Trialling a multi-MUAC tape to screen at-risk infants under six months in East Africa
Eilise Brennan Nutrition Technical Officer at GOAL Global
Amir Samnani Nutritionist at Emergency Nutrition Network (ENN)
Hatty Barthorp Nutrition Advisor at GOAL Global
Alice Burrell Senior Humanitarian Nutrition Advisor (MAMI) at Save the Children
Fabrizio Loddo Senior Humanitarian Nutrition Advisor at Save the Children
Angelina Nasira Boi Former MAMI Coordinator at MOMENTUM Integrated Health Resilience (MIHR), IMA World Health South Sudan, an affiliate of Corus International South Sudan
Marlene Traore-Hebie Senior Technical Advisor for Nutrition at MIHR, Corus International, USA
Nicky Dent MAMI Global Network Coordinator at ENN
Marie McGrath Technical Director at ENN
We would like to express our deepest gratitude to the country offices and the dedicated health workers at the MAMI sites for providing exceptional care to at-risk mother–infant pairs, and the unwavering commitment of the mothers that made this multi-MUAC pilot possible. We would like to acknowledge the ministries of health in South Sudan, Ethiopia, Kenya, and Somalia, as well as MIHR MAMI International Consultant Hedwig Deconinck. We also extend our sincere thanks to ECHO, the Bill & Melinda Gates Foundation, the Department of Foreign Affairs Ireland, BHA, USAID, and Latter Day Saints Charities, who supported this research.
What we know: There is building evidence that mid-upper-arm circumference (MUAC) is a reliable tool and a good predictor of mortality in infants aged under six months (Hoehn et al, 2021). However, practitioners have faced challenges in accessing and producing tapes for research and programming.
What this adds: Operational pilots by GOAL, Save the Children, and MIHR of a prototype multi-MUAC tape found that healthcare workers (HWs) and caregivers in Somalia, Kenya, and South Sudan could effectively and feasibly use it to screen infants under six months of age. Recommendations for design improvements and contextual influences have informed an updated World Health Organization (WHO) and UNICEF MUAC tape for women and infants (aged six weeks to six months), which is now available from UNICEF regional and country offices.
The ‘management of small and nutritionally at-risk infants under six months and their mothers’ approach (MAMI) refers to the continuity of respectful quality care for at-risk mother–infant pairs across systems of health and nutrition. ‘At-risk’ or vulnerable pairs include infants and mothers who may be identified in many ways. They include infants born too early (preterm) or too small (low birth weight), infants who are wasted, underweight, or growing poorly, and mothers with nutrition, mental/physical health, and social problems (McGrath et al, 2024).
Since 2019, MUAC has been used in infants aged under six months in a limited number of settings, building valuable evidence of its application in this age group. These efforts have contributed to a recommendation on the use of MUAC to identify infants at risk of poor growth and development (MUAC <110mm, infants aged six weeks to six months) in the 2023 guideline on the prevention and management of wasting and nutritional oedema (WHO, 2023).
In 2022, a working group was convened by the MAMI Global Network to address challenges in accessing or producing a quality MUAC tape for use with infants. This was a time-sensitive challenge given imminent opportunities to include MUAC for infants aged under six months in research, and the potential for a WHO recommendation to emerge. While a MUAC template for infants aged under six months was available (Rana et al, 2021a), in-country replication was proving difficult to the necessary specifications.
The working group oversaw the design of a pilot ‘multi-MUAC’ tape, produced for research purposes by UNICEF in collaboration with WHO. The aim was to produce a practical, high-specification MUAC tape that was designed to assess infants aged under six months, while also incorporating mother’s assessment alongside. The tape also included children aged 6–59 months to avoid the need for multiple different MUAC tapes.
The multi-MUAC tape was piloted by three agencies (GOAL, Save the Children, and MIHR) to test its feasibility and effectiveness for screening infants aged under six months by HWs and caregivers. This article shares the collated findings of this collective effort.
Methods
Design and production
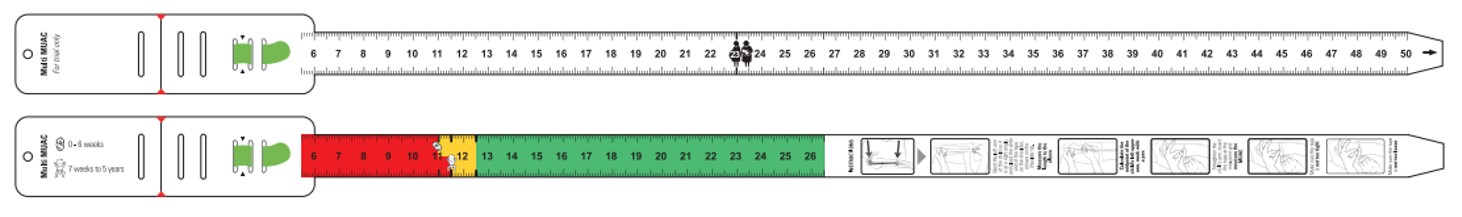
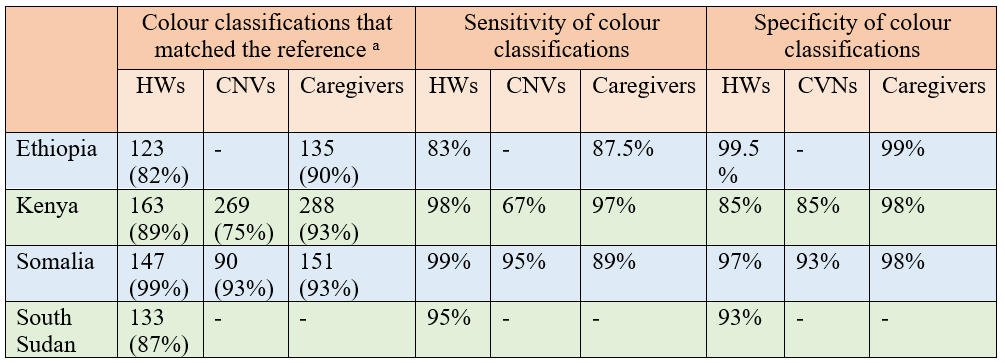
The multi-MUAC tape design (figure 1) was developed by the working group using the GOAL template as a strong starting point. One side measures infants and children (mm, colour-coded), while the other measures women (mm only). At the time of development there were no guidelines for the use of MUAC in infants. To identify infants at heightened risk of malnutrition requiring referral for further assessment and support, we used <110mm (infants aged 0–6 weeks) and <115mm (aged seven weeks and above). Infants above these cut-offs and <125 mm were still considered to be at risk of deteriorating nutritional status and referred to community HWs for additional counselling and support. The material thickness of the multi-MUAC tape was adjusted to address problems with the UNICEF MUAC tape for children aged 6–59 months (Rana et al, 2021b). The tape design was managed by UNICEF Supplies Division and a limited number were rapidly produced for research purposes only.
Figure 1: ‘Multi-MUAC’ tape design
Operational pilots
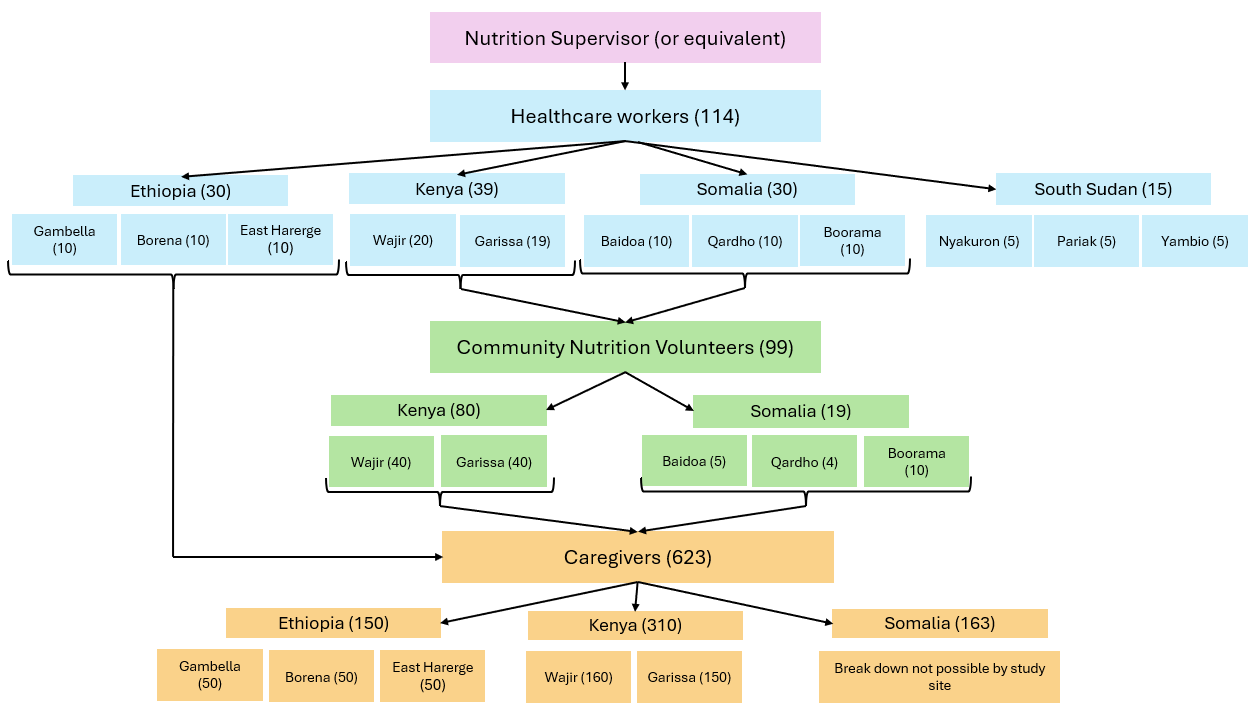
GOAL developed a study protocol that informed the basis for the operational pilots, adapted to each country’s context and capacity. In Ethiopia, GOAL tested the tape with HWs and caregivers in three study sites (figure 2). Save the Children tested the tape with HWs, caregivers, and community nutrition volunteers (CNVs) – community members who receive brief training on health and nutrition – in two study sites in Kenya and three in Somalia. In South Sudan, MIHR tested the tape with HWs in three study sites. Training on the use of the multi-MUAC tape varied by setting but in general was cascaded from nutrition supervisors (or equivalent) to the different HW cadres and caregivers.
Figure 2: Number of participants trained at each study site
Data collection
Data was collected over various time periods between December 2022 and July 2023. While all infants included in the pilots were aged under six months, the exact age of the infant at the time of assessment was not recorded. Information on measurement accuracy, which side of the tape was preferred, and any challenges in tape usage were collected from study participants. Information on preferred side of the tape was not collected in South Sudan, but recommendations for future development of the tape were gathered.
In Ethiopia, Kenya, and Somalia, HWs measured five infants each. In South Sudan, 10 infants were measured by each HW. Across the study sites, verification measurements were taken by the Nutrition Supervisor (or equivalent) on the same infants. In Kenya and Somalia, CNVs measured five infants each, with verification measurements taken by HWs on the same infants. Caregivers measured their own infant’s MUAC using the colour classification only, which was compared to measurements taken by HWs (Ethiopia) or CNVs (Somalia, Kenya).
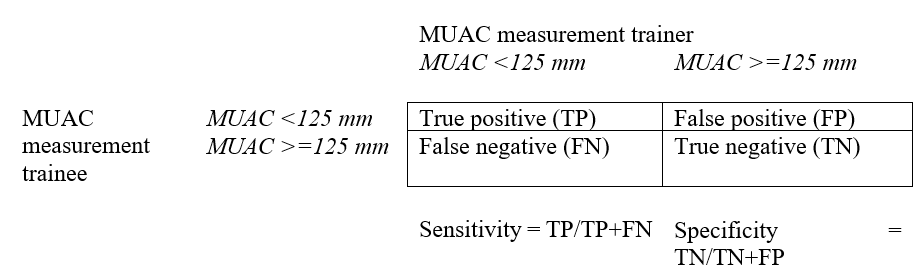
Data analysis
To assess performance, absolute numeric MUAC measurements and risk classifications by colour were compared (HWs vs nutrition supervisors, CNVs vs HWs, and caregivers vs HWs/CNVs). For numeric MUAC measurements, a standard of error of +/- 1mm was applied across study sites. We also calculated the sensitivity and specificity of numeric MUAC measurements and risk classifications by colour using a MUAC cut-off of 125 mm (Figure 3).
Figure 3: Calculating the sensitivity and specificity of measurements
Findings
Accuracy of MUAC measurements
Apart from in Kenya, over 70% of HWs and CNVs were able to correctly measure the infant’s numeric MUAC value to within 1mm, compared to measurements taken by trainers on the same infant. There was high specificity of numeric MUAC measurements by HWs and CNVs across all countries. Apart from CNVs in Kenya, there was high sensitivity of numeric MUAC measurements by HWs and CNVs.
Table 1: Multi-MUAC measurement accuracy (>=125mm) by participant
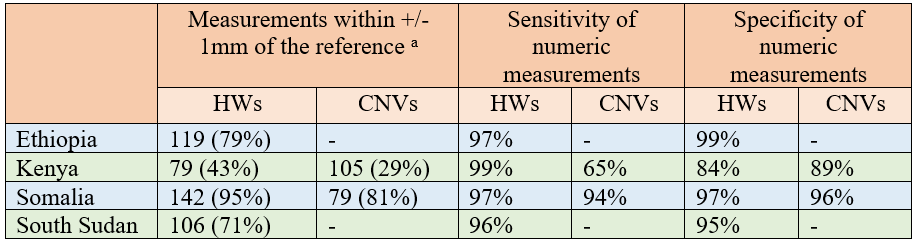
a Reference = Measurement taken by a trainer on the same infant
Healthcare workers (HWs); Community nutrition volunteers (CNVs)
A higher percentage of HWs and CNVs were able to correctly identify infants' risk classification using colour coding compared to numeric MUAC measurements. Similarly, a high percentage of caregivers were able to correctly identify the risk classification by colour (table 2). Across all countries, there was high sensitivity and specificity of risk classifications by colour for HWs, CNVs, and caregivers.
Table 2: Risk classification (by colour) accuracy arranged by participant
a Reference = Measurement taken by a trainer on the same infant
Healthcare workers (HWs); Community nutrition volunteers (CNVs)
Challenges using the multi-MUAC tape
HWs reported some challenges in reading the tape (table 3) due to the small font size of measurements, the window of the tape being too narrow (making the measurements difficult to read), and the infants wriggling during assessment. CNVs in Kenya reported challenges in reading and interpreting the tapes due to low literacy rates, coupled with small text size. Training also greatly varied between study sites. Response rates were low for questions on challenges (4–16%), so these results should be interpreted carefully.
The South Sudan MAMI team identified design problems with the women’s tape side that confused interpretation: specifically, the placement of the breastfeeding mother image alongside the 235 mm measurement point implied to some that this was the cut-off to apply to breastfeeding mothers (rather than 230mm). While measurements were recorded in millimetres they were presented on the tape in centimetres, which also caused confusion. The length of the tape was reported as too long and inconvenient when measuring very young infants.
When asked which side of the tape they preferred, 79% of HWs and 59% of CNVs who responded found the coloured side of the tape (the child side) easier to use. However, the response rate was also low for this question (26% HWs, 31% CNVs).
Table 3: Reported challenges in multi-MUAC tape usage
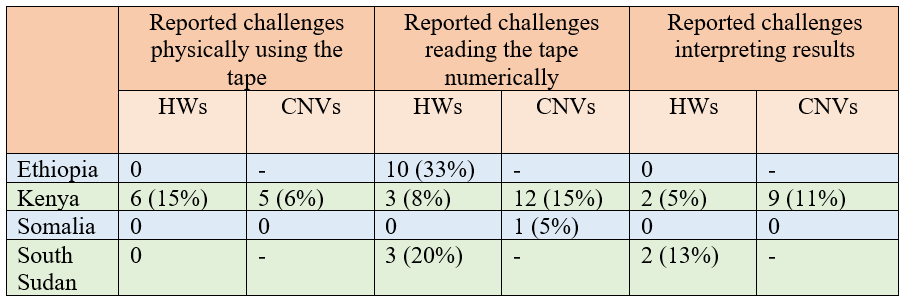
Healthcare workers (HWs); Community nutrition volunteers (CNVs)
In Somalia and the Garissa region in Kenya, data on the challenges in using the tapes in infants were reported per group of caregivers (not individuals). Caregivers reported difficulties in using the tape in Wajir (Kenya) (32% of caregivers), Garissa (Kenya) (13% of groups), and Ethiopia (19% of caregivers). Caregivers reported challenges in reading / interpreting the results in Wajir (21% / 37% of caregivers), Garissa (20% / 13% of groups), and Somalia (6% / 3% of groups), respectively. A range of challenges in physically using the tape were reported by caregivers, such as in estimating the midpoint of the infant’s arm, measuring small infants due to crying and wriggling, and confusion on how to lace the tape correctly through the windows.
Suggestions to improve the MUAC tape
The respondents highlighted several design changes that could improve the multi-MUAC tape. These included increasing the font size of measurements, colour coding both sides, and reducing the number of windows through which the tape is laced. The MUAC design team recognise that three windows through which to lace the tape is greater than many traditional MUAC tapes, but this was done to reduce the lateral movement of the tape and reduce measurement inaccuracies more common with a single window design. Respondents also suggested using millimetres on the tape (to improve accuracy and precision), reducing tape length, and improving tape durability (in reference to the colouring fading quickly). One team suggested moving the pregnant and breastfeeding women images to the head of the tape to avoid confusion. To improve legibility, including colour coding only in the middle of the tape was also suggested.
Respondents were eager to ensure that cut-offs are adjusted to align with specific contexts and national protocols (e.g. cut-offs for women should align with admission criteria for supplementary food programmes where operational). Using ‘0–6 weeks’ and ‘seven weeks and above’ as classification descriptors was noted as inconsistent with both the MAMI Care Pathway (which uses ‘infants under six weeks’ and ‘infants six weeks to six months’) and the latest WHO recommendation (‘six weeks and above’).
Discussion and conclusions
As the studies were opportunistically implemented by different agencies at different operational settings, implementation varied between study sites. Qualitative data and discussions with the implementing teams indicated considerable variation in training and delivery modality. There was also considerable variability in the quality of data collection, with a large amount of missing data for qualitative findings from Somalia and Kenya. Results should therefore be interpreted carefully.
Our findings indicate that the majority of HWs, CNVs, and caregivers could feasibly and effectively use the multi-MUAC tape to screen infants aged under six months, to varying degrees. Caregivers found the tape most challenging to use and interpret, followed by CNVs, and then HWs. Several factors affected the usability of the piloted tape: some of these were specific to the tape design, and some not. Our experience emphasises that while the tool itself may be simple, contextualised training and support will be important for practice.
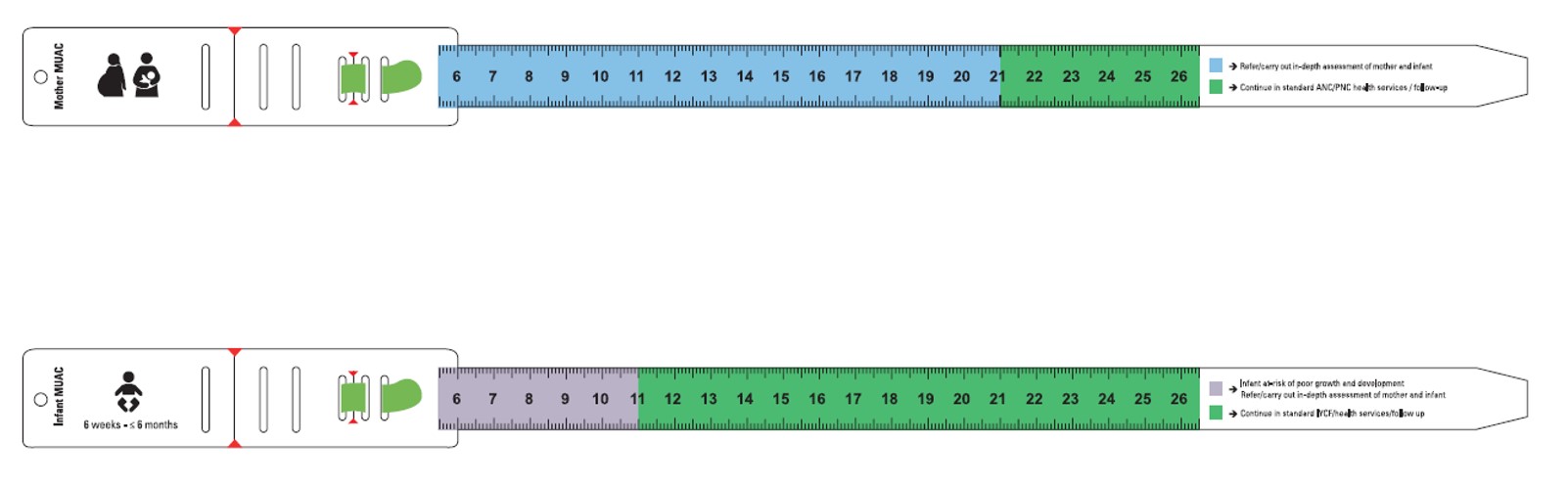
The multi-MUAC tape was developed as a first-step test prototype, anticipating it would likely need amending and adaptation to contexts. Our findings have been shared and they informed a subsequent version that has been co-developed and produced by UNICEF and WHO under the Wasting and Nutritional Oedema (Acute Malnutrition) Technical Advisory Group (Infants Sub-Working Group) (WHO, 2024). This version only includes infant MUAC cut-offs for those aged six weeks and over, for consistency with the 2023 recommendation (WHO, 2023). There are two versions with 21cm or 23cm cut-offs for pregnant women/mothers (figure 4).
Figure 4: Mother/infant MUAC tapes available from UNICEF
Version 1 (23cm cut-off):
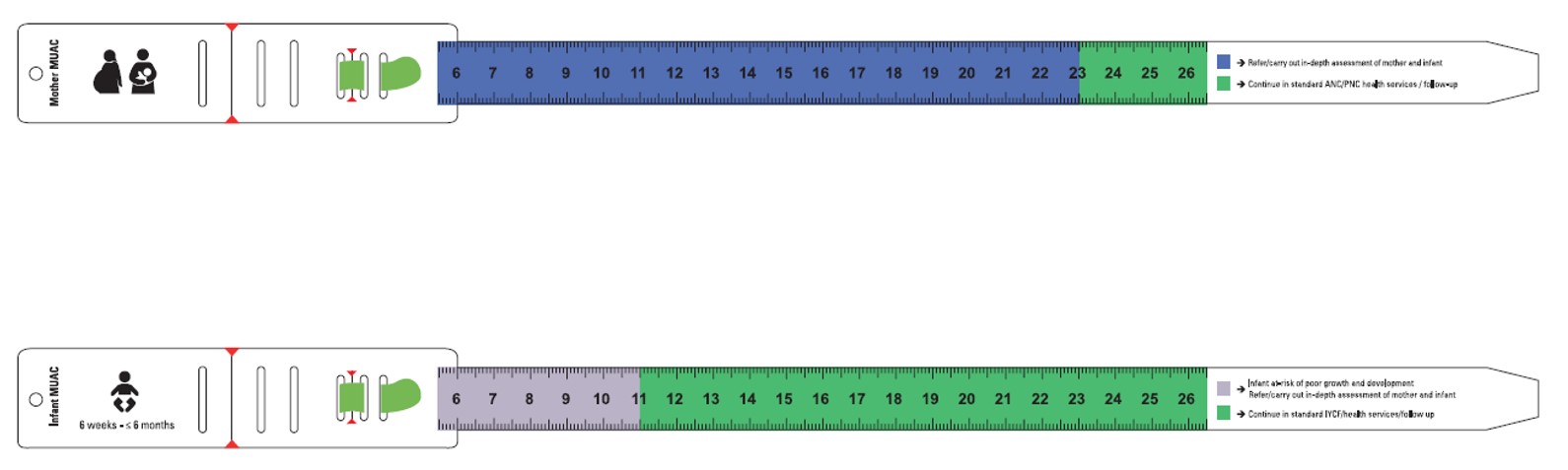
Version 2 (21cm cut-off):
For more information, please contact Eilise Brennan at ebrennan@goal.ie
To order mother/infant MUAC tapes, please contact UNICEF regional and country offices for supplies, guidance and to provide user feedback.
References
Angood C, McGrath M, Mehta S et al (2015) Research priorities to improve the management of acute malnutrition in infants aged less than six months (MAMI). PLOS Medicine, 12, 4, e1001812
Hoehn C, Lelijveld N, Mwangome M (2021) Anthropometric criteria for identifying infants under 6 months of age at risk of morbidity and mortality: A systematic review. Clinical Medicine Insights: Pediatrics, 15
MAMI Global Network, ENN, LSHTM (2021) MAMI Care Pathway Package, Version 3. www.ennonline.net/mamicarepathway
McGrath M, Wrottesley S, Brennan E (2024) Invisible pursuit: Global policy guidance on care of vulnerable infants under 6 months and their mothers: A scoping review. https://www.ennonline.net/global-policy-guidance-on-care-of-vulnerable-infants-under-six-months-and-their-mothers
Rana R, Barthorp H, Murphy M (2021a) Implementing the family-MUAC approach for infants under 6 months in the context of COVID-19 in Ethiopia. Field Exchange 64. https://www.ennonline.net/fex/64/ethiopiagoalcovidadaptations
Rana R, Barthorp H, McGrath M et al (2021b) Mid-upper arm circumference tapes and measurement discrepancies: Time to standardize product specifications and reporting. Global Health, Science and Practice, 9, 4,1011–1014
WHO (2023) WHO guideline on the prevention and management of wasting and nutritional oedema (acute malnutrition) in infants and children under 5 years: Web annex A: Guideline questions and outcomes. iris.who.int
WHO (2024) UNICEF/WHO technical advisory group on wasting and nutritional oedema (acute malnutrition) – members and secretariat. who.int
About This Article
Jump to section
Download & Citation
Reference this page
Eilise Brennan, Amir Samnani, Hatty Barthorp, Alice Burrell, Fabrizio Loddo, Angelina Nasira Boi, Marlene Traore-Hebie, Nicky Dent and Marie McGrath (2024). Trialling a multi-MUAC tape to screen at-risk infants under six months in East Africa. Field Exchange 73. https://doi.org/10.71744/4jp7-gw75


