Integrated Community Case Management ‘Plus’: Treating closer to home in Somaliland
Yuusuf S Yuusuf Research Coordinator Integrated Community Case Management Plus at Save the Children International, Somalia/Somaliland
Mohammed Ismail Mahamoud Area Research, Evaluation, Accountability, Learning and Monitoring Manager at Save the Children International, Somalia/Somaliland
Said A Mohamoud Research Advisor at Save the Children International, Somalia / Somaliland
Guleid Mahdi Mohamed Integrated Community Case Management plus Coordinator at Save the Children International, Somalia/Somaliland
Saeed Mohamood Soleman Senior Health Policy & Integrated Planning Specialist, Somaliland Ministry of Health Development
Lucas Nene User Insights & Service Design Consultant at DesignHealth
Emily Keane Senior Nutrition Advisor at Save the Children
Meftuh Omer Head of Health, Nutrition, and WASH at Save the Children International Somalia / Somaliland
Adan Yusuf Mahdi Senior Nutrition Technical Specialist at Save the Children International Somalia / Somaliland
Nimo Gulied Nutrition Programme Manager at Save the Children International Somalia / Somaliland
What we know: Integrated Community Case Management (iCCM) improves coverage and quality of care for sick children by training community health workers to diagnose, treat, and refer common childhood illnesses at the community level. Adapting the iCCM platform to include treatment of wasting shows promise.
What this article adds: The iCCM+ service prototype implemented in Somaliland, which focused on female health workers (FHWs), was encouraging – with findings indicating that common barriers to wasting treatment services can be reduced when provided as part of an iCCM package. ‘User-centred’ and ‘service design’ approaches provide great value, ensuring that services are effective by solving operational challenges as they arise.
Improving Access
In Somaliland 1.4 million children under five years are wasted (Ministry of Planning and National Development, 2020). The iCCM platform screens for and refers children with wasting to local health facilities, but coverage and accessibility are often low. Rural communities lack consistent, cost-effective transport and caregivers must often find financial resources to access health facilities, often involving a day-long commitment away from the household. Inconsistent communications between health facilities and FHWs may also result in a wasted trip – such as in the event of a stock-out of treatment supplies. These challenges may then repeat over the duration of treatment until a child is discharged.
Adapting current iCCM platforms to provide wasting treatment alongside common illness treatment (named ‘iCCM+’) may offer a solution that improves access to these essential services.
This article documents the process and learnings of Save the Children’s experience between 2022 and 2023. Save the Children worked with DesignHealth1, Somaliland’s Ministry of Health Development (MoHD), community members, and health workers to design and refine a service prototype for FHWs to treat uncomplicated wasting within iCCM.
Methodology
Save the Children has been implementing facility-level health and nutrition programmes in Somaliland since 1991 and community-based health services since 2017. In 2019, Save the Children started integrating iCCM and severe and moderate wasting treatment by FHWs. This was the first time iCCM+ was operationalised in Somaliland. We therefore undertook a process of adapting and contextualising protocols and tools that had been developed in other contexts (Marron, 2021) to develop an ‘iCCM+ service prototype’ that would enable low-literacy health workers to treat wasting in Somaliland (Box 1). For this process we utilised ‘user-centred design’, which is a phased approach to developing health services, user experiences, and products, in collaboration with DesignHealth. Each phase involved users throughout the design and development process, incorporating and building upon the evidence established in the previous phases. The service prototype used all five principles of service design: user-centredness, co-creation, efficient sequencing of events, evidencing design decisions, and a holistic approach to stakeholder needs. The process facilitated rapid feedback and adaptations to be made as service delivery was ongoing.
Box 1: ProcessDevelopment of the simplified iCCM+ tools progressed throughout 2019 and into 2020, including four field visits for testing and co-creation with Somaliland's FHWs. The complete suite of simplified tools was delivered in late March 2020. In response to COVID-19 treatment protocol amendments, DesignHealth was tasked with creating additional FHW and community COVID-19 awareness job aids. All content was translated into the Somaliland dialect of the Somali language by May 2021. Operational planning and service delivery design began in 2022. The 'service prototype phase' ran between June 2022 and February 2023. The objective of this phase was to develop all the necessary protocols, reporting systems and logistics to ensure that FWHs could efficiently implement an adapted treatment protocol for uncomplicated severe and moderate wasting - using their simplified tools, while providing their community-based caseloads with an uninterrupted supply of ready-to-use therapeutic food (RUTF). This phase of work was also intended to validate a service approach that will be implemented at a larger scale as part of a research study (planned for the end of 2023) looking into the effectiveness of iCCM+ in improving wasting treatment coverage in a wider geographical area in Somaliland. |
The treatment approach and service continuum
The iCCM+ treatment protocol was developed by adapting traditional wasting treatment with the information gained from several rounds of user-centred design efforts. The protocol consisted of three steps (below) and FHWs were provided with monthly in-person support/training from MoHD supervisors.
Step 1
Screening at the child’s home using a simplified mid upper arm circumference (MUAC) tape, checking for oedema and using the ‘nutrition tally register’, and assessing for danger signs. The simplified MUAC tape used existing measurement increments for severe and moderate wasting, but replaced the numbers and measurement increments with five colour-coded sections. These colour codes were featured throughout the suite of simplified tools – enabling low-literacy/numeracy cadres to effectively deliver iCCM+ services, thus expanding access.
Step 2
Admission, treatment, and counselling at the FHW’s home (using malnutrition registers); providing routine medications and a modified biweekly RUTF dose for moderate or severe wasting (one or two sachets/day); and nutrition counselling. The FHW recorded key information about the child’s assessment, treatment, and actions taken in a modified treatment register.
Step 3
Follow-ups occurred during weekly FHW visits to the child’s household. Caregivers brought their children to the FHW’s home every two weeks for an additional progress assessment. If the child did not show any danger signs, the caregiver continued to receive RUTF until the child was discharged or referred. Treatment registers (updated fortnightly) contained an additional pictorial register that supported the FHW to assess if the child’s condition improved, stagnated, or declined. This continued until the child met the discharge criteria.
Data Collection
Data collection for the iCCM+ service prototype used both qualitative and quantitative methods, with different stakeholders managing and executing different roles. DesignHealth was responsible for qualitative research design, data collector training, and leading any iterations to the service experience and iCCM+ tools. Save the Children was responsible for collecting quantitative health outcomes data and managing the development of Kobo Toolbox – a digital, tablet-based tool used for all data collection efforts. Save the Children and its partners at the MoHD also conducted monthly site visits during each home distribution day, during which they reviewed and interviewed FHWs and caregivers. DesignHealth provided remote support and guidance during the service prototype phase by facilitating monthly progress reviews with project implementors.
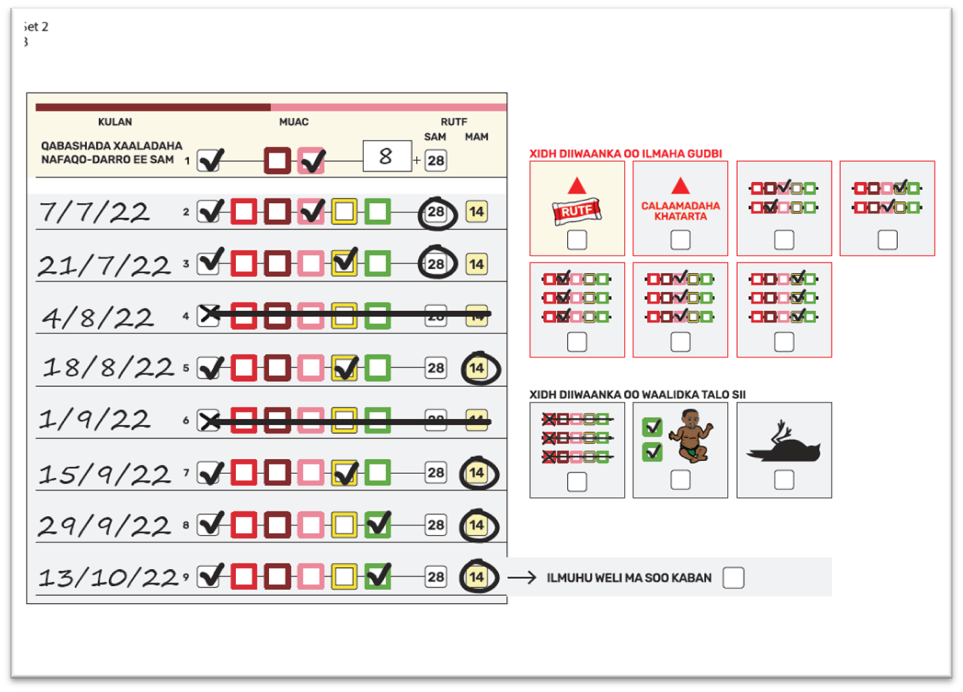
Service launch preparation
In preparation for the service prototype launch, DesignHealth developed a four-day in-person curriculum, instructional design, and training aids for the iCCM+ training of trainers. Heavy emphasis was placed on scenario-based training, requiring students to recognise visual patterns on the treatment register that indicated the child’s progress toward recovery (Figure 1). Save the Children conducted community mobilisations in August 2022 to introduce the iCCM+ service prototype to each community.
Figure 1: An example training scenario2
Measuring tool performance
The iCCM+ tools enabled FHWs to process data and make decisions. FHW errors and omissions were categorised by DesignHealth using patient safety frameworks, with an explicit focus on errors with implications for the child and FHW’s wellbeing.
Findings
Treatment outcomes
Although the main objective of the service prototype phase was not to assess the effectiveness of treatment delivered by FHWs – which will be investigated during the subsequent research phase – specific data related to the user experience, including on the access ”œjourney” of community caregivers and the impact of the additional workload on the FHW, was collected and reviewed during the service prototype phase.
Across the five trained FHWs, 1,203 screenings for malnutrition were conducted during five months of implementation3. In total, 83 children were admitted for moderate wasting, with 38 recoveries and eight defaulters; four children were admitted for severe wasting, with two recoveries and two defaulters.
Tool performance
We observed that some of the modified MUAC tapes had issues with the coloured pigment scratching off after three months of use. This resulted from procuring a small batch of modified tapes that sought to balance costs. For the next phase of work, alternative MUAC tape suppliers will be identified with additional quality checks and sufficient contingency stock in place.
Other iCCM+ tools, such as registers, tally sheets, and job aids, did function as intended – having already been validated through previous usability testing by DesignHealth.
FHW errors
FHW errors that were observed (and corrected by Save the Children and MoHD during the home distribution day) included incorrect MUAC tape application, oedema checks, and delivery of counselling messages.
FHWs still struggled with omissions at various points of data entry. Arguably, the most serious cases involved incorrect documentation of the child’s discharge status. While these issues were observed during the first two months of the service prototype, one instance of an omission of discharge data was observed by the end of the prototype phase. This suggests that monthly follow-up visits and on-site training may improve FHW compliance with the treatment protocol.
Stock management
During the five months of service prototyping, emergency resupply was only used once, in response to an influx of families into the study community due to the regional drought. The emergency resupply protocol maintained a buffer-stock of RUTF and pre-arranged systems to ensure delivery within two days of the FHW or supervisor’s request, ensuring continuity of treatment until the next scheduled resupply.
Water access and use
iCCM+ protocols indicate the importance of having potable water available (for handwashing and drinking) when RUTF is provided to the child. In Somaliland, caregivers and FHWs face a myriad of water access challenges. At the time of the service delivery prototype, water, sanitation, and hygiene (WASH) had not yet been integrated into iCCM+. WASH integration was recommended by DesignHealth and is expected to have a variety of positive benefits, such as mitigating potential drivers of diarrhoea and the occasional caregiver perception that RUTF itself is to blame for their child’s diarrhoea. The latter point, which was documented three times in separate communities, is worth noting as it resulted in a referral being refused because the RUTF (and therefore the FHW) was blamed for causing the diarrhoea.
Lessons Learned
What worked well?
A key benefit to this approach is that caregivers experienced reduced transport time and costs when accessing iCCM+ services from the FHW’s home compared to the health centre.
To increase adherence and acceptability, the home distribution day for RUTF was decided in consultation with caregivers and FHWs. Thursdays were chosen as this was reported to be the least busy day, with travel to the health centre and markets occurring earlier in the week.
Although FHWs reported a higher workload, due to the introduction of wasting treatment in addition to regular iCCM activities, they were willing to provide these additional services during the prototype phase and expressed satisfaction regarding their additional skills.
Overall, FHWs were directly observed to provide good quality treatment according to the iCCM+ protocol when provided appropriate training, tools, and consistent support and direction from supervisors and monthly field visits.
The supply chain system ensured that supplies were available to FHWs and caregivers in sufficient quantity to provide uninterrupted wasting treatment, during the service prototype.
What were the challenges?
Although FHWs were able to provide a good quality of care, there were errors in performing some functions, particularly after the initial introduction of iCCM+. However, errors gradually reduced over time. In future phases of implementation, supportive supervision will be intensified (ideally biweekly for the first three months of implementation), with refresher training every six months.
Caregivers reported challenges when they were referred for additional healthcare that could not be provided by the FHW, including costs and impacts to care for other children in the household. There is a need for further investigation of what additional support for caregivers to attend referrals is feasible within existing systems and resources, with the potential need for additional interventions.
FHWs reported additional water costs and the need for additional WASH infrastructure to deliver wasting treatment alongside iCCM services (e.g., water needed for the appetite test). In the next phase of implementation, support will be provided to FHWs to ensure they can provide safe water as a part of treatment. Limited WASH infrastructure was acknowledged by all project stakeholders and will be addressed for the research implementation phase in late 2023 / early 2024.
FHWs reported increased workload and personal costs for the delivery of services. Further work is required to evaluate FHW compensation and decisions should be responsive to the increased scope of work and personal expenses incurred by FHWs.
RUTF sachets remain critical for treating uncomplicated wasting. Unfortunately, they have become a financial commodity that can be reliably traded for goods, posing a challenge to programme budgets and health outcomes. Strong community engagement and consistent messaging about the purpose of iCCM+ and RUTF is required from all actors, alongside further exploration of the underlying causes of RUTF sachet exchange.
Limitations
While the service prototype was able to adapt to challenges, different problems may occur when such a service is rolled out at a wider scale, in other locations, for a longer period. Reporting bias, particularly related to FHWs’ experience of additional workload and additional tasks, may have been present given that Save the Children and MoHD supervisors were serving as data collectors for the prototype, likely influencing FHW conclusions A neutral third party should survey participating FHWs to gain a more accurate and representative picture.
Conclusion
We recommend the use of ‘user-centred service design’ when initiating a novel service in a new location, which provides functional insights to address operational challenges as they arise.
Overall, the service prototype showed several benefits, including reducing the amount of time and resources that were required by caregivers to access care for their children. The simplified tools enabled FHWs to provide quality care when backed up with proper training and supportive supervision, and the supply system that was developed ensured that RUTF was available to FHWs and caregivers in a timely manner.
The next phase of the work will be the initiation of research evaluating the effectiveness of the iCCM+ approach through cluster randomised control trial, on a larger scale in Somaliland, using the tools and approaches that were validated through the service prototype. Save the Children is also planning to expand the approach into to other locations in Somalia, including those that are more conflict affected, and will try to understand if additional adaptations are required.
For more information, please contact Emily Keane at e.keane@savethechildren.org.uk and Yuusuf Siciid at yuusuf.yuusuf@savethechildren.org.
References
Marron B (2021) Community health worker-led treatment for uncomplicated wasting: Insights from the RISE study. Field Exchange 64. https://www.ennonline.net/fex/64/healthworkersrisestudy
Ministry of Planning and National Development (2020) The Somaliland Health and Demographic Survey 2020. somalia.unfpa.org.
1 DesignHealth is an agency specialising in user-centred design.
2 Students were required to review the simulated register for documentation errors, and then select the appropriate closing icon.
3 Screenings do not represent individual children as the same child may be measured multiple times.


