Food-based recommendations to improve vitamin A and iron intake in Niger
Jen Burns Senior Technical Advisor, Nutrition in Humanitarian Contexts, USAID Advancing Nutrition
Lisa Sherburne Technical Director, Social and Behaviour Change, USAID Advancing Nutrition
Mamoudou Djibo Khaled former SBC Advisor for USAID Advancing Nutrition, Niger
Hadiara Souley former Nutrition Lead for USAID Advancing Nutrition, Niger
Jennifer Nielsen Senior Advisor for Nutrition, Helen Keller International
Abigail Conrad Learning and Research Advisor, USAID Advancing Nutrition
We acknowledge the senior leadership of this work, namely Marily Knieriemen (Chief of Party, USAID Advancing Nutrition, Niger) and Tina Lloren (Director of Country Programs, USAID Advancing Nutrition), for their support to the activities in Niger.
What we know: In Niger, iron and vitamin A deficiency remain high for multiple reasons. The provision of information alone is often not sufficient to change behaviours.
What this adds: An approach to increase the consumption of vitamin A- and iron-rich foods was designed with community members. These tools identified 18 locally available foods rich in vitamin A and iron that were available and acceptable for young children and pregnant women, as well as household roles that could be promoted through community-based platforms (Husbands’ Schools, women’s peer groups, and radio spots).
Background
Diets are typically insufficient in rural Niger. Few pregnant and lactating women or children aged 6-23 months consume an adequately diverse diet (Cisse-Egbuonye et al, 2017; Egbuonye et al, 2021). Coverage of vitamin A and iron-folic acid supplementation is also inconsistent, with quality implementation constrained by multifaceted barriers (Begum et al, 2018).
The Ministry of Public Health (MoPH) has a national nutrition security strategy, a micronutrient supplementation strategy, a national health and nutrition social and behaviour change (SBC) communication strategy, and multiple resources for promoting improved diets, including a national book of recipes. Despite these resources, more can be done to support households in food-insecure contexts to consume locally available and acceptable iron- and vitamin A-rich foods.
We introduced a systematic process to improve dietary practices among pregnant and lactating women and children aged 6-23 months by developing evidence-based tools that can be integrated into existing community-based programming platforms.
Programme description and justification
Between 2020 and 2023, the United States Agency for International Development’s (USAID) flagship multi-sectoral nutrition project, USAID Advancing Nutrition, targeted: a) a reduction in the prevalence of anaemia for women of reproductive age and adolescents; and b) a reduction in vitamin A deficiency in children under five years.
We collaborated with the MoPH and USAID implementing partners in Maradi and Zinder regions - areas with the highest prevalence of malnutrition and food insecurity - to meet our objective through existing programmes and strategies.
Effective nutrition SBC promotes the adoption of healthy behaviours and reduces barriers to maintain those behaviours over time (USG, 2022). Understanding the role of human behaviour is key to the success of nutrition interventions, as every change requires someone to act - whether market actors, health workers, community leaders, or family members.
Quality nutrition SBC processes follow six key steps: 1) prioritising behaviours that can improve nutrition outcomes; 2) formative research; 3) strategy design; 4) planning for implementation and monitoring; 5) implementation; and 6) evaluation. This article focuses on the first four steps, with MoPH and partners responsible for subsequent implementation and evaluation.
Methodology
Defining priorities
We reviewed existing data to identify the behaviours that have the largest impact on iron and vitamin A intake. The team prioritised six behaviours (‘behavioural outcomes’), which included two related to dietary improvement – ”œcaregivers use a variety of nutrient-rich foods each day in the meals and snacks of their child aged 6–23 months” and ”œpregnant and lactating women eat a variety of nutrient-rich foods daily, for both meals and snacks.”
Conducting formative research
To understand the factors that prevented or supported people to practise these priority behaviours, we conducted formative research with women, their family members, community leaders, health providers, and stakeholders at national and district levels.
The findings highlighted the importance of social and gender norms, as well as family support, in improving women’s and children’s dietary diversity. The need to improve food access and quality counselling – focusing on locally available food rather than the variety of ‘good’ foods, which may be unavailable to households – was also highlighted.
Elaboration of intervention strategies
Using the research findings, we engaged with MoPH and partners at the national and sub-national levels to prepare and validate an SBC strategy to operationalise the micronutrient elements in the national SBC communication strategy and bolt on to communication solutions, which identified activities to strengthen existing programmes by reducing barriers to action.
Planning
Partners mapped their activities in the two regions to visualise where there was convergence and where there were gaps. With this roadmap, we co-created solutions with partners for community media and materials that could be integrated into existing nutrition programmes.
We prepared flipcharts for group discussions that modelled positive social and gender norms and greater family support for women’s food choices, for herself and her children. One set was specific to fathers and husbands, for use in ‘Ecoles des maris’ (Schools for Husbands). We also prepared community radio spots and magazines with technical support from Breakthrough ACTION.1 Each material was pre-tested and refined with communities.
Local partners identified vitamin A- and iron-rich foods to promote in these materials that were both acceptable and locally available within their communities. We then used food databases and composition tables to identify and then form a list of those foods with greater micronutrient density.
To ensure acceptability, we asked ”œwhich of these key foods would women be willing and able to eat more of, or feed young children of different ages?” USAID Kulawa and Girma conducted participatory exercises with two communities as part of this step. Using the average amount of food that caregivers may add to their own or their child’s meal, community groups tested food preparations via focus group discussions, pile-sorting exercises, group food preparation exercises, and reflection.
Barriers to adequate dietary intake
Access to affordable, locally available foods
Access to diverse vitamin A- and iron-rich foods remained a primary challenge for communities. Although caregivers knew about ‘good’ foods to feed children (from health workers and the media), many of these foods were simply not available in their homes. Agricultural yields did not last all year and, even if available in their community, many foods were unaffordable - including animal source foods such as kilishi (dried meat), locusts, liver, and eggs.
Social and gender norms
For women, we found that social and gender norms constrained food choices and were entwined with family support. Men were the primary decision makers about what food to purchase and what crops to grow, while women were responsible for gathering wild greens and fruits. Women (including those pregnant or lactating) were expected to serve their own food last, after all other members of their household, with little food remaining.
For young children, customs held by elder women dictated that children were fed a monotonous porridge consisting primarily of millet or sorghum. Children aged 6-11 months were usually fed from a cup two to three times a day. Caregivers offered children aged 12-23 months the same food at the same frequency, but double in quantity. Such social norms further limited food choice when adding to children’s meals (e.g., some communities believed children should not eat eggs, leafy greens, and/or meat).
"We also do not give eggs to children under five, otherwise the child will be locked up like an egg, that is to say, it takes a long time before it starts to speak" - Community leader
However, some norms were found to enable positive change. Communities noted that men were expected to provide for their families and care for their wives and children, while and mothers-in-law were responsible for teaching their daughters-in-law. Most men and older women felt motivated by the positive recognition of fulfilling their roles.
Counselling on diets
Women shared that health workers advised them on good foods to eat during antenatal care visits, outreach, and community groups - although they recognised that most of the recommended ‘good’ foods were not available in their communities. Even if available, as women they would not have the choice to eat the food or not.
Selecting vitamin A- and iron-rich foods
Shortlisting available foods
To identify specific iron- and vitamin A-rich foods that were available in these highly food-insecure communities, and that were feasible for caregivers to feed children and eat themselves, we first narrowed down a list of 18 foods (Table 1). Using this list of foods available locally, partners conducted exercises in two communities.
Table 1: Nutritional content of locally available foods for children in Niger
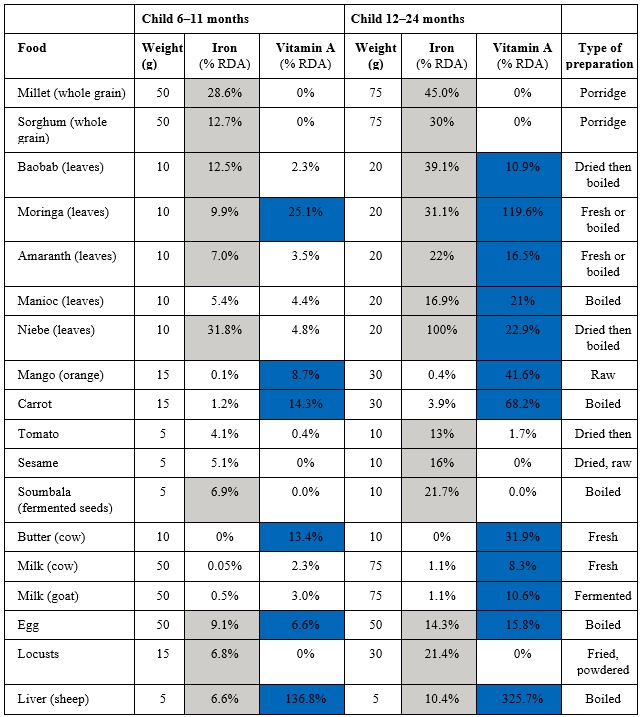
RDA = Recommended daily allowance
Highlighted values indicate foods with favourable iron (grey) and vitamin A (blue) contents.
Acceptable foods for children
Through interactive card-sorting exercises, caregivers narrowed the list to the foods they would be willing to feed their children. In both communities, caregivers identified three foods that they found acceptable and realistic to add to their child’s meals all year round: 1) dried moringa powder; 2) dried bean leaf powder; and 3) goat’s milk.
Caregivers noted that they grew and gathered moringa and bean leaves in the wild so they could process these at home to feed children. When caregivers cooked porridge using one of the three identified foods, they saw that children enjoyed the taste and finished their meal. Caregivers in these communities also identified cow’s milk, butter, mangoes, baobab leaves, crickets, small fish, liver, and sesame as having the potential to feed children, but only when seasonally available.
Acceptable foods for mothers
Pregnant and lactating women used the list of locally available foods to narrow down five acceptable additions: 1) cow’s butter; 2) eggs; 3) moringa leaves; 4) liver; and 5) goat’s milk.
Learnings
Successes
Addressing malnutrition requires multiple actors coordinating at the same time and place. Through a participatory process, USAID Advancing Nutrition collaborated with the MoPH at national and sub-national levels and six nutrition partners. This collaboration ensured technical expertise and co-design to develop tools that met programme needs.
Achieving SBC relies upon locally acceptable and feasible actions; giving technically sound information is rarely sufficient for people to make changes. Focusing on activities that promote dietary diversity - including counselling, group discussions, and using media to promote specific foods - gives realistic options to enable practical skills development, problem solving, and action. The final list of key foods that are locally available and acceptable helps to contextualise the national recipe book to select recipes that promote iron- and vitamin A-rich foods.
Challenges
The limited time available was a key challenge, as the programme ended just prior to providing the finalised tools to MoPH and nutrition programmes for use. Therefore, we do not yet have findings on effectiveness in programme settings beyond a pretest.
Status quo bias - i.e. the tendency to prefer what is familiar - is common in nutrition, making the introduction of new foods a challenge. Educating mothers and fathers is usually not sufficient to overcome this bias.
Additive bias - i.e. the tendency to solve problems through addition - meant that nutrition experts were tempted to include all possible nutrient-rich foods on key food lists. However, focusing on a smaller number of changes and limiting new information is often more effective in SBC strategies. Engaging community members in the process of selecting only foods that were available, affordable, and desirable helped to keep these lists focused and relevant.
Lessons learned
Communities have solutions. They were able to identify locally available and acceptable iron- and vitamin A-rich foods to feed young children and pregnant and lactating women. Communities also shared the reasons why their knowledge about nutrition was not put into practice and what they needed to make changes. This demonstrates the importance of community engagement to identify solutions.
Communities also highlighted the need for greater support for women. Positive social and gender norms revealed opportunities for change through culture (e.g., the representation of an ideal man). These strong norms are an entry point for reflection and discussion related to nutrition, especially in the early days of life, when lifelong benefits to the family and including the father can be achieved.
"The ideal husband is one who provides for his family and takes on all the family burdens, such as health, education, food, and clothing. He cannot have peace of mind when the family is in a critical situation." - A father from Zinder
Although the list of locally available foods received multiple reviews and revisions, the shortlist was identified by only two communities. Partners working in these regions could engage other communities to confirm or refine the short list so that it is adapted to their specific contexts.
Conclusion
As the government and implementing partners strengthen the agricultural sector, improving access to and use of micronutrient-rich foods is needed to improve diet quality in rural Niger. Identifying and promoting acceptable, locally available, micronutrient-rich foods is critical to making this happen.
Using SBC methods, USAID Advancing Nutrition and implementing partners facilitated a stepwise approach that focused on the issues identified by women and communities, instead of relying on generic information. We designed new tools, including technical briefs, radio spots for communities, group discussion flipcharts for community-based groups, and a guide to localise food-based recommendations. Their actual use and impact will now need to be taken forwards by MoPH and implementers.
For more information, please contact Mohamed Yattara at myattara@hki.org.
References
Begum K, Ouédraogo CT, Wessells KR et al. (2018) Prevalence of and factors associated with antenatal care seeking and adherence to recommended iron-folic acid supplementation among pregnant women in Zinder, Niger. Maternal & Child Nutrition, 14, 1, e12466.
Cisse-Egbuonye N, Ariun I, McKyer ELJ et al. (2017) Examining Nutritional Adequacy and Dietary Diversity Among Women in Niger. Maternal and Child Health Journal, 21, 6, 1408-1416.
Egbuonye N, Ariun I, McKyer ELJ et al. (2021) Examining the Dietary Diversity of Children in Niger. Nutrients, 13, 9, 2961.
USG (2022) U.S. Government Global Food Security Strategy Fiscal Year 2022-2026. usaid.gov.
1 Breakthrough ACTION is USAID's flagship global SBC project, which encourages people to adopt healthier behaviours.


