Cost-efficiency of a simplified protocol for wasting treatment in Mali
Lisez cet article en français ici
Derek Lee is a Best Use of Resources Advisor for Nutrition at International Rescue Committee (IRC).
Cesaire Ouedraogo is a Nutrition Research Coordinator at IRC.
What we know: The use of ‘simplified protocols’ for the treatment of wasting have been shown to be non-inferior yet less resource intensive compared to traditional treatment protocols. Logically, reduced ready-to-use therapeutic food (RUTF) dosage, among other programmatic simplifications, will result in reduced programme costs.
What this adds: This paper assesses the cost-efficiency of different treatment protocols in Mali, comparing the traditional treatment protocol against a simplified approach. Across every spending category, treating severely wasted children with a traditional protocol cost more than under the simplified protocol.
Background
The treatment of wasting is currently divided into separate programmes based on severity. Uncomplicated severe wasting is treated through outpatient therapeutic feeding programmes, whereas moderate wasting is often treated through supplementary feeding programmes. While wasting is essentially a spectrum from mild to moderate to severe – with cutoffs acting as necessary proxy thresholds to designate treatment – these treatment programmes often run independently from each other with different sites, treatment days, and using different products with their own supply chains.
The Combined Protocol for Acute Malnutrition Study (ComPAS) demonstrated that, in Kenya and South Sudan, a combined and simplified protocol was non-inferior to conventional treatment for children admitted to treatment by mid-upper-arm circumference (MUAC) measurement or presence of oedema (Bailey et al, 2018). In the study, severely wasted children were treated with two daily sachets of RUTF and moderately wasted children were treated with one daily sachet of RUTF – whereas in the conventional treatment, dosage was calculated as kcal/kg/day.
However, questions have remained about the effectiveness and larger cost implications of the protocol change in a routine setting. To provide further evidence, IRC conducted a combined and simplified wasting treatment pilot in rural Mali. In December 2018, IRC and the Ministry of Health (MoH) in the Nara region of Mali transitioned to a simplified protocol to treat wasting. For three years – until December 2021 – 27,800 children aged 6–59 months were treated with this protocol in 35 health facilities and 38 community health sites. The pilot sought to maximise treatment coverage by combining the treatment of severe wasting and moderate wasting, providing treatment at the community level through community health workers (CHWs), and training caregivers to detect and monitor their children’s nutrition status using MUAC bands (known as the ‘family MUAC’ approach).
Methodology
The simplified treatment pilot conducted in Mali complied with the ComPAS trial protocol. Children were discharged after two consecutive measures of MUAC ≥125mm and the absence of oedema for two weeks. All patients were followed up weekly at treatment sites with regular MUAC, weight, and height measurements.
Treatment was provided by both government-employed health workers and incentive-provided IRC CHWs at health facilities (primary sites), as well as solely by CHWs at community health sites (secondary sites).
The cost analysis was designed as a pre-post study; data from before and after the switch to the simplified protocol were analysed. We tracked expenditure and patient data over time to determine the cost implications of the protocol switch and any potential cost-efficiency gains.
The effectiveness of the simplified protocol pilot was assessed through an observational cohort study (Kangas et al, 2022). IRC cost-efficiency was determined through IRC’s standard cost methodology and use of the Dioptra software – a multi-sector costing tool managed by a consortium of non-governmental organisations. Dioptra provides quick cost-efficiency calculations for humanitarian projects using standardised humanitarian costing methodologies.1
We have presented our findings first by overall cost by year, number of children treated (by different protocols), and then cost per child treated – allowing us to view the overall cost-efficiency of the simplified protocol. We then break down total yearly costs into cost categories, highlighting the main cost drivers of a given year. We then calculate how many children can be treated with 100 cartons of RUTF under the simplified vs traditional protocol, an important real-world consideration for programmers.
In addition to following the standard IRC cost-efficiency research method, supplemental data were collected to analyse the costs borne by caregivers, the MoH, and UNICEF. This was to ensure that any cost savings made by the implementing organisation were not a result of offloading costs onto others.
To evaluate MoH and caregiver costs, we performed additional surveys and interviews of MoH staff responsible for treatment. Health centre staff were surveyed to determine their wage, which was then allocated to treatment based on the number of days per week each health facility provided treatment. This was done to create a cost per facility, which could then be used to determine the cost per child at each facility.
While care and treatment were provided to patients for free, additional costs borne by caregivers fell into three categories: the opportunity cost of caregivers’ time; foregone income; and any out-of-pocket expenses for transportation. To estimate caregiver costs, we conducted surveys on a random sample of 150 caregivers stratified by distance to track their typical daily activities that must be foregone to access treatment. The surveys also collected socioeconomic and demographic characteristics.
RUTF consumption cost estimates were also generated, based on average RUTF consumption per admission type (severe or moderate wasting) and assuming a constant cost of USD 0.75 per sachet.
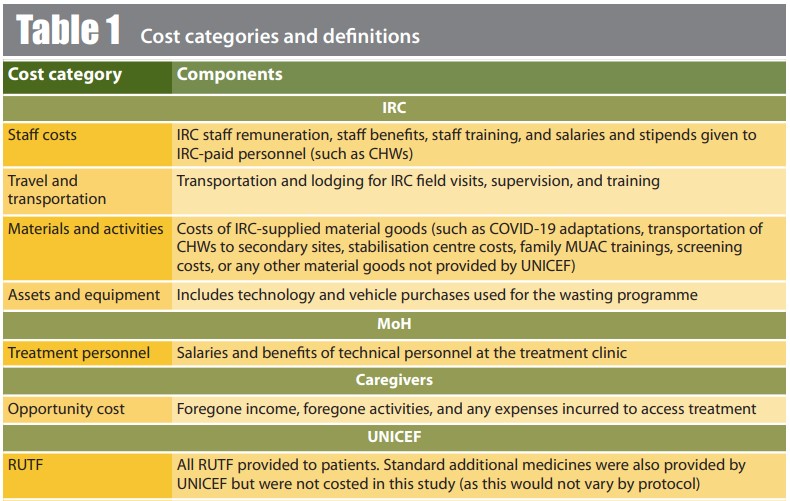
All the components included in the costing analysis are provided in Table 1.
Results
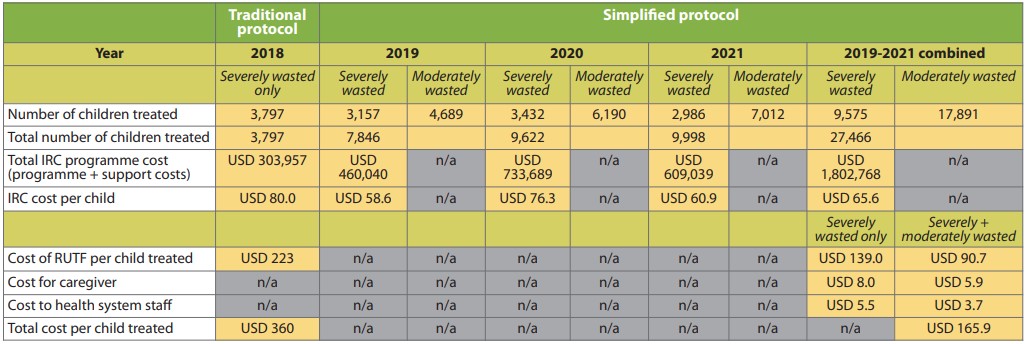
All data resulting from our analysis are provided in Table 2.
Table 2: Costs and cost-efficiency data results in Nara, Mali
Implementing partner costs
Overall, a more cost-efficient programme
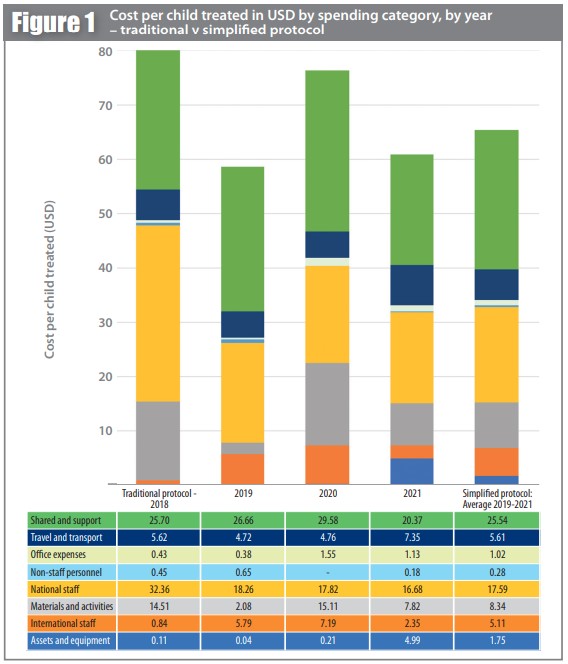
The IRC spent slightly over USD 2.1 million on acute malnutrition treatment in Nara between December 2017 and December 2021 (Table 2). Annual spendings were around USD 300,000 when the traditional protocol was implemented compared to around USD 600,000 per year under the simplified protocol pilot phase. However, due to the increased caseload that we could manage under the simplified protocol, the cost per child treated was lower (USD 65.6 per child) than when using the traditional protocol (USD 80.0), which corresponds to an improved cost-efficiency of 18%.
The higher costs per child treated in 2019 and 2020 were a result of additional start-up and COVID-19 costs. These estimates reflect the IRC spendings only – they do not include government personnel time nor RUTF costs.
The cost per child treated was lowest in 2021 (Table 2 and Figure 1). This reduction was largely driven by the decreasing needs for set-up, training, and COVID-19 prevention materials (e.g., the installation of handwashing facilities, COVID-19 awareness campaigns, bulk purchasing of personal protective equipment, etc.) – which were still being incurred well into 2020. Our analysis showed that pandemic-related costs accounted for an additional 17% of the budget (data not shown) compared to costs in 2021 (USD 60.9 per child), which represented more ‘normal’ conditions despite some COVID-19 measures still being in place.
We observed additional costs in 2019 that were related to the protocol change, but most new programmatic costs were incurred in 2020 – after the health staff became more familiar with the new protocol. Start-up included activities such as family MUAC trainings and the establishment of new secondary sites.
Direct programme costs
The main cost drivers for the simplified protocol in Nara were related to staff and personnel for IRC – 27.0% national staff and 7.8% international staff; 8.6% for travel and transport (percentages derived from Figure 1). This is typical of other IRC-implemented wasting treatment projects. IRC staff were responsible for the management and coordination of malnutrition treatment. Community health worker stipends also contributed a significant proportion in the same category of costs, given the large number of CHWs needed to provide treatment (at secondary sites), screening, and outreach services.
After staff and personnel costs, the largest amount of spending was on materials and activities (12.8%). These costs were primarily the drugs and medical supplies provided to malnourished children. A large proportion of these medical goods were used in stabilisation centres, where the most vulnerable children receive more complex medical interventions.
In total, 39.1% of total IRC spending on the project was on indirect ‘shared project costs’. These include IRC office rental costs and support staff (e.g., logistics, security, and human resource staff).
Ready-to-use therapeutic food costs
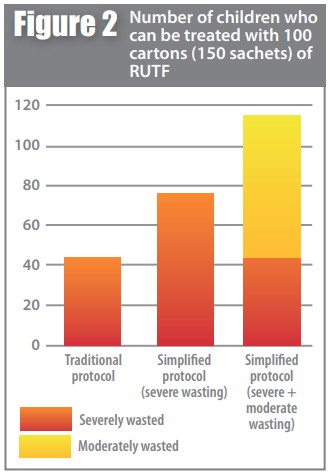
Per child treated, the RUTF costs fell from USD 223 to USD 91 once we switched to the simplified protocol (Table 2). The difference in RUTF costs can be attributed to two factors.
First, the simplified protocol adapted the overall quantity of supplies per child treated – severely wasted children were treated with two daily sachets of RUTF whereas with the traditional protocol dosage was calculated based on kcal/kg/day. The simplified protocol required 38% less RUTF per severely wasted patient treated than the traditional protocol – a reduction in the cost of RUTF from USD 223 to USD 139. For the same amount of RUTF procured, the simplified protocol can potentially treat either 77% more severely wasted children or 155% more moderately wasted children (compared to numbers of severely wasted children) (Figure 3).
Second, the inclusion of moderately wasted children drove down average RUTF consumption per child being treated – as moderately wasted patients require less RUTF to fully recover. This is important, as this skews the average cost per child treated. Including moderately wasted children may not result in reduced overall RUTF use and its associated costs, but it will increase cost-efficiency and allow more children to be treated – an important distinction for both programmers and donors.
Cost to clients
Total caregiver costs per visit – opportunity cost (time lost), foregone income, and out-of-pocket expenses – were estimated from survey results to be equivalent to a little over USD 1.0 per week.2 Caregiver costs for severely wasted children (USD 8.0 for an average length of stay of 7.7 weeks) were higher than those of moderately wasted children (4.6 weeks) as more visits were required with more severe cases. The overall average caregiver cost was USD 5.9 for an average length of stay of 5.7 weeks for child treatment (Table 2).
Additional analysis of treatment provided by CHWs at secondary sites showed that visits are, on average, 57% more cost-efficient for caregivers compared to visits to primary treatment sites. This cost difference was driven primarily by reduced opportunity costs (time lost), as travel time was reduced and there was a steep reduction in out-of-pocket costs that were inherent when accessing primary health centres.
Costs to health system staff
The analysis of staff costs (by treatment site type) highlights increased cost-efficiency at secondary sites – USD 5.5 (primary sites) and USD 1.0 (secondary sites) per child treated. This is largely driven by staff salaries at primary sites, which encompass both formally trained (more expensive) health workers and CHW stipends. Despite the much larger caseloads that health facilities are able to treat, treatment at secondary sites is provided by only a single CHW. Staff treatment costs were around 5–6 times cheaper at secondary sites.
Overall, the average staff cost for all children treated was USD 3.7. Further research is ongoing around the costs associated with running secondary sites compared to primary health facilities.
The bottom line
Looking at the total costs for all agencies and caregivers, the cost per child treated under the simplified protocol was USD 165.9 (including support and in-kind RUTF costs), whereas the cost per child treated under the traditional protocol was USD 360.0 per child, even without the additional caregiver and MoH costs.
Study limitations
For caregiver and MoH staff costs, we were unable to perform pre- and post-analyses as we did not collect caregiver and MoH costs prior to the switch to the simplified protocol. In addition, IRC also added additional nutrition activities such as the establishment of secondary sites and ‘family MUAC’ training, which hinders our ability to make direct comparisons.
Cost-efficiency conclusions
The cost analysis results demonstrate that the simplified protocol in Nara, Mali was more cost-efficient per child than the traditional protocol previously implemented. Across every spending category, treating severely wasted children with the traditional protocol costs more than under the simplified protocol. Regardless of protocol, the findings suggest that scale is a major determinant in cost-efficiency.
Our study’s results align with our previous ComPAS study in Kenya (Bailey et al, 2018) and its accompanying effectiveness paper, which demonstrate that the simplified protocol reduced the dosage of RUTF for severely wasted children without reducing treatment efficacy.
While there is still much work to be done to improve wasting treatment for children, simplified, combined approaches can provide strong support through the reduction of costs to implementing agencies, ensuring that programmes can more readily be achieved at scale and at lower costs to caregivers and service providers.
For more information, please contact Derek Lee at derek.lee@rescue.org
References
Bailey J, Lelijveld N, Marron B et al. (2018) Combined Protocol for Acute Malnutrition Study (ComPAS) in rural South Sudan and urban Kenya: Study protocol for a randomised controlled trial. Trials 19, 251.
Kangas S, Marron B, Tausanovitch Z et al. (2022) Effectiveness of acute malnutrition treatment at health center and community levels with a simplified, combined protocol in Mali: An observational cohort study. Nutrients, 14, 22, 4923.
1 For more information on the IRC’s costing methodology, see https://www.rescue.org/resource/malnutrition-cost-analysis-methodology-irc
2 We used the Malian minimum wage rate (CFA 28,465 per month or USD 50.34) to cost the time spent accessing treatment, as the survey demonstrated that almost all caregivers were not engaged in any income-generating activities.


