support from the Global Nutrition Cluster to develop the joint nutrition cluster operational response plan. The plan was completed in November 2022, and it laid out the activities and tasks that Nutrition Cluster partners had to carry out to scale up comprehensive nutrition interventions and improve the nutrition outcomes (GNC, 2022a). A clear package of comprehensive nutrition actions was defined (GNC, 2022b), guided by the Ethiopian national guidelines for management of wasting and UNICEF core corporate commitments for nutrition in emergencies, which highlighted the activities for partners (Box 1). A workshop with all partners was held to familiarise each partner with the operational plan and the core nutrition actions and strategies to use in the health systems strengthening approach before 2023.
Box 1: Components of the comprehensive nutrition actions package in the Tigray nutrition response
|
The Nutrition Cluster consulted with the local government and with nutrition partners to rationalise the partners’ presence. With the identification of a single partner that would cover a woreda (district), the objective was to ensure full coverage of nutrition activities in all woredas with partners integrating activities from other sectors in their response area. This would leverage technical and financial resources and improve efficiency and effectiveness.
The Nutrition Cluster recommended that UNICEF and WFP create partnerships with the implementing partners that had been mapped. By January 2023, most woredas (70 out of 79 – 89%) had the same partner for the targeted supplementary feeding and therapeutic feeding programmes.
Achievements and challenges
Strengthening multisectoral efforts
The nutrition emergency response in northern Ethiopia relied on the implementation of a multisectoral action that had three fundamental components: working in partnership with local and international NGOs, working through mobile health and nutrition teams (MHNTs), and initiating the ‘find and treat campaigns’.
Partnership with local and international NGOs
The response purposefully leveraged partners’ geographical convergence, especially those also responding in food security; health; water, sanitation and hygiene; and protection in the same woreda. UNICEF and WFP strengthened this process by engaging the same partners for such activities. Consultations were further done with other clusters and advocacy with donors for multisectoral projects and partner selection based on partners’ ability to implement in more than one sector.
Mobile health and nutrition teams
Within the rollout of improved access to primary health care, nutrition and health activities were integrated through the establishment of MHNTs. These teams provided basic curative and preventive health and nutrition services where health facilities had been destroyed or health workers were not available.
Each MHNT consisted of three trained nurses, one health officer, and a midwife. Teams provided nutrition screening, referral, and treatment for children with malnutrition. Infant and young child feeding in emergencies support and counselling and micronutrient supplementation services were also provided. Teams were deployed to internally displaced persons (IDP) sites and communities, offering nutrition services integrated with other routine health services.
At IDP sites with larger population sizes, temporary service delivery sites were established, and these were supported by an MHNT providing outreach services in that area. In the two regions of Afar and Amhara, UNICEF supported 66 MHNTs through its partnerships. In Tigray, 86 MHNTs were operational – most of them were located near large populations of IDPs.
© Raphael Pouget, UNICEF Ethiopia
Baby Solom being screened for acute malnutrition using a mid-upper arm circumference band by a health worker at Selekleka health facility, Tigray. Ethiopia, 2022.
Find and treat campaigns
Find and treat campaigns were launched in August 2021 by UNICEF with the aim of sustaining malnutrition prevention efforts and expanding treatment services to priority areas. They represent a rapid response and quick assessment mechanism to be delivered through UNICEF’s partners together with the regional health bureau and health extension workers alongside communities.
All children and women in a woreda were targeted for screening using mid-upper arm circumference (MUAC) measurements either in their homes or at a central point. The campaign integrated provision of other services like micronutrient supplementation, health promotion, immunisation, and distribution of water treatment tablets.
As part of the campaign in Tigray, Afar, and Amhara, UNICEF screened 2.5 million children and 500,000 pregnant and lactating women for wasting, providing treatment on the spot for the malnourished while linking them to health facilities for follow up between August 2021 and December 2022. This led to 18% (230,000 children) of the targeted annual admissions for wasting in the 2022 Humanitarian Response Plan being admitted through the campaigns. The find and treat campaigns have also been useful in estimating nutrition needs in the absence of regular nutrition surveys (Figure 2).
Figure 2: Find and treat campaign results for northern Ethiopia
Partnerships
When the crisis began in Tigray, partnerships to scale up the nutrition humanitarian response were created with UNICEF engaging eight international NGOs. By 2022, the coverage of the response improved as more partners were engaged to cover the gaps in service delivery and the response scaled up from 30 woredas in 2021 to all 79 accessible woredas in 2022. Similarly, WFP engaged the same international organisations and scaled up in 2022 to cover all accessible woredas through 12 partners.
As the response progressed, it became apparent that local partners had the comparative advantage of moving to areas of need where international partners had limited access due to security concerns. Local partners also provided lower operational costs, which helped increase coverage, and had good knowledge of geographic areas and the context, with extensive networks on the ground. They had the confidence of regional government and communities, allowing them to navigate constraints and deliver services. UNICEF thus engaged its first two local partners in early 2022 in Tigray. By 2023, six local partners were supporting the nutrition response in 22 woredas (30% of the total).
Local partners spearheaded UNICEF’s find and treat campaigns and supported emergency nutrition services. Their technical capacity was sometimes suboptimal, including on highly technical nutrition rehabilitation programmes. This was further compounded by an inability to source international technical capacity due to the restrictions in place. To overcome this, some international organisations sub-granted local partners in their areas of response and supported skills development. UNICEF also provided technical support throughout, deploying trained local consultants with the required technical skills and experience in nutrition as needed.
Local partners also faced operational constraints. For example, the cessation of banking services prevented access to cash, and they were not able to bring in cash through humanitarian flights arriving into Tigray, as international NGOs did. To ensure continuity of services, UNICEF initiated bringing in cash to advance to local partners.
Coordination
UNICEF, WHO and WFP, the three United nations agencies engaged in the nutrition response, had pre-existing working relationships, and could pool expertise to manage children along the continuum of care. Due to the increasing scale of the emergency, UNICEF as cluster lead agency, took the lead for coordination efforts, working alongside the government (EDRMC, Ministry of Health and the Ethiopian Public Health Institute) and all cluster members to provide technical support and to ensure a timely, effective response. In places where the ENCU (regions and national) was functioning, the hybrid coordination was ensured with EDRMC and UNICEF.
At Federal level the Multi Agency Nutrition Task Force or Nutrition Cluster coordination meetings were also organised bi-weekly. Coordination meetings were held weekly in Afar and bi-weekly in Amhara to respond rapidly to the emergency. In Tigray, where the context was more complex, a dedicated nutrition cluster coordinator, a co-coordinator and an information manager supported the response.
Nutrition information systems
In Afar and Amhara, routine nutrition information was collected from health facilities using paper-based tools which were submitted monthly to woreda health offices. The woreda health office would then enter the data into the national health management information system (HMIS). However, because there were only a few nutrition indicators in the Ethiopian HMIS, a parallel ENCU data set has been used for the past 15 years to collect health facility data on severe wasting admissions and outcomes. This system was pivotal in monitoring the progress of the emergency response.
In Tigray, due to limited communication services, fuel, and health facility access, the routine nutrition data reporting system could not be used. The cluster therefore supported the use of an Excel-based tool where partners provided weekly data on wasting admissions, outcomes, and other nutrition services. This alternative reporting system also faced operational challenges; physical reports that were collected from health facilities had to reach the regional level, which was a lengthy process. This meant that regular reports were available only for the most accessible health facilities – an average of 31% of outpatient sites and 61% of stabilisation centres were reporting monthly. Despite these limitations, this data was used to continuously monitor the nutrition response.
The lack of population representative surveys during the emergency phase complicated response planning. As an alternative, MUAC screening data was included in multisectoral assessments in Tigray (e.g., in the emergency food security assessments). Find and treat campaigns and rapid nutrition assessments also served to provide a snapshot of the nutrition situation using the CDC protocol on nutrition assessment using MUAC measurement (Figure 2).
Supplies and resources
As needs increased, development funds were reprogrammed to provide the initial response, including procurement of supplies and operational budgets. Availability of nutrition supplies in facilities was limited due to access issues (see below) and transportation challenges linked to a shortage of fuel. The Logistics Cluster played an essential role, airlifting required nutrition supplies when road movement was not possible and organising for the passage of supplies after the road network re-opened.
Access
Maintaining access to areas of need became difficult at various stages of the conflict, causing a sporadic supply of nutrition commodities, fuel, and cash availability (Figure 3). The humanitarian corridor often faced long waiting times for the clearance of goods and sometimes total blockage. Most international NGOs that participated in the response were unable to travel freely to affected areas due to intensified security procedures. As noted above, local partners had easier access and became increasingly involved in the response.
Figure 3: Northern Ethiopia access map
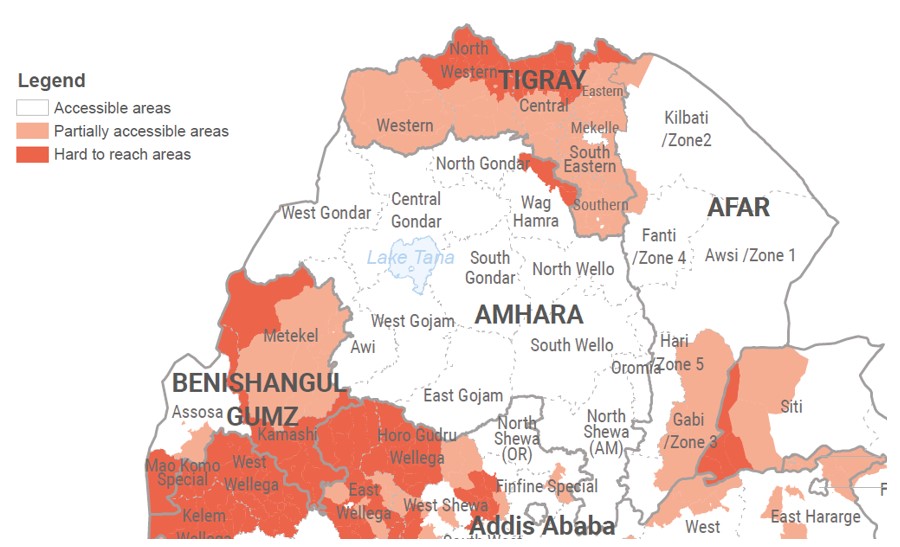
Source: OCHA
Note: Correct as at 30 November 2022
Lessons Learned
Despite the challenges, the nutrition sector managed to scale up the treatment of children with wasting and respond to the nutrition needs of over 200,000 children with severe wasting (52% of the estimated children in need), as well as 2.5 million children with moderate wasting, in the three regions. Counselling and support were provided to improve infant and young children feeding practices and prevent malnutrition among children under five. Most children targeted (80%) received vitamin A supplementation in 2022, by means of the integration of the service into the find and treat and measles campaigns.
Through this response, coherent and meaningful partnerships between United Nations agencies and implementing partners were formed, guided by humanitarian principles, best practices, and value for money. Intersectoral efforts to reduce malnutrition - in which the food, health, and water, sanitation, and hygiene clusters also played a role in preventing malnutrition in children - highlighted the benefits of a multifaceted, coordinated response.
The localisation of the response was instrumental in reaching more people with nutrition services. As the response progressed, local partners expanded their geographic coverage and offered services in areas deemed inaccessible by other agencies. Other local solutions (e.g., the use of animal-drawn carts to make nutrition commodities available to hard-to-reach health facilities) were instrumental in providing a continuum of care in most areas.
The response was a continuous learning curve for nutrition partners in northern Ethiopia. Practical solutions were made on partnership framework agreements and operational processes to ensure that nutritional humanitarian needs were met. Flexibility in engaging partners despite not having formal agreements with UNICEF or WFP helped ensure a timely response in an unpredictable and ever-changing context. United Nations agencies now need to work toward stronger strategic and operational partnerships with implementing partners. For instance, having programme agreements with a unique partner to cover a given geographical location appears good practice, but more evidence is needed to demonstrate that better outcomes are reached.
Conclusion
The nutrition response in northern Ethiopia achieved positive results due to the commitment of nutrition partners. The strategic processes of the Nutrition Cluster led to better accountability and improved the scale and standards of nutrition activities. Extending the engagement of local actors within the response was instrumental to its scale-up and sustainability. Going forward, the nutrition response will benefit from investment in building resilient communities and systems in case of future shocks.
For more information, please contact Nakai Munikwa at nmunikwa@unicef.org
References
Ethiopian Public Health Institute and ICF (2021) Ethiopia Mini Demographic and Health Survey 2019: Final Report. dhsprogram.com.
Global Nutrition Cluster (2022a) Tigray strategic nutrition operational response and capacitation plan. Global Nutrition Cluster Technical Alliance & United States Agency for International Development.
Global Nutrition Cluster (2022b) Tigray nutrition response: Comprehensive nutrition actions package. Global Nutrition Cluster Technical Alliance & United States Agency for International Development.
Federal Ministry of Health, Ethiopia (2019) National Guideline for the Management of Acute Malnutrition May 2019. nutritioncluster.net.
OCHA (2021) Northern Ethiopia response plan – 2021. humanitarianresponse.info.
OCHA (2022a) Ethiopia: Humanitarian Response Plan 2022 (July 2022). reliefweb.int.
OCHA (2022b) Ethiopia – Access Map (As at 30 November 2022). reliefweb.int.
1 GAM provides information on the percentage of all children aged 6–59 months in a population with low weight-for-height and/or oedema.
2 Fortified flours consisted of fortified Corn Soya Blend (CSB++).