Kenya: Linking information to action. Synthesis of coverage assessment findings
Lucy Maina Gathigi Nutrition Specialist, Information System, Monitoring & Evaluation, Nutrition Section, UNICEF Kenya Country Office
Charles Mumbi Nutrition Support Officer, Data and Monitoring at the Nutrition Section, UNICEF Kenya Country Office
Lucy Kinyua Monitoring & Evaluation Manager at the Division of Nutrition and Wellbeing, Ministry of Health, Kenya
Ellyn Yakowenko Project Director, Scaling Nutrition at International Rescue Committee (IRC)
Everlyne Adhiambo Nutrition Policy and Research Uptake Advisor at IRC
Shadrack Oiye Public Health Nutrition Specialist at the Intergovernmental Authority on Development (IGAD)
This integrated management of acute malnutrition (IMAM) coverage assessments synthesis was funded by United States Agency for International Development (USAID). The authors recognise the leadership of the Government of Kenya in this work. Special thanks to Veronica Kirogo, Head of Nutrition at the Ministry of Health, and Dr Ismael Teta, Chief of Nutrition at UNICEF Kenya, for their leadership and guidance. Technical inputs from members of the Nutrition Information working group (NITWG) led by Lucy Kinyua and Samuel Murage, as well as the Emergency Nutrition Advisory Committee (ENAC) led by Grace Gichohi, are appreciated. We acknowledge inputs from the UNICEF Kenya Country Office team, including Francis Wambua (Emergency Nutrition Specialist) and Victoria Mwenda (former Nutrition Sector Coordinator), and UNICEF nutrition field teams led by Francis Kidake and Tom Amolo. Special thanks to Edwine Ochieng from the International Centre of Policy and Research Solutions (ICPRS) for his inputs.
The analysis, interpretation, and conclusion reflected in this article are those of the authors. They do not necessarily represent the views of USAID, UNICEF, IGAD, ICPRS, or IRC.
What we know: Since August 2010, Kenya has adopted IMAM programming as part of routine health services. Semi-Quantitative Evaluation of Access and Coverage (SQUEAC) surveys are conducted regularly to provide localised, contextual information on IMAM services.
What this article adds: The need to systematically combine SQUEAC survey results to generate all-inclusive recommendations for improving IMAM coverage across the Arid and Semi-Arid Land counties (ASALs) was recognised. This article explores the synthesis of findings from 18 independent surveys. Most IMAM programmes in ASALs have attained coverage above 50% targets, but there is room for improvement. Key barriers and facilitators are explored and recommendations to improve policy, programmes, and coordination are provided.
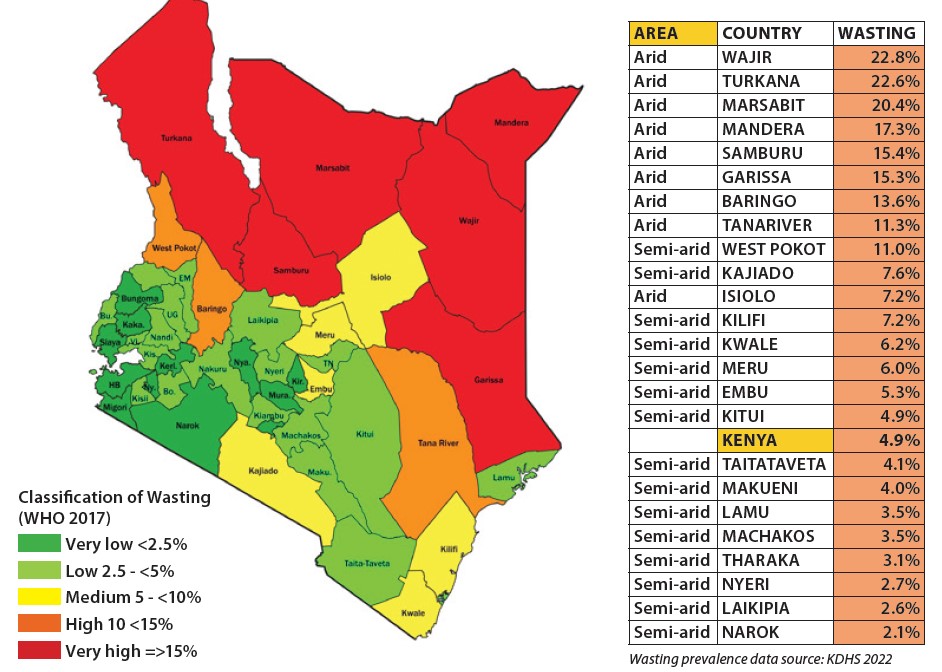
In Kenya, around 5% of children aged under five years are wasted and about 18% stunted (KNBS, 2022). However, the national prevalence of wasting obscures important sub-national patterns – particularly in the ASALs where wasting is generally more prevalent than the national average (Figure 1). The scale-up of IMAM services in the ASALs is a key component of Kenya’s country roadmap toward achieving and sustaining the Global Action Plan targets on wasting. IMAM is implemented by the Ministry of Health in collaboration with UNICEF, the World Food Programme, and implementing partners as part of the emergency nutrition response in the ASALs.
Figure 1: Wasting prevalence in different Kenyan counties
The Kenya Nutrition Information Technical Working Group (NITWG) recognised the need to systematically review localised data, from SQUEAC surveys, to generate all-inclusive recommendations to address key challenges to IMAM coverage across the ASALs. This single, high-level comprehensive outlook could then be used for advocacy, planning, and resource mobilisation, informing the scale-up of IMAM in the ASALs.
Methods
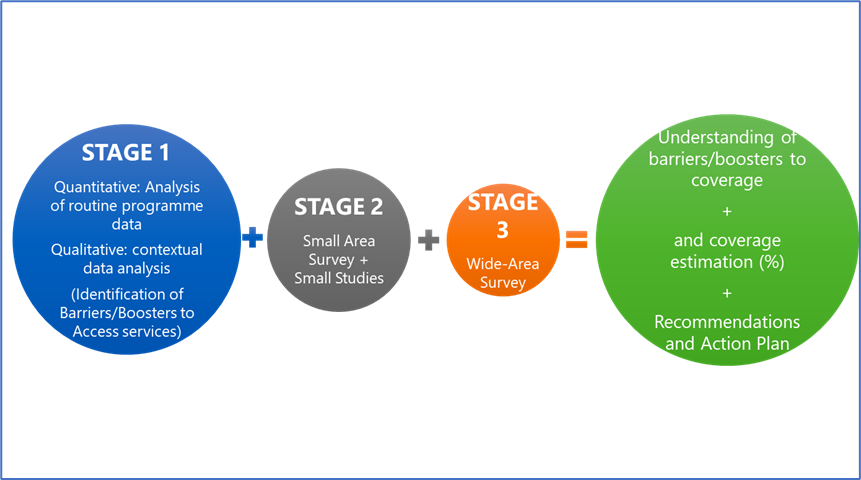
Conducting independent SQUEAC surveys
A total of 18 coverage assessments were conducted between May and July 2023 across 10 ASALs: Turkana, Marsabit, Samburu, West Pokot, Baringo, Isiolo, Tana River, Mandera, Garissa, and Wajir. These assessed Outpatient Therapeutic Programmes (OTPs) and Supplementary Feeding Programmes (SFPs) according to the key steps summarised in Figure 2. In Turkana and Marsabit, six and four separate surveys were conducted at the sub-county level, respectively. This was due to the geographical expansiveness of these counties.
Figure 2 : Key steps used to conduct SQUEAC surveys in Kenya
Synthesis of SQUEAC surveys
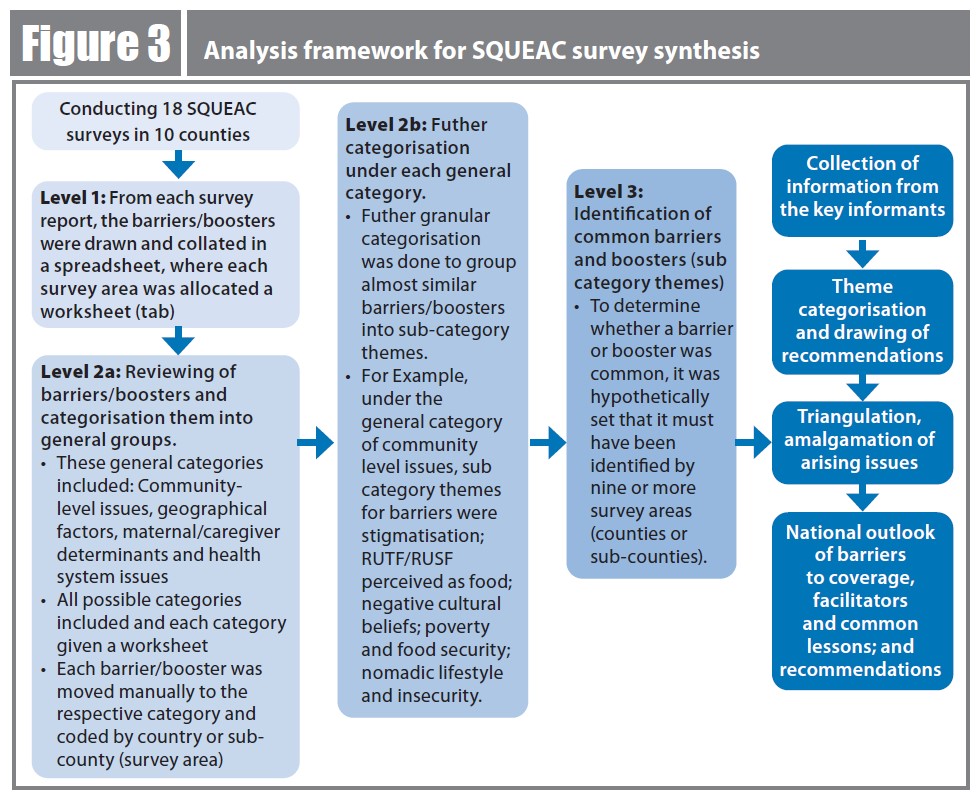
We conducted a ‘quasi’ meta-analysis that collated the results of the 18 SQUEAC surveys. First, the single coverage estimates for either programme (OTP or SFP) were compiled for comparison. From each survey area, coverage barriers and facilitators were collated into an Excel worksheet. Each survey area was allocated a separate worksheet. This was the ‘level one’ analysis of OTP/SFP barriers/facilitators.
In ‘level two’, barriers and facilitators were reviewed and categorised into four general groups: community-level issues, geographical factors, caregiver determinants, and health system issues. The barriers and facilitators that were similar in each of the general groups were further organised into more granular sub-category themes. Sub-categories were then coded in a drop-down menu for ease in enumerating which survey areas reported which barriers and/or facilitators. This allowed us to determine the number of survey areas that reported each sub-category. Our threshold for determining whether a barrier or facilitator (sub-category) was common was that it must have been reported by nine (50%) or more survey areas (counties or sub-counties).
Key informant interviews were also conducted to draw on a broader perspective and to complement county-specific issues. Purposively selected national-level interviewees included: the Ministry of Health National Manager for Emergency Nutrition (n=1), the Ministry of Health Monitoring and Evaluation Manager (1), national staff of implementing partners supporting IMAM (4), the UNICEF Monitoring & Evaluation Specialist (1), the Nutrition Sector Coordinator (1), the UNICEF Emergency Nutrition Specialist (1), nutrition supply chain officers (2), national-level World Food Programme staff (1), the UNICEF Data and Monitoring Nutrition Support Officer (1), and UNICEF Nutrition Specialists at zonal level (2). Guide questions for the key informant interviews were drafted and distributed appropriately across these key informants. This gathered additional information about IMAM coverage that may not have been addressed through the SQUEAC survey methodology alone.
The information collected from key informants was categorised into common themes. These were then triangulated with the synthesised barriers and facilitators to inform the national outlook of issues affecting IMAM programming in Kenya’s ASAL areas (Figure 3).
Figure 3: Analysis framework for SQUEAC survey synthesis
Results
Programme coverage
There were seven OTP and five SFP survey areas that reported single coverage estimates of less than the 50% minimum standard for rural areas (Figure 4) (Sphere, 2018). When SFP and OTP coverage and wasting data were merged, and regression analysis performed, a positive relationship was observed – coverage increased in line with increasing wasting rates. Almost two in every three survey areas (64%) with high wasting rates (over 15%) had higher coverage rates (greater than 50%) for both OTP and SFP. From the synthesis, we noted that areas with higher wasting prevalence also had many nutrition partners supporting IMAM programming, thus explaining the higher coverage estimates. However, this did not come into play for areas with high levels of insecurity (such as Samburu and Laisamis).
Figure 4: Single coverage estimates for outpatient and supplementary feeding programmes compared to observed wasting prevalence a,b
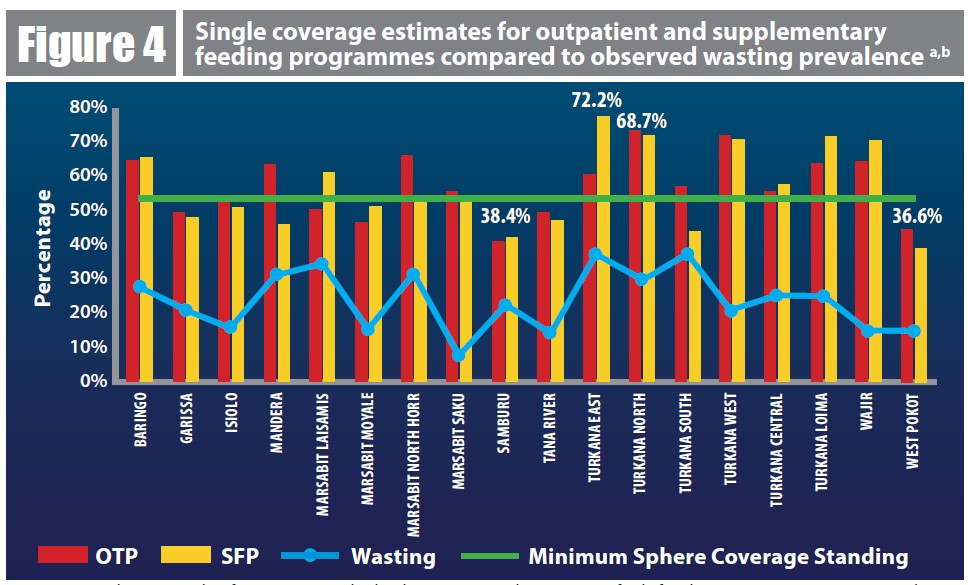
a Wasting prevalence was taken from recent Standardised Monitoring and Assessment of Relief and Transitions (SMART) surveys (July 2022 or January 2023).
b In Turkana and Marsabit counties, sub-counties were assessed separately due to the expansiveness of these areas. Highest and lowest coverages are labelled.
Common barriers to coverage and treatment
In both OTPs and SFPs, 94% of survey areas reported the sharing of ready-to-use therapeutic food (RUTF) or ready-to-use supplementary food (RUSF) – or exchanging them for money or food – as a major barrier (Table 1). Similar findings were reported by key informants, who noted nutrition commodity sharing was commonplace. Some caregivers who consumed alcohol would also exchange RUTF for money or alcohol. Maternal workload was also highlighted as a key barrier, as well as poor active case finding and referral. Long distances to health facilities and migration (due to drought or floods) were also important barriers to access.
Table 1: Barriers and facilitators to outpatient and supplementary feeding programme coveragea
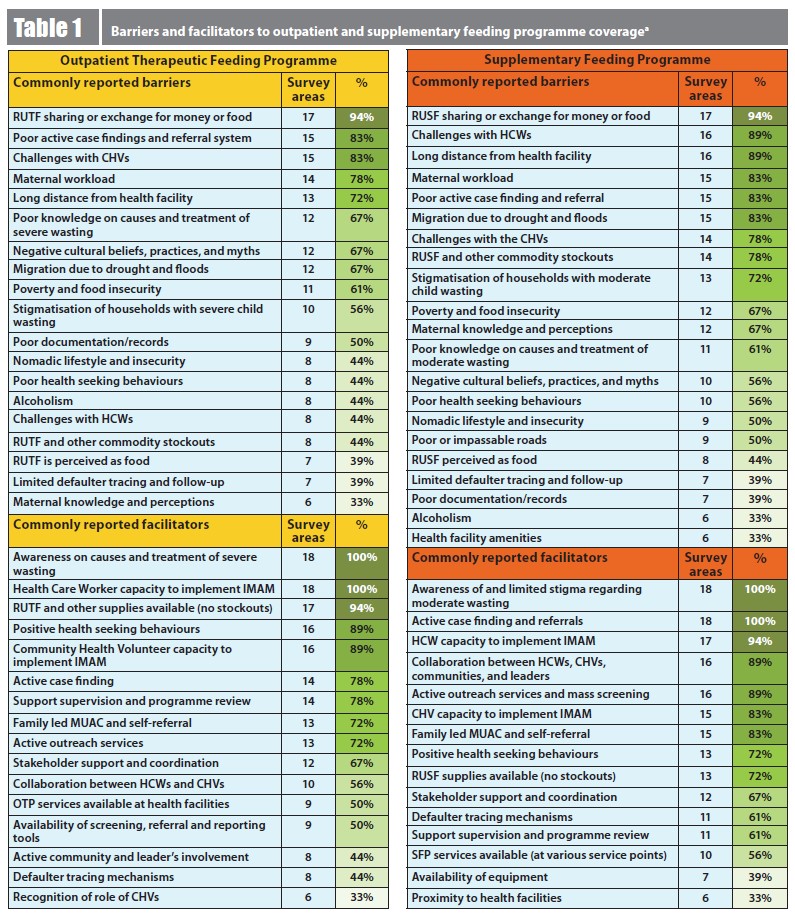
a Only commonly reported barriers / facilitators have been shown here (i.e. those reported in six or more survey areas)
RUTF/RUSF = Ready-to-use therapeutic/supplementary food
CHV = Community Health Volunteer
HCW = Health Care Worker
MUAC = Mid-upper arm circumference
Kenya’s community health strategy was launched in 2006 to improve community access to healthcare. Since then, most counties have adopted it – including all the survey areas featured in this article. However, continued challenges were observed in regard to the community health strategy. In some areas, there were no community health volunteers (CHVs). Where they existed, numbers were often not adequate to support in active case finding, defaulter tracing, and referral. Some CHVs had capacity gaps, as was reported by a partner staff key informant.
“Knowledge of IMAM by CHVs has enhanced screening and active case finding in the community. However, a good number of CHVs have not been trained on IMAM due to limited resources” – Key informant, nutrition partner
Demotivation, due to a lack of or a delayed stipend, was commonly reported for CHVs across the survey areas. We also observed that a barrier may have a geographical aspect due to geopolitical and sociocultural similarities. An example is maternal alcoholism, which was reported in Turkana Central, Turkana South, Turkana West, Samburu, West Pokot, Baringo, Laisamis, and North Horr. These areas border each other, and this finding calls for inter-county collaboration in addressing the challenge.
Common facilitators of coverage
Most health systems facilitators were common across the survey areas for both OTPs and SFPs. These included HCWs and CHVs’ availability and their capacity to provide IMAM services, active case finding, active outreaches, and mass screening exercises. Also important were no stock-out of nutrition commodities, provision of supportive supervision and programme reviews. All the surveyed areas indicated awareness of the causes and treatment of severe and moderate wasting as a key community-level facilitator.
Common maternal/caregiver facilitators identified were positive health seeking behaviour, training caregivers to identify early signs of malnutrition in their children using MUAC (“Family-led MUAC”) and self-referral. Only Turkana North reported availability of active mother support groups as a facilitator.
What next?
The synthesis of findings from the independent surveys, together with the consolidation of insights from key informants, highlight actions to be considered to scale up IMAM across Kenya’s ASALs.
Policy and strategy considerations
Developing and implementing a national strategy for peace, security, development, and humanitarian operations, as well as tackling poverty and infrastructural challenges, all remain important. Poverty and childhood malnutrition are interlinked – and they are mediated by inadequate diets, lower education, poorer living standards, and limited access to healthcare facilities and appropriate water, sanitation, and hygiene. This clearly articulates the need for policies and guidelines that prioritise overall poverty and malnutrition reduction.
Kenya has chosen the primary healthcare system to deliver universal health coverage. A ‘community health strategy’ has been given prominence in all the survey areas. However, challenges to full strategy implementation still exist, as only two counties are reported to be giving CHVs a monthly stipend. There is a need for county governments to collaborate with partners to develop and implement community health acts. These acts will provide a legal basis for counties to allocate funds for renumeration and provide adequate supervision of CHVs. This will result in CHVs who are better motivated, better equipped, and who are accountable when providing health services at community level.
Programmatic issues
Across 18 independent SQUEAC surveys, with a few exceptions (Turkana East, Turkana Loima, and Wajir), the OTP was found to perform better in both coverage and outcome indicators than the SFP. This is despite both programmes being implemented jointly in all the survey areas. This calls for further analysis to understand the associations and unique factors that could be causing this difference.
Maternal workload was highlighted as a key caregiver barrier. Programming should be designed to encompass male involvement in childcare activities and not purely focus on mothers and children. Counties and partners could also support establishing peer-to-peer support groups for fathers at community level, which have been proven to positively influence child feeding practices (Bogale et al, 2022; Atuman et al, 2023). Fathers can be involved in financial and resource support, as well as social and physical support, such as shared responsibility for the nutritional wellbeing and health of the child. A study in Ethiopia found that, for children aged 6–23 months, dietary diversity in the household increased by 13.7% when fathers were involved in infant and young child feeding (Gebremedhin et al, 2017).
Community engagement, sensitisation, and mobilisation clearly remain as barriers to increasing coverage for both OTPs and SFPs. Addressing these issues will be central to achieving greater coverage in IMAM programmes. As well as developing guidelines and strategy documents, it is critical for counties and partners to allocate resources for improved community engagement.
The sharing and commodification of RUTF/RUSF was a major barrier. This directly affects programme outcomes, increasing both length of stay and non-response in a programme. Ultimately, children who remain wasted remain at heightened risk of mortality and morbidity associated with malnutrition. Such practices also increase the cost of programmes. To curb this, it is critical to link households with malnourished children who have exited as ‘cured’ from IMAM programmes to social safety net schemes. However, in this analysis, only two survey zones reported the availability of social safety net programmes as a facilitator. National and county governments, and partners, must scale up social safety net and poverty alleviation programmes that integrate nutrition.
The adequacy and availability of nutrition supplies was a key facilitator leading to the success of the IMAM programme. Although the supply chain is government led, procurement is heavily supported by donors. Advocacy efforts should continue at both the national and county levels for resource allocation to cover nutrition supplies and for ring-fencing finances to protect any allocated funding for this task.
Coordination actions
Several coordination mechanisms for nutrition exist in the country at national level, providing opportunities for collaboration and to strengthen partnerships between the Ministry of Health and nutrition stakeholders. These include the Nutrition Technical Forum, ENAC, and NITWG. Counties could establish such coordination structures for inter-county information sharing and collaboration, seeking to address common barriers and documenting best working practices.
Conclusion
This systematic synthesis of findings from 18 SQUEAC surveys highlighted that most IMAM programmes in ASALs have attained OTP and SFP single coverage above 50% but there is room for improvement and a need to sustain the gains already made. OTP was noted to perform better compared to SFP.
The identified common barriers and facilitators, and additional key observations, provide relevant information for policy, advocacy, and programmatic efforts to scale up the management of wasting across the ASALs. Moreover, the synthesis diagnoses the need for inter-county collaboration in tackling specific barriers, given their geographical spread. Ultimately, systems need to be strengthened to prevent children from becoming wasted in the first place. Poverty alleviation, stronger community systems, and gender equity (all advocated for above) will not only reduce barriers to increasing treatment coverage but also promote prevention.
For more information, please contact Lucy Maina at lmaina@unicef.org
References
Atuman S, Langat O, Iellamo A et al (2023) Father-to-father support groups in northern Nigeria: An emergency response initiative. Field Exchange 70. https://www.ennonline.net/fex/70/father-to-father-support-groups-in-northern-nigeria
Bogale S, Cherie N & Bogale E (2022) Fathers’ involvement in child feeding and its associated factors among fathers having children aged 6 to 24 months in Antsokia Gemza Woreda, Ethiopia: Cross-sectional study. PLoS One, 17, 11, e0276565
Gebremedhin S, Baye K, Bekele T et al (2017) Predictors of dietary diversity in children ages 6 to 23 months in a largely food-insecure area of South Wollo, Ethiopia. Nutrition, 33, 163–8
KNBS (2023) Kenya demographic and health survey 2022 – Key indicators report. dhsprogram.com
Sphere (2018) Humanitarian charter and minimum standards in humanitarian response. spherestandards.org
About This Article
Jump to section
Download & Citation
Reference this page
Lucy Maina Gathigi, Charles Mumbi, Lucy Kinyua, Ellyn Yakowenko, Everlyne Adhiambo and Shadrack Oiye (2024). Kenya: Linking information to action. Synthesis of coverage assessment findings. Field Exchange issue 72. https://doi.org/10.71744/5sv2-qd20


 English
English Français
Français Deutsch
Deutsch Italiano
Italiano Español
Español